About 73% of healthcare organizations keep using legacy systems for their clinical operations. This reliance often comes at a significant cost associated with continuously maintaining outdated technology. More critically, outdated systems can become the cause of limited healthcare software functionality and pose the risk of losing sensitive medical data.
If you recognize the need to modernize your clinic’s outdated EHR or other systems to maintain operational efficiency and patient care quality, this article is for you. You’ll discover the common challenges that arise during the modernization process, tips to overcome them, ways to tackle popular upgrade mistakes, and steps to conduct a legacy system modernization smoothly and efficiently.
Top Reasons for Legacy Software Modernization in Healthcare
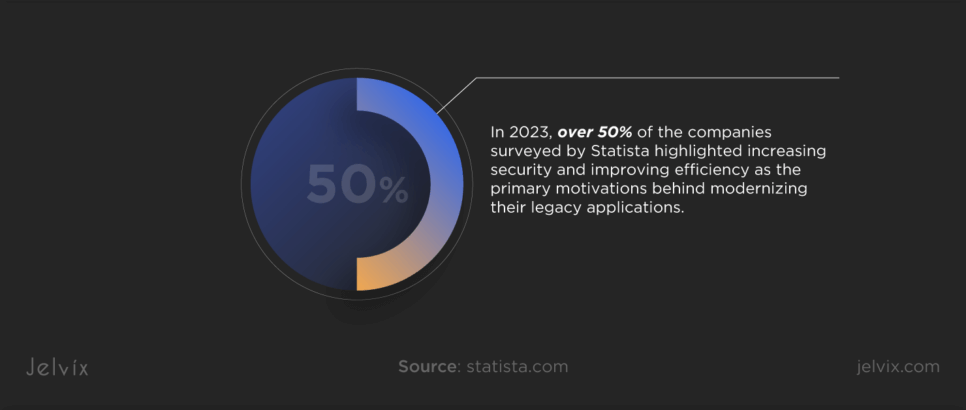
Many medical companies have started seeing modernization as a strategic step aimed at improving the quality of care, organizing clinical processes, and complying with changing industry standards. In 2023, over 50% of the companies surveyed by Statista highlighted increasing security and improving efficiency as the primary motivations behind modernizing their legacy applications. Nearly half also cited cost reduction, better integration with modern technologies, and the desire for increased flexibility as significant drivers.
Boosting Productivity
Legacy systems often involve slow and outdated processes that limit operational efficiency. Modernization helps make clinical workflows more efficient by automating repetitive tasks and minimizing manual entry errors. As a result, clinicians become more productive and attentive during patient care.
Ensuring Data Security
As cyber threats grow more sophisticated, the vulnerabilities in legacy systems pose significant risks to sensitive patient data. Modernizing these systems introduces robust security protocols and measures that can help safeguard against breaches and data leaks.
Improving Patient Care
Upgraded systems provide a holistic approach to patient management, offering advanced tools for record-keeping, telehealth services, and AI-driven insights. This enhances patient outcomes through more accurate diagnoses, personalized care plans, and data-proofed treatment processes.
Enhancing Interoperability
Legacy systems often lead to data silos, preventing the seamless exchange of patient information. Modern systems are designed with interoperability in mind, facilitating easy sharing across healthcare settings, which is crucial for coordinated patient care.
Achieving Cost Efficiency
While modernization requires initial investment, it can lead to considerable long-term cost savings. Enhanced operational efficiency, reduced system downtime, and decreased reliance on manual processes can result in a significant return on investment.
Maintaining Regulatory Compliance
The healthcare industry is quite dynamic in terms of regulations. Modern healthcare systems are built to adapt to the changes, helping organizations stay compliant with current and future regulatory requirements and avoid potential fines.
Scalability
Legacy systems can limit healthcare organizations’ growth. Modern software solutions offer scalability, making it easier for medical facilities to expand functionalities, manage growing data volumes, and accommodate more users without decreasing clinical performance.
