It’s no longer just a guess that AI will be used in dentistry; it’s already being utilized, it’s growing quickly, and it’s been proven to work in business. Almost one-fifth of dental offices around the world are using AI-driven platforms as of 2024.
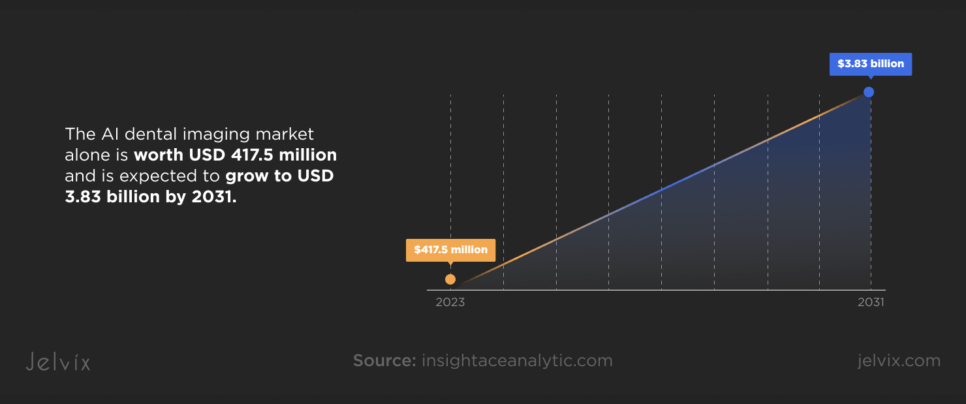
Latest research done by Insight Ace Analytics shows that the AI dental imaging market alone is worth USD 417.5 million and is expected to grow to USD 3.83 billion by 2031. That’s a 32.5% CAGR, which is not a trend line but a path that’s transforming an entire vertical.
When 77% of dentists say they’ve seen real improvements in their practice and more than 59% of patients say they trust AI-enhanced treatment more, as stated in Dentistry, adoption becomes strategic.
The signal is just as obvious on the research front. Over the last ten years, there has been a 21.6% rise in dental papers that mention AI. However, the 34.5% rise in only the last five years is even more significant. That makes sense for markets.
The global digital dentistry market, which uses AI in its infrastructure, according to Insight Ace Analytics, is expected to grow from $6 billion in 2024 to almost $19.66 billion by 2034, with a strong 12.6% CAGR.
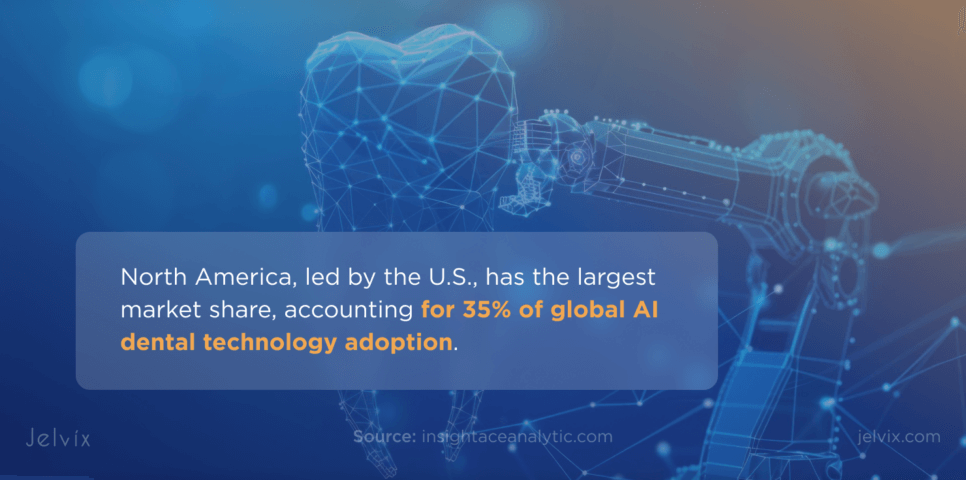
North America, led by the U.S., has the largest market share, accounting for 35% of global AI dental technology adoption. The region continues to set the pace through institutional investment and regulatory readiness.
