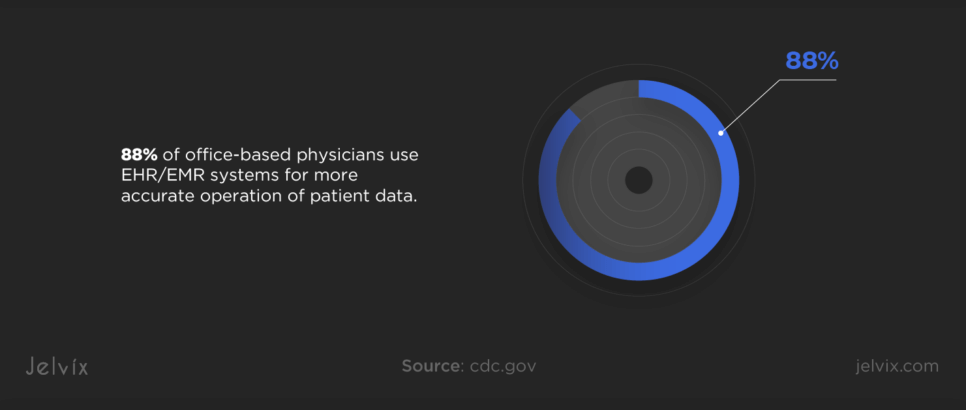
With the development of digital technologies and the growing amount of user data, businesses seek ways to facilitate data entry, storage, and management. In healthcare, 88% of office-based physicians use EHR/EMR systems for more accurate operation of patient data.
However, adopting an EHR system into established healthcare settings can be challenging. It requires managing data migration, maintaining regulatory compliance, and ensuring staff training for successful system use.
If you’re a healthcare provider, consultant, or IT specialist aiming to improve clinical workflows by adopting EHRs, keep reading. You’ll find out how to choose the right system, how to prepare your clinic for EHR adoption, and steps to develop an implementation plan.
What Is an EHR System in Healthcare?
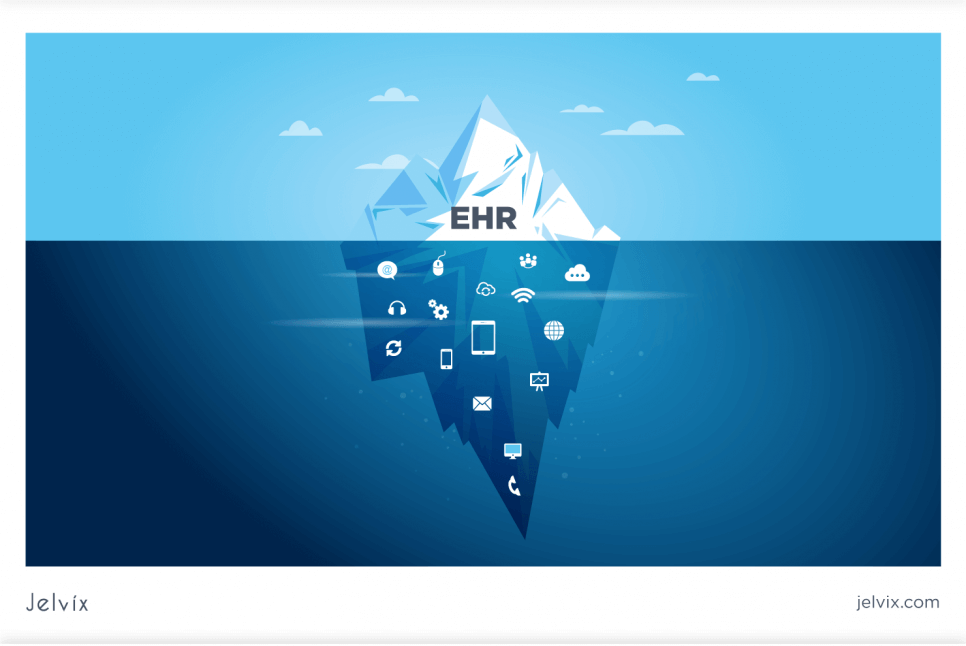
An Electronic Health Record (EHR) system is a digital platform that stores patient health information, replacing traditional paper records. It consolidates data such as patient history, medications, lab results, and treatment plans, making it accessible in real time to authorized users across different healthcare settings.
The Importance of EHRs in Modern Healthcare
EHR systems offer numerous benefits that streamline healthcare delivery, making it safer, more efficient, and patient-centered.