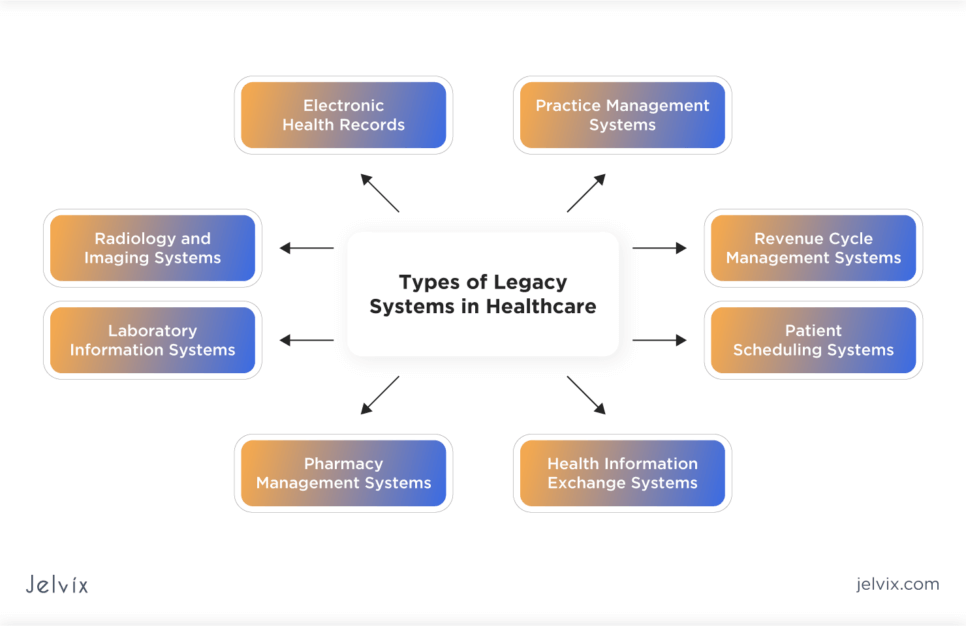
Types of Legacy Systems in Healthcare
Legacy healthcare systems pose challenges due to their outdated technologies and inability to meet the demands of the healthcare industry. Understanding the types of outdated systems can help to plan your modernization efforts properly.
Electronic Health Records
Legacy EHR systems often lack interoperability, making it difficult to share patient data across different healthcare settings or integrate with newer health technologies. They may also be difficult to use, affecting clinical efficiency and patient care.
Practice Management Systems
These systems, designed to manage daily operations such as scheduling, billing, and reporting, can become inefficient over time. Legacy practice management systems may not support electronic billing or fail to integrate with modern EHRs, leading to administrative inefficiencies.
Radiology and Imaging Systems
Outdated radiology and imaging systems, such as PACS (Picture Archiving and Communication Systems), might not support the latest imaging modalities or integrate well with other healthcare systems, complicating the storage, retrieval, and sharing of diagnostic images.
Laboratory Information Systems
Legacy LIS may struggle with integrating with EHR systems or supporting new test technologies, leading to delays in test results, inaccuracies, or inefficiencies in ordering and processing laboratory tests.
Pharmacy Management Systems
Outdated pharmacy management systems may not efficiently manage medication inventories, integrate with EHRs for medication reconciliation, or support electronic prescribing, potentially leading to medication errors and compromising patient care.
Revenue Cycle Management Systems
RCM systems are critical for the financial health of medical organizations. Legacy payment systems may not comply with current billing regulations, support electronic claims processing, or provide efficient revenue cycle management, affecting financial performance and leading to losing revenue.
Patient Scheduling Systems
Older patient scheduling systems may offer limited functionality, lacking features like online appointment booking, automated reminders, or integration with updated clinical workflows, which can lead to scheduling inefficiencies and reduced patient satisfaction.
Health Information Exchange Systems
Legacy HIE systems may lack the capability to support seamless and secure sharing of health information across different healthcare settings, compromising efforts towards coordinated care and population health management.
Explore the benefits and challenges of real-time data entry in healthcare and learn how this innovative approach can optimize patient care and streamline clinical workflows.
Maintaining vs. Replacing Legacy Systems
The choice between replacing or maintaining a legacy system should involve a careful cost-benefit analysis, considering both direct and indirect impacts on clinical workflows, patient care, and staff satisfaction.