Why AI Is Becoming a Competitive Necessity for Dental Software Providers
The AI in dentistry field is now a great chance for healthcare software development companies since it has unmet clinical demands, regulatory support, and the potential for growth. Dental practitioners no longer want static platforms; they want smart solutions that can analyze, predict, and improve treatment pathways on their own.
This isn’t simply about imaging and diagnosing teeth, even if that is still the most popular area. AI will be used in all parts of the practice, from predictive analytics and patient management to robotic assistance with making decisions in real time.
In the meantime, the machine learning subfield is the most important part of the tech stack because it can read imaging data, X-rays, CBCT scans, and intraoral visuals, with clinical-grade accuracy.
Simultaneously, we are seeing automation and education come together. Overjet for Educators, which was previously approved by the FDA and came out in 2024, was a big step forward. The same AI technologies that are utilized in the best dental clinics are now being used to train the next generation of oral health professionals.
The ecosystem, along with Harvard’s 2025 Global Symposium on AI in Dentistry, shows that things are evolving from individual applications to whole systems.
To put it another way, this isn’t a race. It’s a shift in platforms, and providers who don’t construct AI-ready infrastructure now will find themselves building on outdated ground tomorrow. In the next sections, we’ll look at every part of employing AI in dentistry, from technological integration and clinical validation to compliance, risk reduction, and long-term growth.
Advantages of AI in Dentistry
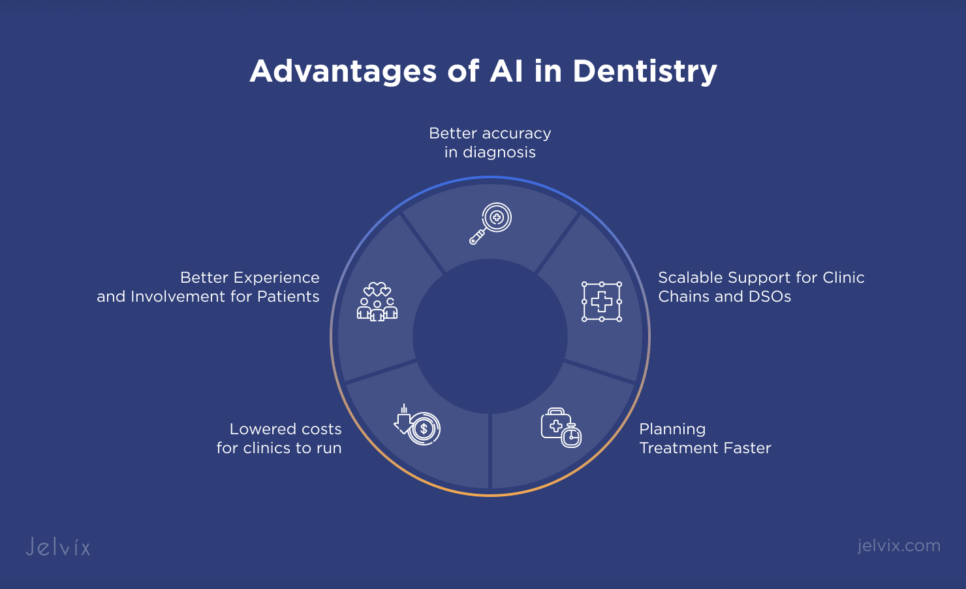
Artificial intelligence in dentistry has grown much beyond proof-of-concept in terms of its use. Today, AI is an essential part of diagnosis, workflow optimization, and communication with patients. Dental AI solutions are making substantial improvements in accuracy, efficiency, and cost structure, whether they are used in single practices or throughout DSOs. Here are the most important benefits that show how AI is changing the way dentists work today:
Better Accuracy in Diagnosis
AI-powered image analysis consistently enhances the reliability of diagnoses. Some platforms use deep learning to find cavities, bone resorption, and periodontal disease at a level of accuracy that is hard to achieve manually. Finding problems early on, sometimes years before a person can, means less aggressive treatments and better long-term results.