Centralized Patient Information
EHRs centralize all patient data like medical history, medications, and diagnoses in one location, enabling coordinated care by providing healthcare professionals with instant access to patient information.
Improved Patient Care
EHRs enhance patient care quality by offering access to the latest research and clinical guidelines, supporting accurate diagnoses, reducing medical errors, and improving safety through critical alerts.
Enhanced Efficiency
By streamlining workflows and reducing paperwork, EHRs save time and resources, speed up prescriptions, and improve communication across care teams, allowing healthcare professionals to focus on patient care instead of administrative tasks.
Secure Sharing of Patient Information
Secure sharing of patient information via EHRs streamlines care coordination, making clinical decision-making more efficient. It ensures privacy compliance, reduces legal risks, and enhances patient care quality.
Preparing for the Adoption of EHR
The transition to an EHR system requires a well-thought-out strategy for a smooth adoption. This involves assessing your organization’s needs and considering key factors, such as usability, scalability, and healthcare interoperability of your EHR solution.
Assessing Your Healthcare Organization’s Needs
Before you go into choosing an EHR system for your organization, make sure to evaluate your needs. Begin by mapping out current workflows and processes to identify how they can be optimized with an EHR system. Then, define what you aim to achieve with the EHR system: improving patient care, increasing efficiency, or ensuring compliance with health regulations. Finally, evaluate your current IT infrastructure to determine if any upgrades or changes are needed to support the new EHR system.
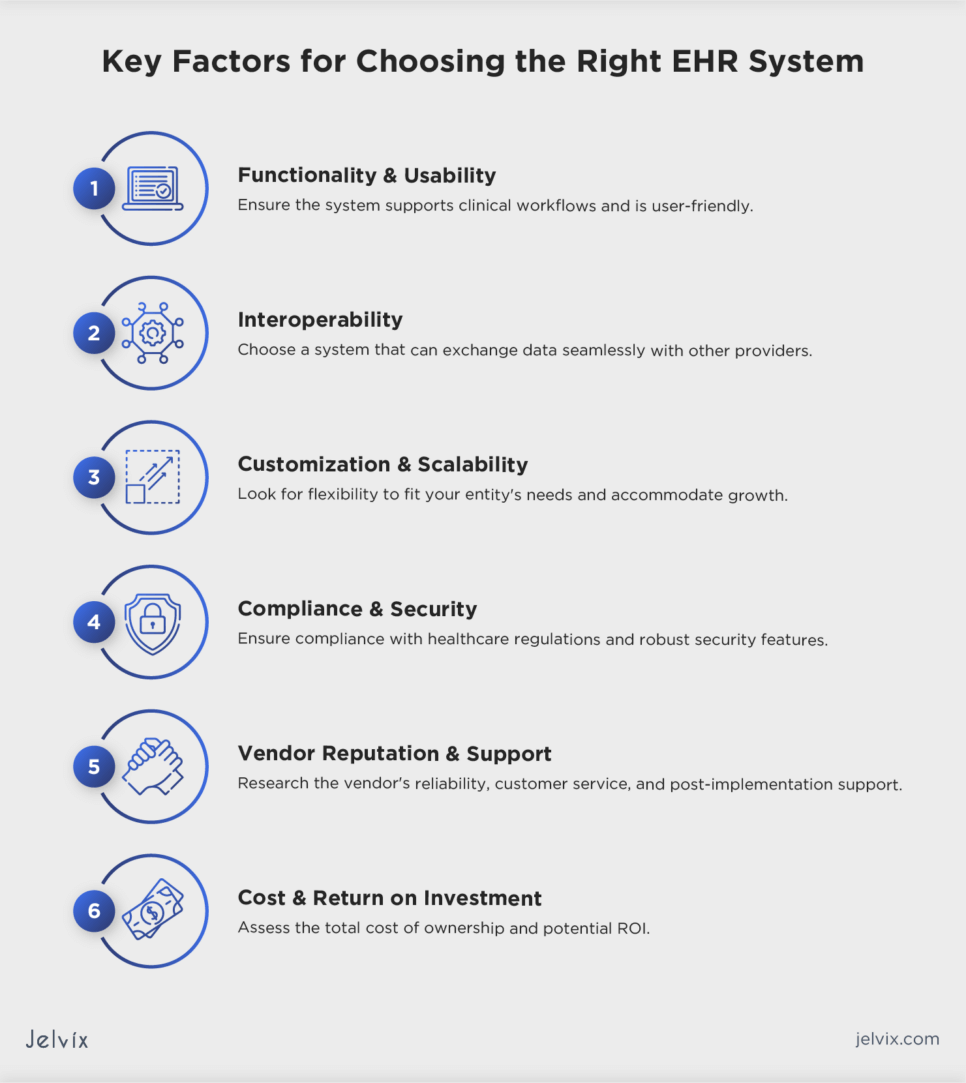
Choosing the Right EHR System: Key Considerations
Since EHR is aimed at streamlining clinical operations, providers should evaluate a range of factors to find a system that best fits their unique needs.