The Jelvix team recommends replacing the legacy system if it fails to meet new healthcare standards, incurs high maintenance costs, lacks scalability, offers a poor user experience, or presents security vulnerabilities that can compromise patient data.
Consider maintaining the legacy system if it remains cost-effective, complies with healthcare regulations, satisfies your organizational needs without significant issues, and can be integrated with newer technologies. This approach may be beneficial for short-term cost savings and minimizing disruptions while carefully planning for future upgrades.
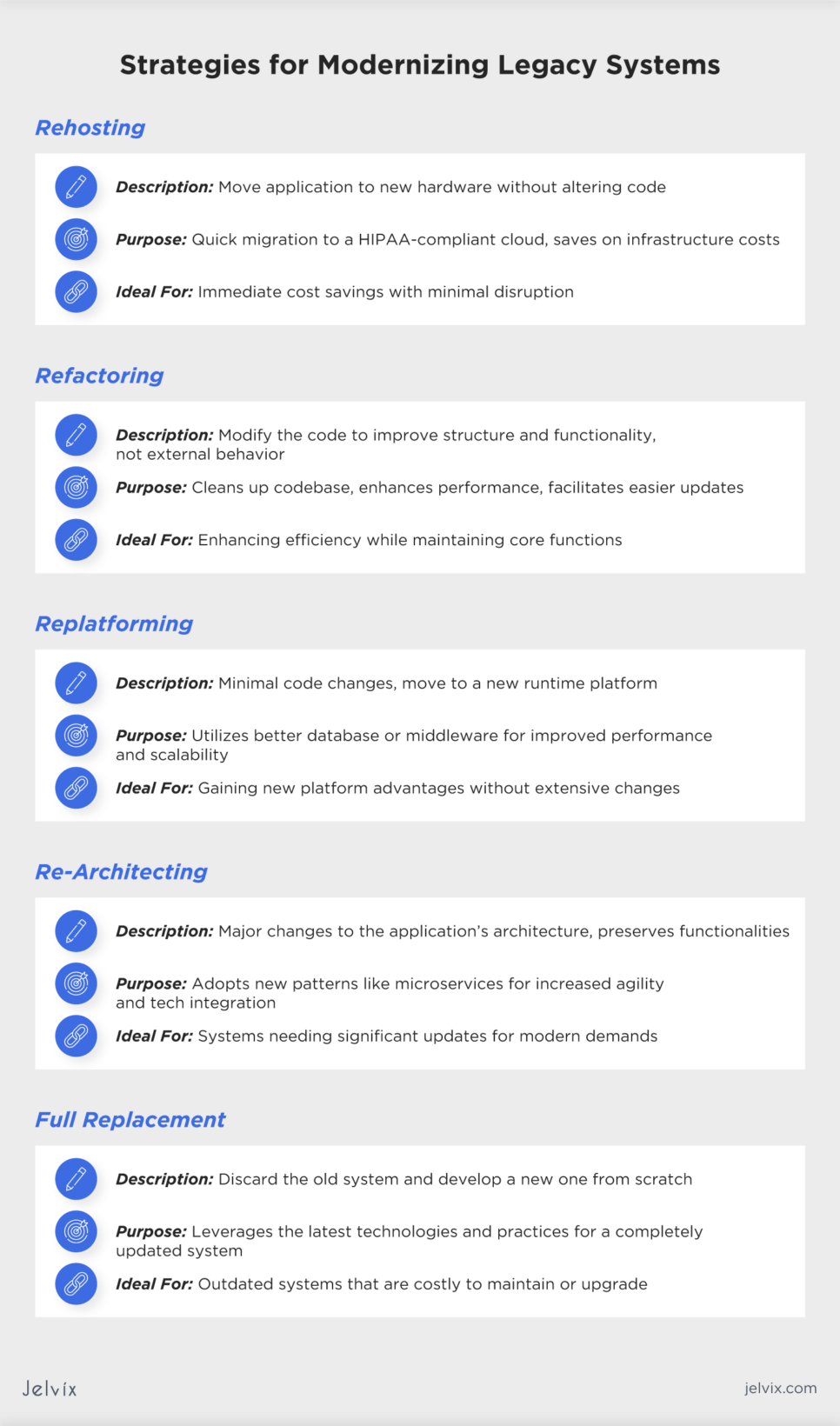
Modernizing Legacy Systems: Key Strategies To Consider
The modernization of legacy systems is a complicated process that involves different strategies, each with its challenges, benefits, and considerations. Selecting the appropriate strategy requires a careful assessment of your current system’s limitations, your entity’s goals, budget constraints, and the desired outcomes.