Planning Treatment Faster
AI speeds up clinical workflows by breaking down X-rays, intraoral scans, and patient histories. Dentists don’t have to spend time planning anymore. Instead, they get options that are based on facts and probability. This quick decision support cuts down on treatment delays and makes time-to-care metrics better.
Lowered Costs for Clinics to Run
Automating regular processes, such as billing, scheduling, and charting, saves staff time and reduces mistakes made by the administration. Predictive analytics also helps with capacity planning and inventory management, which makes businesses more financially flexible.
Lowered Costs for Clinics to Run
AI doesn’t merely work in the background. It makes the front-facing experience better by letting dentists display patients’ diagnostic images in real time, simulate treatment outcomes, and tailor care pathways to each patient. This openness builds trust, especially as 59% of patients say they feel more confident when AI is employed in their care.
Scalable Support for Clinic Chains and DSOs
Enterprise-grade AI solutions let group practices ensure that quality is the same at all of their sites, even if they are far apart. Centralized AI integration ensures that treatment planning, outcome monitoring, and compliance reporting are all done the same way every time.
AI in Dentistry Use Cases
The practical applications of AI for dentistry extend far beyond image analysis or scheduling widgets. Today’s systems are built as integrated intelligence layers—designed to enhance diagnostic rigor, optimize back-office workflows, and personalize clinical decision-making. From frontline care to operational backend, dental artificial intelligence is reshaping the technology stack.
AI-Powered Dental Imaging and Diagnostics
Advanced artificial intelligence (AI) imaging software powered by deep convolutional neural networks (CNNs) is being used to assist in the detection of carious lesions, root fractures, bone loss, and periapical pathology with high accuracy. AI dental software analyzes X-ray images in real time (formatted via DICOM) and superimposes diagnostic proposals directly onto the clinician’s viewer.
In addition, the fact that the system can be used for longitudinal analysis of image sequences allows time series disease progression analysis, which would be infeasible for manual processing at volume scales.
Predictive Analytics for Treatment Outcomes
Based on historical patient data, AI dental models predict the likely response to treatment based on age, comorbidity, history of procedure, and radiologic findings. These models use structured clinical data and gradient-boosted decision trees to evaluate treatment efficacy and guide clinicians to align treatments with those that have statistically optimal outcomes.
Such forecasting-based planning steps the drug-treatment planning from the reactive treatment to preventive (or proactive) treatment.
Virtual Assistants for Patient Interaction
NLP models are used in conversational AI interfaces for FAQs, appointment pre-screening, post-op care instructions, and intake information collection. Unlike run-of-the-mill chatbots, dental AI assistants are trained on a specialized, domain-specific dataset and are context-aware as well as HIPAA-ready. With integration with practice management solutions, patient responses are automatically parsed and attached to the charts.
AI in Appointment Scheduling and No-Show Reduction
Scheduling platforms now incorporate predictive modeling algorithms to maximize the use of calendars. These models consider previous attendance records, the weather, traffic in the area, and patient demographics to identify likely no-show patients and overbook. The reminders (mostly AI-driven) sent to a user on their phone, via SMS or email, are contextually time-based and do, in turn, increase response rates and reduce idle chair time.
Real-Time Insurance Verification with AI
AI dental software is being used to verify patient eligibility in real time by parsing Electronic Data Interchange (EDI) 270/271 transactions. Instead of manual phone calls or waiting on payer portals, AI scrapes and structures coverage data instantly, reducing administrative lag. Rules engines also flag mismatches in CDT codes vs. policy exclusions, minimizing claim denials and audit exposure.