Functionality and Usability
Ensure the EHR system has the functionalities required to support your clinical workflows, including patient scheduling, documentation, order entry, and billing. Evaluate the system’s usability to ensure it is intuitive and user-friendly to minimize the learning curve for your staff.
Interoperability
Choose a system that can easily exchange data with other EHR/EMR providers, laboratories, and pharmacies to ensure seamless care coordination. Assess the system’s ability to integrate with existing healthcare infrastructure, such as practice management systems and health information exchanges.
Customization and Scalability
Look for an EHR system that can be customized to fit the specific workflows and needs of your medical entity. Consider the system’s scalability to accommodate growth, add new functionalities, and integrate with new technologies.
Compliance and Security
The system must comply with healthcare regulations, such as HIPAA and GDPR, to protect patient privacy and ensure data security. Evaluate the system’s security features, such as data encryption, access controls, and audit trails, to safeguard patient information against breaches.
Vendor Reputation and Support
Research the vendor’s reliability, customer service, and support offered post-implementation.
Make sure that they have experience in the healthcare sector and offer system updates with the latest healthcare standards and technologies.
Cost and Return on Investment
Assess the total cost of ownership, including upfront costs, implementation, training, ongoing maintenance, and additional fees for upgrades or support. Evaluate the potential ROI, considering improvements in efficiency, patient satisfaction, and the ability to meet regulatory requirements.
If you’re struggling to choose a reliable tech partner or have concerns about the functionalities your EHR system should have, feel free to contact us for a consultation.
Discover how integrating EHR with healthcare CRM enhances patient care, streamlines workflows, and boosts operational efficiency.
Developing an EHR Implementation Plan: Key Steps
A well-structured implementation plan ensures that the transition to an EHR system is smooth, with minimum disruptions to clinical workflows. The Jelvix team recommends that you adopt a step-by-step approach for successful EHR implementation.
1. Establish a Team
Form a multidisciplinary team, including clinical, IT, administrative, and financial specialists, to make key decisions and serve as a bridge between medical staff and the EHR vendor.
2. Define Goals and Objectives
Clearly outline what you aim to achieve with the EHR system. Goals may include improving patient care, enhancing data security, or increasing operational efficiency. Consider adopting a SMART strategy, where objectives are specific, measurable, achievable, relevant, and time-bound.
3. Conduct a Workflow Analysis
Map out current workflows to identify how processes are carried out without an EHR and how they will change after its implementation. This will help to fit an EHR to existing workflows and identify areas for improvement.
4. Choose the Right EHR System
Based on the needs assessment and workflow analysis, select an EHR system that aligns with your organization’s requirements, as discussed in previous steps.
5. Develop a Project Plan
Create a comprehensive project plan that includes timelines, milestones, responsibilities, and budget. The plan should cover all phases of the implementation process, from system customization to staff training.
6. Prepare for Data Migration
Decide on the data that needs to be migrated to the new EHR system. Plan for a clean-up of existing data to ensure that only accurate and relevant information is transferred.
7. Provide Training and Support
Develop a training program tailored to all user roles and responsibilities. Training should be ongoing, with initial sessions before the launch and refresher courses afterward. Ensure that your EHR vendor provides technical support to address the issues promptly.
8. Implement a Pilot Phase
Consider running a pilot phase with a small group of users. This will help you identify and address any issues before a full-scale rollout.
9. Launch the New System
Choose a go-live date, preferably during a quieter period to minimize disruptions. Provide comprehensive on-site support to assist users with any immediate issues.
10. Monitor and Optimize
Continuously monitor the system’s performance after its launch and gather user feedback to make necessary adjustments and optimize the EHR system for better performance.