Rehosting
Rehosting involves moving an application from its current hardware environment to a new one without changing the application’s code, structure, or features. This strategy is typically used for quick migrations to a HIPAA-compliant cloud storage, offering cost savings on infrastructure without the need for extensive changes to the system.
Refactoring
Refactoring involves making code modifications to improve an application’s existing structure and functionality without altering its external behavior. This strategy is often used to clean up the codebase, improve performance, and make future updates easier while keeping the core functionality intact.
Replatforming
Replatforming involves moving an application to a new runtime platform and making minimal changes to the code. This might include adopting new databases or middleware to enhance performance and scalability. The goal is to use better capabilities of the new platform without a complete overhaul.
Re-Architecting
Re-architecting means significantly changing the application’s architecture while preserving its functionalities. This approach is suitable for legacy systems that need to adopt new architectural patterns, such as microservices, to increase agility, scalability, and the ability to integrate with modern technologies.
Full Replacement
Full replacement involves completely discarding the legacy system and developing a new solution from scratch. You should choose this strategy when the existing system no longer meets your organization’s needs, cannot be easily upgraded, or when maintaining it becomes too costly. Full replacement will allow you to take advantage of the latest technologies and best practices, offering a fresh start with a system designed to meet current and future needs.
If you aim at full legacy system replacement but need professional guidance, reach out to our experts for help. They will provide advice based on your healthcare system’s current state and offer a solution that will suit your company’s needs best.
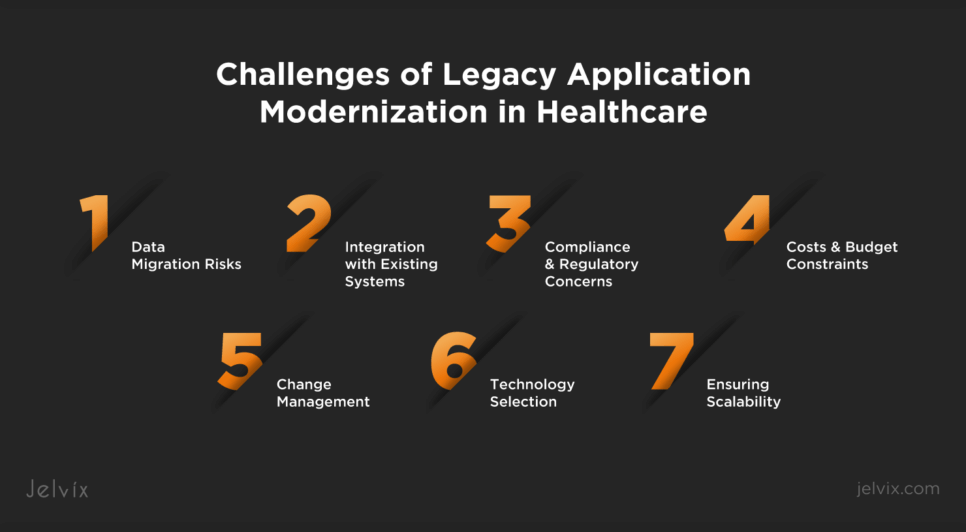
Common Challenges of Legacy Application Modernization in Healthcare
The legacy system modernization process is full of challenges that often stop medical companies from upgrading their tech. To successfully address these challenges, you need to adopt a phased approach that includes planning, technology selection, and phased implementation of newer systems.
Data Migration Risks
Migrating patient and operational data from old systems to new platforms can be complex and risky. There’s a potential for data loss, corruption, or breaches during the transfer process. The Jelvix team recommends that you implement a robust data migration plan that includes data cleansing, mapping, and validation processes. Use encryption and secure data transfer protocols to protect data during migration and conduct incremental data transfer to minimize the risks.