AI-Powered Charting and Clinical Documentation
AI transcription tools with voice recognition are helping automate charting. These programs are augmented with speech-to-text engines that are tailored for dentistry, and they also have the ability to transcribe those chairside dictations for you and auto-fill the SOAP notes. A few of the solutions integrate with EHRs and utilize NLU to extract and code clinical insights into structured fields, improving documentation and enhancing the accuracy of ICD/CPT mapping.
AI-Based Patient Risk Stratification
Patients are stratified according to the presence or degree of risk factors, such as risk of periodontal disease progression, potential for oral cancer, or probability of orthodontic relapse, using classification algorithms. Machine learning models such as logistic regression and neural networks, trained on population-level data, facilitate practices transitioning toward risk-adjusted care pathways, an essential component for preventive dentistry and long-term planning.
Revenue Cycle Optimization and Billing Automation
Machine learning is streamlining revenue cycle management by identifying coding errors, underbilling patterns, and claim status anomalies. AI bots reconcile EOBs (Explanations of Benefits) and automatically generate appeals for underpaid claims. Platforms like Apteryx and Carestream Dental embed these capabilities into their workflows, allowing dental teams to increase collection efficiency without increasing the number of billing staff.
Real-World Examples of AI in Dental Software
Several companies in the AI dentistry field are using production-grade systems that accomplish far more than just diagnosis. For example, Pearl’s “Second Opinion®” platform uses convolutional neural networks to scan X-rays for more than 30 dental issues and provide real-time notes that can be added straight to the practitioner’s imaging program. The FDA approved the instrument, and it is now used in more than 100 nations, including by several DSOs in the U.S.
Overjet’s AI suite also looks at bitewing and panoramic radiographs to measure bone levels and find calculus. This not only makes diagnoses more accurate, but it also helps with periodontal management. Their FDA-approved models are built into big business systems like Dentrix and Eaglesoft, which makes it easier for practitioners to handle risk assessment, compliance paperwork, and treatment acceptance.
AI dental app Bola AI is changing the way practices engage with patients on the administrative side by using voice-assisted documentation, NLP-powered intake, and automated insurance verifications. Similar AI applications in dentistry fill in EHR fields with almost no delay by using a mix of speech recognition in real time and dental-specific NLU models. The end effect was much less time spent on charting and more accurate billing entries.
Apteryx Imaging’s cloud-based platform is another example. It blends AI-enhanced image analysis with automatic CDT code assignment, which speeds up both clinical review and reimbursement timelines. In general, these solutions show how AI has evolved from a diagnostic tool to an operational backbone. This means that AI dentistry can work as a full-stack augmentation layer in both clinical and commercial areas, not simply as an assistant.
Implementation Challenges and Best Practices
Ensuring Patient Safety with AI-Driven Tools
No AI dentistry deployment is successful unless it begins with patient safety as a core design principle. AI models must be trained on high-quality, representative datasets to avoid clinical blind spots. Dental practices need robust validation protocols, including clinician-in-the-loop verification and routine performance benchmarking, to ensure models continue operating safely over time.
Addressing Interoperability and Third-Party Integrations
Most AI dental software solutions are not built in isolation—they need to interact with PMS, EHRs, imaging tools, billing platforms, and sometimes even CRM systems. Legacy software systems and fragmented tech stacks are indeed an impediment to smooth deployment.
HL7 FHIR-based APIs, microservices that are modular, and middleware adapters have emerged as technical best practices to ensure that AI applications in dentistry can plug into existing infrastructure without risking data loss, version conflicts, or system downtime.
Maintaining Data Privacy and HIPAA Compliance
Handling PHI (Protected Health Information) in compliance with HIPAA and local regulations is an architectural constraint. AI must run in secure and auditable environments with full encryption, access control, and audit logging. And during use, identity data leaks must be prevented through anonymization of training datasets and role-based access controls.