11. Evaluate Success against Goals
Evaluate the adoption success against the initial goals and objectives. Consider quantitative metrics and qualitative feedback from users.
12. Setting Realistic Timelines and Milestones
Creating realistic timelines and milestones can help manage expectations, ensure tasks are completed in a logical order, and keep the project on track. The Jelvix team recommends that you divide the EHR implementation process into manageable phases and involve stakeholders from the start for input on each phase.
13. Staff Training and Support
Training your staff will help ensure that all users are competent and confident in using the new system. Different staff members may require different levels of training based on their roles. Make sure to assess individual needs to tailor training programs accordingly. Continuously monitor the effectiveness of training programs and make necessary adjustments.
Explore our detailed case study showcasing the development journey of an innovative EHR solution.
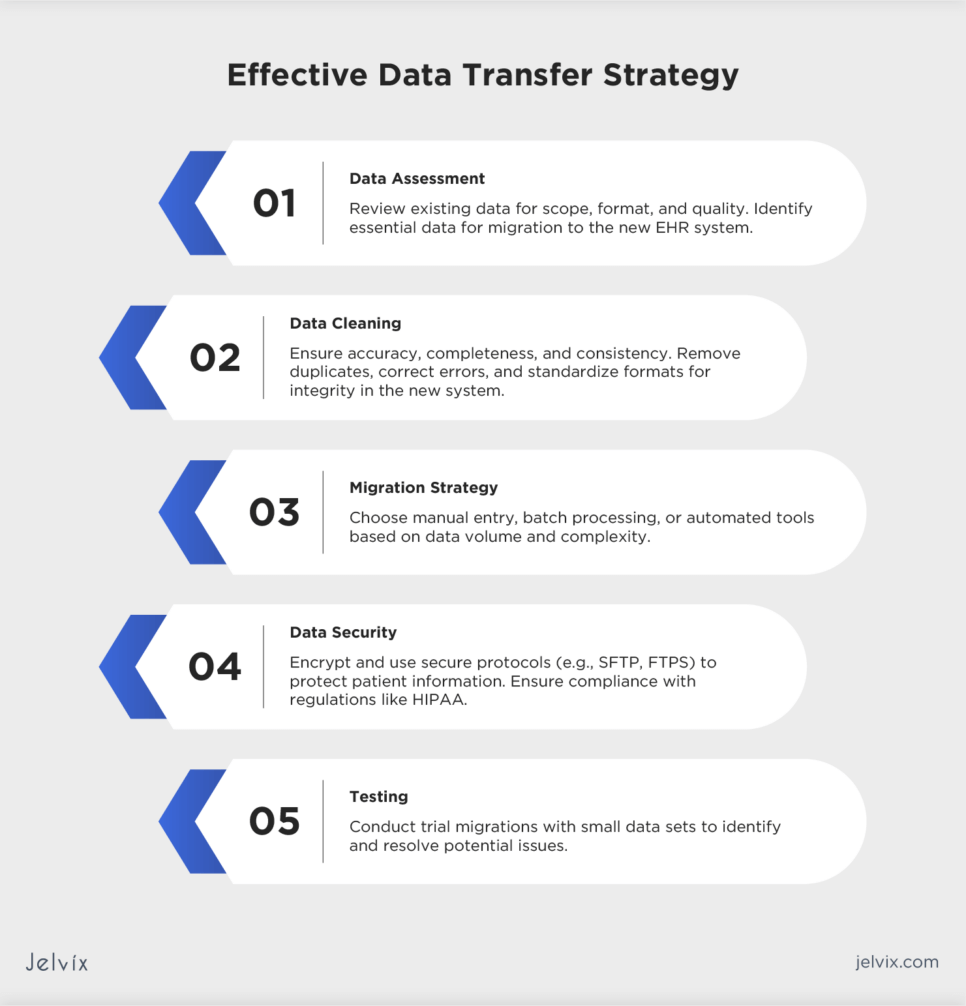
Strategy for Effective Data Transfer
The transition to an EHR system is a process that can be complex and time-consuming. Make sure you follow proven steps to ensure effective data transfer:
- Data assessment: review the existing data to understand its scope, format, and quality. Identify which data is essential and should be migrated to the new EHR system;
- Data cleaning: ensure the data is accurate, complete, and consistent. Remove duplicates, correct errors, and standardize data formats to maintain its integrity in the new system;
- Migration strategy: depending on the volume and complexity of the data, choose between manual data entry, batch processing, or automated migration tools;
- Data security: protect patient information during the transfer by using encryption and secure data transfer protocols, such as SFTP, FTPS, and AS2. Ensure the process complies with all relevant data protection regulations, such as HIPAA;
- Testing: conduct a trial migration with a small set of data to identify potential issues and refine the process.