Integration with Existing Systems
Modernized systems must seamlessly integrate with other existing healthcare systems, such as EHRs, billing software, and laboratory information systems. Adopt open standards and APIs to facilitate interoperability between the modernized system and existing applications.
Compliance and Regulatory Concerns
Healthcare is heavily regulated, and modernization efforts must comply with various laws and standards, such as HIPAA and GDPR. Involve compliance experts in the modernization process to ensure all regulatory requirements are addressed.
Costs and Budget Constraints
Budget constraints may limit the scope of modernization efforts or force organizations to prioritize certain functionalities over others, impacting the project’s overall effectiveness. Develop a detailed cost analysis and prioritize modernization efforts based on critical needs and potential ROI.
Change Management
Modernizing legacy systems often requires significant changes to workflows and processes. What’s more, resistance to change among users accustomed to the old system can block the adoption of the new solution. Implement a comprehensive change management strategy and address resistance by providing support throughout the transition.
Technology Selection
Choosing the right technology for the modernized system can be daunting given the rapid pace of technological advancements. Conduct research and planning and make a choice that aligns with both the current and future needs of your entity.
Ensuring Scalability
The modernized system must be scalable to accommodate future growth, additional functionalities, and changing healthcare practices. Choose flexible and modular technologies that can be easily scaled or updated as your organization grows.
Addressing the challenges described above will enable your healthcare entity to realize the full benefits of modernization, leading to improved operational efficiency and enhanced patient care.
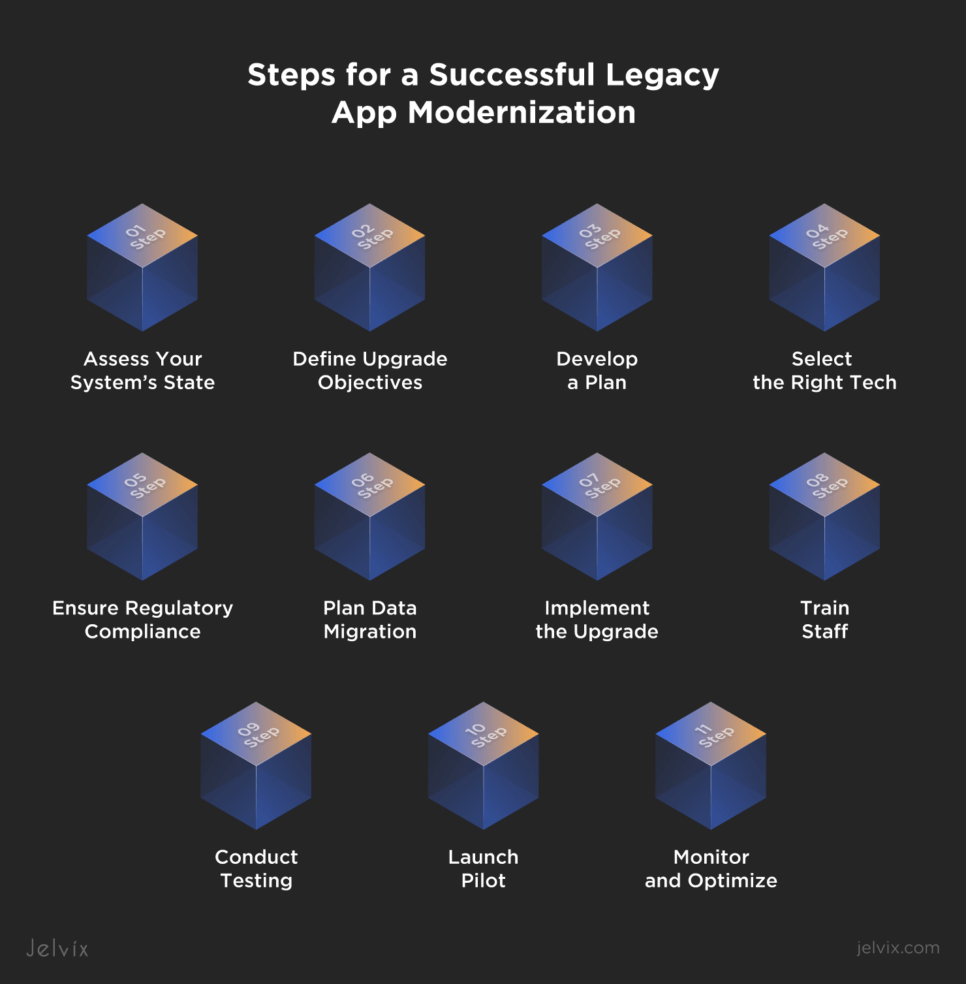
11 Steps for a Successful Legacy App Modernization
Upgrading legacy medical systems requires a structured approach, from initial assessment to post-implementation review. By following these steps, healthcare organizations can ensure a smooth transition to a modern, efficient, and secure infrastructure that supports high-quality patient care.