Practices should also make sure that any AI dental app is signed to a Business Associate Agreement (BAA) before onboarding any 3rd party vendor.
Avoiding “Shadow AI” in Dental Organizations
Shadow AI, unauthorized, unvetted AI tools being used informally by staff, can introduce systemic risk. Whether it’s using unapproved diagnostic plugins or productivity bots with questionable privacy practices, the absence of governance can lead to compliance violations or patient harm. Mitigation demands implementation of AI usage audits, digital access tracking, and staff education.
As demonstrated in Jelvix’s ethical AI chatbot development, integrating ethics and oversight from design to deployment ensures that AI systems remain safe, auditable, and legally compliant.
Read more about the developing Healthcare Chatbot with a focus on Ethical AI case.
Building Explainable and Transparent Models
Black-box models pose a reputational and regulatory threat in healthcare. Clinicians are increasingly asking for interpretable systems, those showing why a diagnosis has been flagged or why a treatment path has been recommended.
Techniques like saliency mapping, feature attribution (e.g., SHAP, LIME), and human-readable audit trails are becoming non-negotiable in production environments. Transparent AI for dentistry allows dental professionals to be confident within their decision-making process while simultaneously keeping trust with the patient and the auditor.
Step-by-Step AI Implementation Roadmap
There’s no one-size-fits-all approach to incorporating AI into your practice. This is a phased process that requires technical acumen, regulatory savvy, and harmonious agreement between dentists’ aspirations and algorithms’ capabilities. Below is a roadmap of how dental practices and groups can embrace dental artificial intelligence solutions in an efficient and sustainable way.
Step 1: Define Business Objectives and Expected ROI
Start with a well-defined statement of purpose for why you are introducing AI. Do you seek to improve diagnostic accuracy, eliminate manual charting, increase treatment acceptance, and/or automate revenue cycle functions? Quantify your expectations with KPIs such as lower diagnostic time per case, higher reimbursement rates, or higher patient throughput. Setting ROI goals up front will focus vendor selection and avoid a disconnect between strategic investments and tactical uptake.
Step 2: Assess Technical Readiness and Legacy Infrastructure
Not every dental work space is an AI-compatible one. Assess your present ecosystem: practice management systems, imaging devices, data storage policies, and network bandwidth. A large number of dental AI application platforms rely on DICOM-compliant imaging machines and support HL7/FHIR integration layers. Organizations using older or siloed technologies may need middleware or hardware upgrades before AI can even be integrated.
Step 3: Choose Between Custom and Off-the-Shelf AI Solutions
The product architecture selection is key. For standardized processes, pre-trained AI diagnostic dental tools such as Pearl or Overjet offer rapid deployment and FDA-cleared confidence. Custom development may be required for practices with extra or custom operational structures, such as DSOs, with regionalized compliance policies.
This frequently involves the choice of particular model architectures (CNNs for radiography, NLP for intake, decision trees for patient risk scoring) and the deployment of those architectures through on-prem, hybrid, and/or cloud-native infrastructure.
Step 4: Prototype and Validate with Real Data
Generic benchmarks also aren’t sufficient. You will need to test the AI tools on your own clinical data, including X-rays, case notes, intra-oral images, and diagnostic histories, to ensure they are functioning correctly in the intended context and that no human bias, biased drift, or edge-case failure modes are detected.
Public datasets aren’t always contaminated with the noise and diversity inherent to real-world procedures, such as the non-uniform exposure of X-rays, the non-standard ways for annotation while repeating the same procedure, or the bizarre diseases.
It would also be wise to examine the performance of the AI diagnostic dental workflow through precision, recall, F1-score, and AUC-ROC, especially for false-positive cases, where a single case may cause unnecessary operations. If one of these conditions is highly prevalent in the dataset and you have few examples of the other, then simply using sensitivity and specificity is insufficient.
Demographic stratified sample, such as age, sex, and ethnicity, as well as device variability (for example, sensors from Vatech, Carestream, or Planmeca), should be part of the validation process.