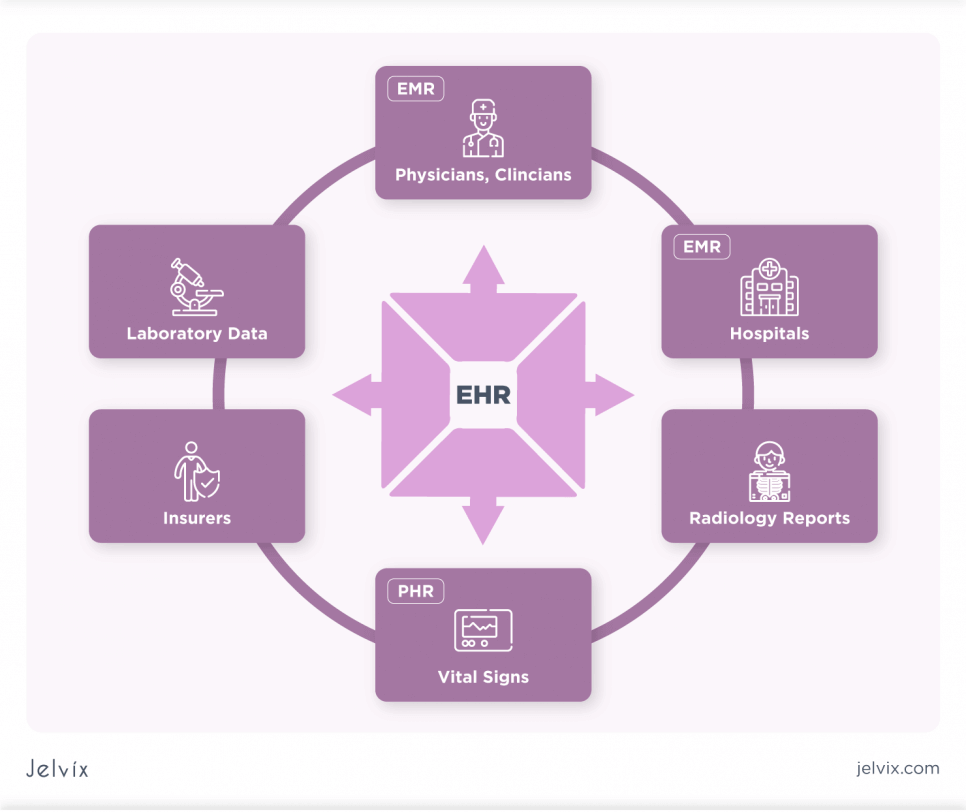
Integrating EHR with Other Healthcare Systems
Integrating EHR with other medical systems enhances care coordination by allowing seamless data exchange across different platforms. Successful integration requires adherence to interoperability standards, robust security measures, and collaboration with vendors to ensure compatibility and compliance with healthcare regulations.
An EHR System Compliance and Security
Protecting patient information and ensuring adherence to regulatory standards is important for gaining patient trust and enhancing care quality. The following best practices will help providers stay compliant and secure.
Regulatory Requirements
Keep up-to-date with healthcare regulations such as HIPAA (Health Insurance Portability and Accountability Act) in the U.S., GDPR (General Data Protection Regulation) in the EU, and other relevant local and international standards that govern patient data privacy and security.
Access Controls
Assign access rights based on user roles, ensuring that individuals can only access the information necessary for their job functions. This will help minimize the risk of unauthorized access to sensitive patient data. Use strong authentication methods, such as multi-factor authentication, to verify the identity of users who access the EHR system.
Data Encryption
Use encryption algorithms, such as AES and RSA, to protect patient data, both when it is stored in the EHR system and when it is being transmitted between systems. This will help prevent data breaches and unauthorized access.
Update and Patches
Regularly update the EHR software and underlying systems to protect against potential vulnerabilities. Implement patches released by vendors on time and conduct regular security assessments and penetration testing.
Response Plan
Develop a comprehensive incident response plan to quickly address any data breaches or security incidents. This should include procedures for containment, investigation, notification, and recovery.