1. Assess Your System’s State
Begin by evaluating the existing legacy system to understand its capabilities and limitations compared to the needs of your healthcare entity. This assessment should cover technical, operational, and clinical aspects, including user feedback on current challenges.
2. Define Upgrade Objectives
Based on the assessment, clearly define the objectives of the upgrade. Whether it’s to improve patient data management, enhance system security, or achieve better interoperability, setting clear goals will guide the upgrade process and help measure its success.
3. Develop a Plan
Create a detailed plan outlining the upgrade process, including timelines, budget estimates, required resources, and specific technologies to be implemented. This plan should also address how the upgrade will impact existing workflows and how these changes will be managed.
4. Select the Right Tech
Research and select the appropriate technology solutions that align with your upgrade objectives. This may involve choosing new software platforms, hardware, or cloud services. Consider vendor reputation, technology scalability, and compliance with industry standards.
Navigate the complex process of choosing a health tech partner with Jelvix's comprehensive guide. Find essential criteria and expert insights for successful collaborations in healthcare.
5. Ensure Regulatory Compliance
Make sure that the new system complies with all relevant healthcare regulations, such as HIPAA and GDPR for patient data privacy and security. This includes assessing the security features of the new system and its capability to protect patient information.
6. Plan Data Migration
Plan for the safe and efficient migration of patient and operational data to the new system. This involves data cleaning, mapping, and validation to ensure accuracy and integrity during the transition.
7. Implement the Upgrade
Carry out the system upgrade according to your established plan, ensuring minimal disruption to daily operations. This may involve a phased rollout of legacy and new systems to smooth the transition.
8. Train Staff
Provide comprehensive training for all users to ensure a painless transition and adoption of a new system. Training should cover operational, clinical, and security aspects.
9. Conduct Testing
Before going live, test the new system to ensure it meets all functional, security, and compliance requirements. This should involve real-world scenarios and user acceptance testing to identify potential issues.
10. Launch Pilot
Consider launching a pilot phase with a limited scope of resources to confirm everything works as intended. This will allow for troubleshooting of a new solution on a smaller scale to minimize disruption during the full transition.
11. Monitor and Optimize
After testing, proceed with the full implementation of the new system. Monitor it closely for any issues and gather user feedback to make necessary adjustments. Conduct a post-implementation review to evaluate the success against the defined objectives.