For a strong evaluation, practices can execute parallel testing. This means that physicians do their normal diagnostic process while the AI works in the background. Discrepancies are marked, checked, and spoken about in meetings with people from other fields.
This method not only checks for accuracy, but it also shows where the model’s logic could not match up with the heuristics used by practitioners. If the dental AI software uses continuous learning, model changes should be tested in a safe environment before being put into production.
Step 5: Test for Compliance and Reliability
Regulatory problems can stop installations that would have otherwise worked out well. Make sure that your solution fulfills HIPAA standards, has encryption for data at rest and in transit, and has sufficient audit trails.
Also, investigate what occurs when the model gives an unclear conclusion if the imaging input is of poor quality. FDA clearance (or anything similar) is strong evidence that a system is clinically grade, but it doesn’t replace compliance checks that are particular to the practice. Be strict here; examples of AI in dentistry indicate that even small gaps in reliability can make clinicians lose trust.
Step 6: Gradual Rollout and Staff Enablement
Put AI to work in low-risk, non-diagnostic areas first, like triage support, post-visit summaries, recall reminders, or insurance verification. Then, add it to essential clinical operations like detecting cavities or staging periodontal disease. These early-stage deployments are like sandboxes; they give operational signals without putting patients at danger.
For example, using AI to automate appointment confirmations or sort patients by how urgent their treatment is based on keywords in their intake forms might make scheduling better without changing how doctors make decisions.
At the same time, invest in structured enablement. Training staff should include more than just walkthroughs of the UI. Not only do team members need to know how to use the dental AI software, but they also need to know when to ignore it, point out problems, or ask for further information when the results are unclear.
User feedback channels included in AI should make it more open. These are UI components that let doctors check, fix, or add notes to AI outputs in real time. This user input can be saved and used in active learning pipelines, which improve the model all the time without having to start over from scratch.
In larger practices or DSOs, AI champions —typically senior clinical staff trained to serve as internal advocates — can continue to provide peer-to-peer support and gather feedback from the front lines to refine the models over time.
Step 7: Continuous Monitoring and Optimization
After the launch, you’re not done. Drift detection systems should monitor changes in the way data is entered or the way models output results. Keep an eye on performance measures over time, like how accurate your diagnostics are, how often you make billing mistakes, and how much more engaged your patients are.
Then, compare them to your baseline KPIs. AI technology in dentistry needs to change with both data and workflow in order to stay clinically useful. This can be done by retraining every so often or by using federated learning pipelines.
Ethical AI in Dentistry
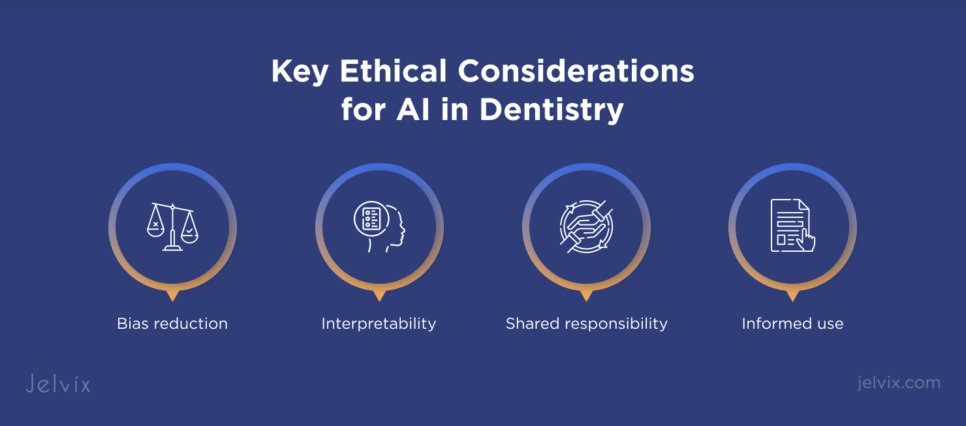
As we become increasingly dependent on automated diagnostics and decision support, AI ethics in healthcare must be tackled directly to avoid unintended negative impact and maintain trust. Key ethical considerations include:
- Bias reduction: The training data should be representative to avoid a situation of systemic under- or overdiagnosis depending on age, race, or socioeconomic status.