By adopting these strategies, healthcare organizations can safeguard patient information, comply with regulatory requirements, and maintain the integrity of their EHR systems.
Techniques To Encourage EHR User Adoption
Boosting EHR adoption requires early engagement with physicians and patients to customize the system according to their needs. Providing training and offering access to educational resources ensures users remain proficient and confident. It’s crucial to address any technical, cultural, or workflow obstacles to facilitate the use of a new system.
Optimizing EHR for Clinical Use
EHR readiness assessment together with customization, training, and improvement will help optimize the system for clinical use. By focusing on strategies that enhance usability, support clinical workflows, and promote high-quality patient care, healthcare providers can maximize the value of their EHR systems for clinicians and patients.
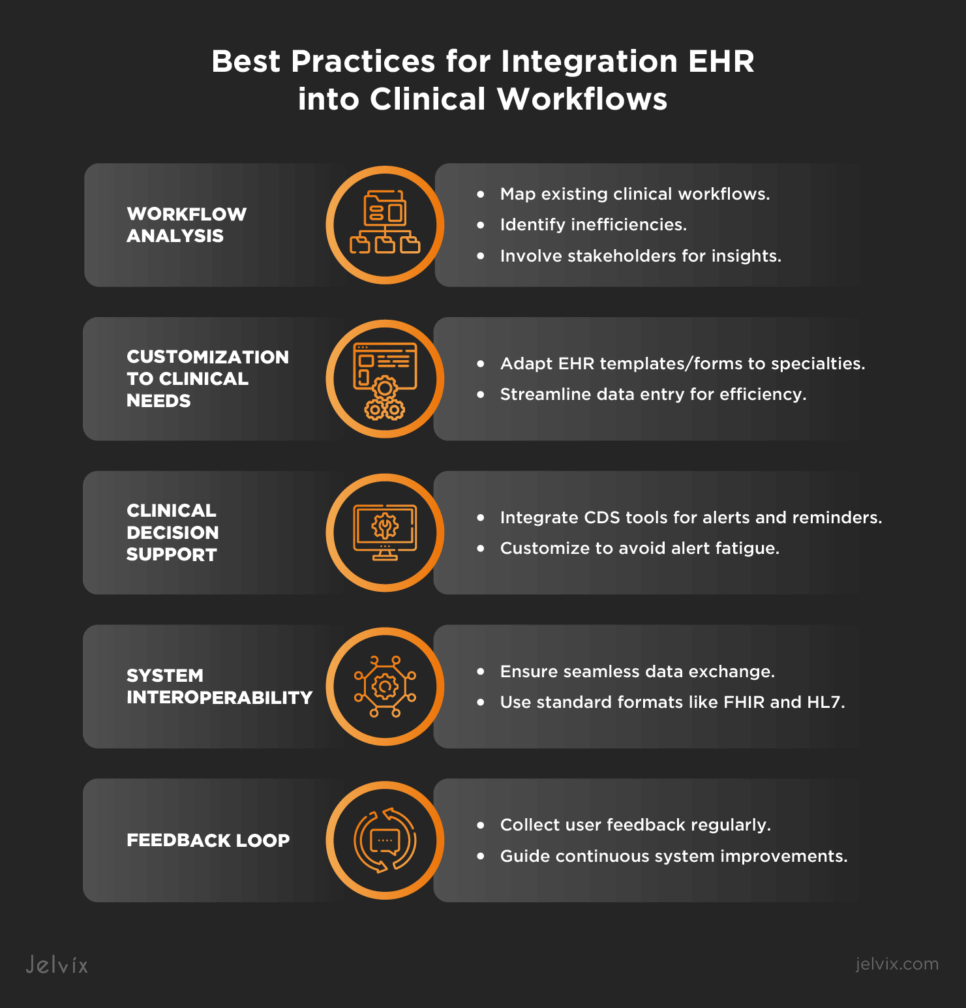
Best Practices for Integration EHR into Clinical Workflows
Following best practices in EHR customization and integrating them into clinical workflows can greatly improve clinical efficiency and boost patient care.
Workflow Analysis
Map out existing clinical workflows to understand how tasks are accomplished and identify inefficiencies. Involving stakeholders in this analysis will help gain insights into their needs and challenges, ensuring the EHR configuration effectively addresses these issues.
Customization to Clinical Needs
Adapt EHR templates, forms, and fields to reflect the documentation needs and preferences of different specialties within the clinic. Streamline data entry to minimize redundant steps that slow down clinical processes.