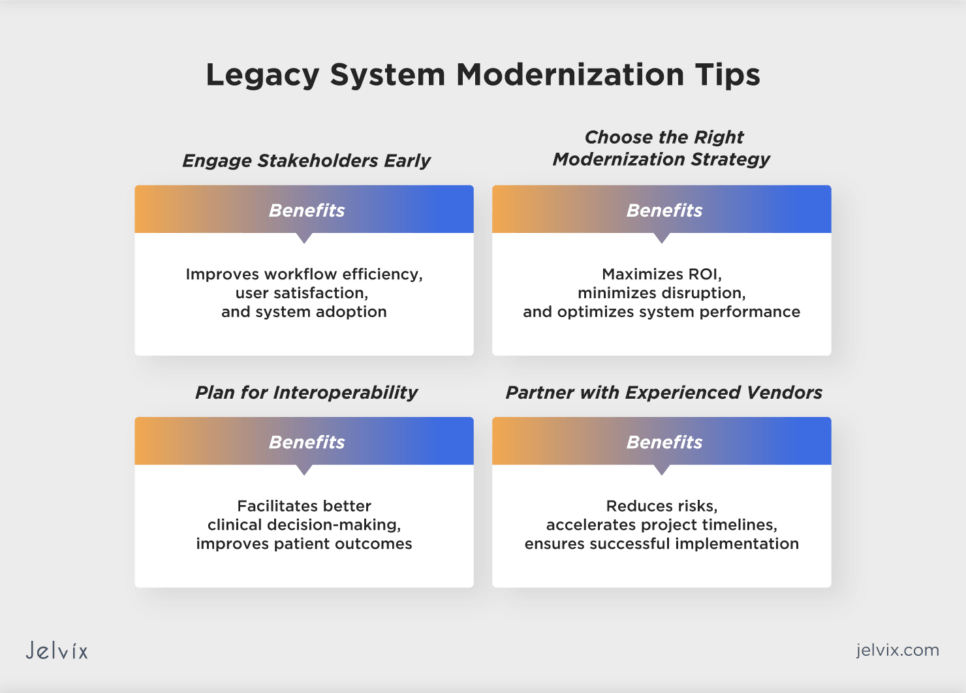
Legacy System Modernization Tips
As you can see, legacy system modernization is a complex process that requires a vast knowledge of the technical and legal aspects of healthcare technology. There are a few tips that you can consider to make the transition process more efficient.
Engage Stakeholders Early
Engage key stakeholders, including clinicians, IT teams, and administrative staff, in the planning stages. Their insights can help identify critical needs and preferences, ensuring the modernized system supports user requirements and improves workflow efficiency.
Choose the Right Modernization Strategy
Determine the most suitable modernization approach (e.g., rehosting, refactoring, replatforming, re-architecting, or full replacement) based on your organization’s needs, budget, and long-term objectives.
Plan for Interoperability
Ensure the modernized system can seamlessly exchange data with other healthcare systems. Adopting standards like HL7 or FHIR API for data exchange can enhance interoperability, facilitating more coordinated and efficient patient care.
Partner with Experienced Vendors
Select a technology partner with a proven track record in healthcare system modernization. Experienced vendors can offer valuable insights, guide you through the modernization process, and provide ongoing support.
Healthcare Legacy System Modernization Use Cases
Modernization of a legacy healthcare system is an investment in the future of your medical company. That’s why it’s important to consider real-world use cases that demonstrate how healthcare organizations across various settings can benefit from legacy system modernization.
Upgrading EHR to Accelerate the Use of AI
The National Institutes of Health has recently recognized the need to upgrade its 20-year-old EHR system. The primary goal is to keep up with developing healthcare tech trends and be able to use AI tools to support clinical decision-making. To date, NIH has identified over 1,000 requirements for its new EHR system.
Increasing the Number of Remote Visits
During the COVID-19 pandemic, Cleveland Clinic upgraded its medical system to be able to provide telehealth services to patients. As a result, outpatient visits conducted remotely increased from 2% to 75% in just over a month, demonstrating a successful transition to virtual care delivery.
Saving Time and Reducing Medical Errors
The upgrade of a legacy system allowed the Calderdale and Huddersfield NHS Foundation Trust in the UK to implement voice recognition technology. Within just 6 months, CHFT saved 150,000 minutes previously spent on routine data entry tasks, reducing the workload for staff and minimizing errors in patient data.
How Jelvix Can Assist in Modernizing Your Legacy System
Legacy system modernization is a critical step for embracing digital transformation and the medical tech advancements it brings. Although software modernization carries costs, it can make your clinical operations more cost-efficient in the future.
At Jelvix, we specialize in upgrading legacy applications and developing new healthcare solutions that we securely integrate into existing medical platforms. If you struggle to evaluate the state of your current EHR system and are not sure what exactly you should do, reach out to our experts for a consultation. Our experienced team of developers will help evaluate your current needs and offer customized strategies for successful legacy system modernization.
Upgrade your healthcare operations with Jelvix's expertise.
Provide seamless integration of new solutions into existing platforms for cost-efficient clinical operations.