- Interpretability: AI results (i.e., identified lesions, risk scores) should be accompanied by an explanation of why a certain output was obtained, or a visual demonstration, not a “number you should trust”.
- Informed use: Patients should be notified when AI tools are involved in their care. When people are presented with consent forms and treatment discussions, it must be made clear what role AI has in diagnostics or planning, if any.
- Shared responsibility: AI systems should be aiding, rather than overriding, clinicians. Ultimately, this must remain in the hands of licensed professionals for clinical accountability and legal transparency.
And it needs to be done responsibly, along with the most stringent AI development standards, auditability, ongoing model validation, and entire life cycle governance. By baking ethics into system design and roll-out, the individual dental practice can be innovative and scale without selling its soul.
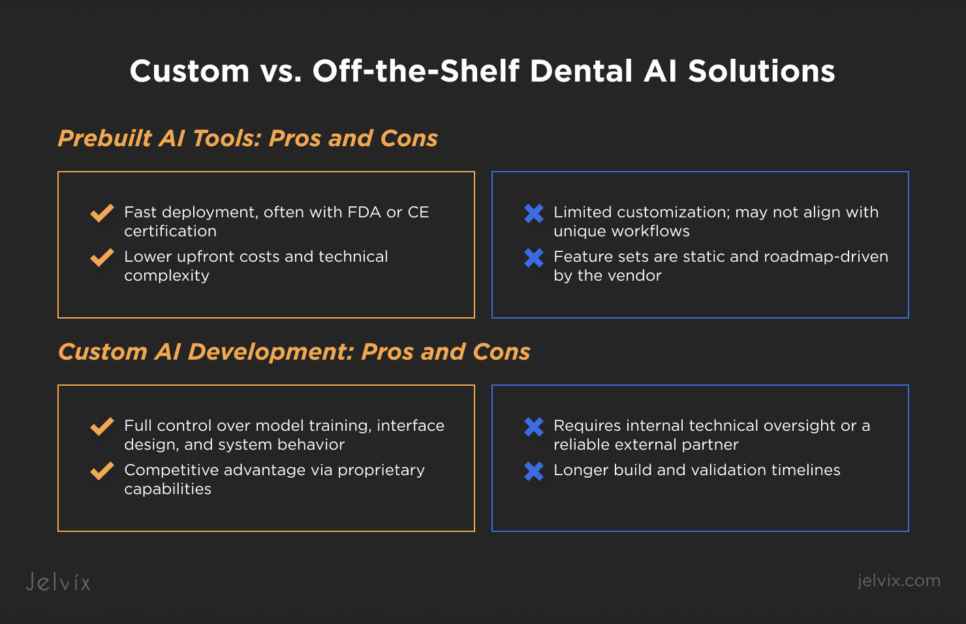
Custom vs. Off-the-Shelf Dental AI Solutions
Choosing between prebuilt and custom dental AI solutions depends on your clinic’s scale, infrastructure, and strategic goals. Each path offers distinct trade-offs in speed, control, and ROI.
Prebuilt AI Tools: Pros and Cons
+ Fast deployment, often with FDA or CE certification
+ Lower upfront costs and technical complexity
– Limited customization; may not align with unique workflows
– Feature sets are static and roadmap-driven by the vendor.
Custom AI Development: Pros and Cons
+ Full control over model training, interface design, and system behavior
+ Competitive advantage via proprietary capabilities
– Requires internal technical oversight or a reliable external partner
– Longer build and validation timelines.
Cost & ROI Considerations
Prebuilt options are usually cheaper upfront and will probably need some kind of short-term or third-party hack fix later. Custom systems require higher CapEx but provide better long-term ROI if designed to meet high-throughput needs or for a multi-site environment.
For instance, a mid-size DSO implementing generic AI-driven diagnostics could achieve ROI in 6–12 months through better case acceptance, while building a predictive tool for patient retention can take longer to break, but would support even stronger margin development down the line.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

The Future of AI in Dentistry
In the future, the combination of AI technology in dentistry with robotics, 3D printing, and digital pharmaceuticals will completely change how things are done in the clinic and how businesses work. Real-time AI imaging analytics will help robots put implants more accurately, which will lower the risk of mistakes during surgery and make the implants last longer.
AI algorithms will change treatment plans in real time based on intraoral scan data in orthodontics. This will allow for ultra-personalized aligner sequences with very little operator input. AI-optimized geometries will power 3D printing systems for prosthodontics, which will speed up the process and improve the fit, especially for full-mouth reconstructions.
As these systems get better, government agencies will need more and more explainable AI, strong audit trails, and the capacity to work with national health data platforms. Dental groups that want to use AI for more than just diagnostics need to focus on architectures that are not just fast but also compliant, easy to understand, and modular.
This includes using adaptive learning pipelines, putting bias reduction into every layer, and following standards for care across specialties. The future isn’t just automated; it’s run by smart algorithms that make human decisions better while still following the rules of healthcare.
Conclusion
AI’s position in dentistry has grown from being a test to becoming an important part of the infrastructure that makes precise diagnostics, simplified procedures, and scalable patient care possible. But having access to the latest tools isn’t enough to make it work.
It requires careful coordination of data workflows, clinician confidence, system interoperability, and compliance with regulations. If AI projects aren’t planned and watched after properly, they can cause problems, lower outcomes, or have other unanticipated effects. This shows the bigger risks of AI in healthcare without sufficient safeguards.
We at Jelvix are experts in closing that gap. Our team can help you with everything from evaluating your technical infrastructure and data strategy to validating your model, making sure it meets compliance standards, and deploying it in a way that can grow with your needs.
This is true whether you are using an FDA-approved, off-the-shelf AI platform or building a completely custom solution that fits your clinical model. We are a trusted partner for dental organizations going through AI transformation since we know a lot about AI systems architecture, domain-specific machine learning, and regulatory design.
Check out our AI development services to find out how we can help you stay ahead of the curve with smart, ethical, and results-driven technology. Get in touch – we’re ready to take on your next challenge.
FAQ
How is AI different from rule-based automation in dental software?
AI can learn from data and get better over time, but traditional rule-based systems need hardcoded logic. This helps people make better choices, especially when it comes to diagnosis, scheduling, and arranging therapy.
How much annotated dental data is needed to train an effective AI model?
Model complexity and specific task influence data needs. For example, image-based models like X-rays usually require thousands of labeled samples, whereas NLP models used for documentation might need structured clinical notes or transcripts.
Can AI be integrated with legacy dental EHRs and practice management systems?
Yes, although it often needs middleware or a microservices architecture to connect data flows. Ensuring compatibility with HL7, FHIR, or proprietary APIs is essential for smooth integration.
What are the hidden costs of AI implementation for dental platforms?
In addition to development, companies need to consider data annotation, staff training, model validation, compliance, continuous monitoring, and infrastructure to support real-time processing or retraining.
Is AI suitable for small or mid-sized dental SaaS companies?
Certainly. Many companies initially utilize pre-trained AI APIs, such as image classification and voice recognition, before developing custom models, which helps lower entry barriers and reduce costs.
How do companies measure ROI from AI adoption?
Key metrics include reduced admin hours, faster patient onboarding, higher diagnostic accuracy, fewer no-shows, increased retention, and faster insurance processing.
Need a qualified team of developers?
Extend your development capacity with the dedicated team of professionals.