Clinical Decision Support
Integrate CDS tools that offer alerts, reminders, and access to clinical guidelines at the point of care. Customize them to avoid alert fatigue and ensure that notifications are meaningful and actionable.
System Interoperability
As noted earlier, the EHR should seamlessly exchange data with other healthcare systems. Use standard data exchange formats, such as FHIR and HL7, to facilitate interoperability and data sharing across your medical settings.
Feedback Loop
Regularly collect feedback from users on EHR usability and effectiveness. This feedback should guide continuous improvements to ensure the system meets the changing needs of your entity.
Enhancing Patient Engagement and Access to an EHR
Providing patients with access to their health records fosters transparency and builds trust. When they understand their health status, they are more likely to adhere to treatment plans and engage in preventive health behaviors.
Providers should consider enhancing patient engagement through strategies listed below:
- Implement patient portals: they allow patients to view their health records, lab results, and medication lists at any time;
- Educate patients on tech use: actively teach patients how to use your medical software effectively, highlighting its most useful features;
- Ensure mobile access: enable patients to actively engage with their health information and access it from their mobile devices;
- Promote data ownership: encourage patients to take an active role in managing their health information and highlight the importance of their involvement in healthcare decisions.
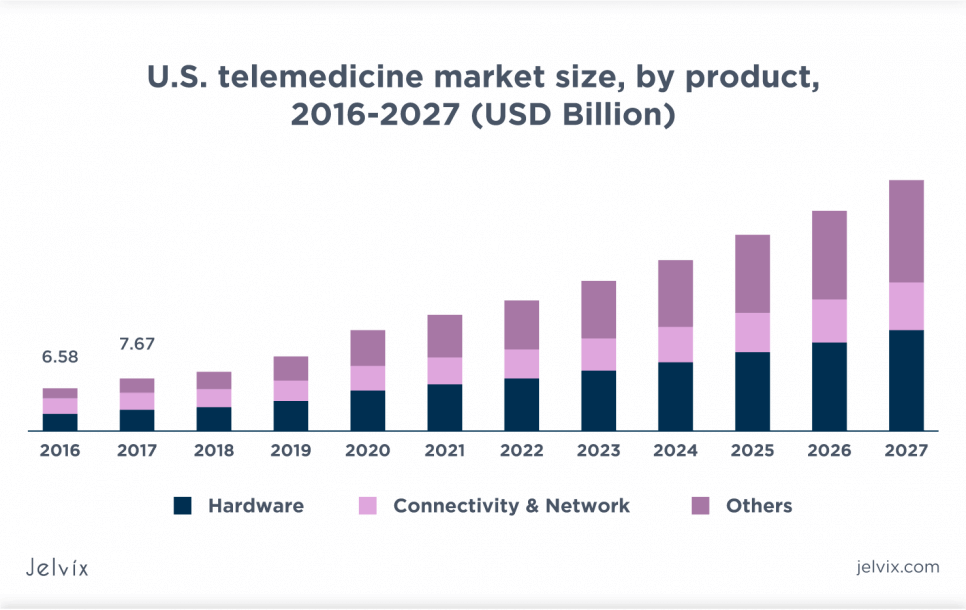
Leveraging EHR for Improved Patient Communication
About 82% of hospitals with basic EHR systems offer a telehealth solution to broaden access to care and enhance doctor-patient communication. Offering a patient portal can be a good idea to support secure messaging on sensitive health issues, while remote appointment scheduling can enable patients to manage their care more effectively.
Evaluating the EHR Impact: Key Metrics and KPIs
Evaluating the impact of EHR systems is vital to ensure they are achieving desired outcomes in patient care, efficiency, and compliance. Key performance indicators provide data that healthcare organizations can use to make informed decisions about EHR system improvements and investments.
Adoption and Utilization Rates
Adoption and utilization rates help measure the level of engagement and active use of the EHR system by both physicians and patients. These metrics typically include the percentage of physicians and patients actively using the EHR system, the frequency of logins, patient portal registrations, and usage rates of specific EHR functionalities, such as documentation and order entry. These metrics help evaluate the effectiveness of EHR integration into daily healthcare practices and the depth of its use by various groups of patients.
Overcoming Common Challenges in EHR Adoption
To unlock the full potential of digital health records, providers should address common challenges that EHR adoption brings along. Overcoming these barriers promotes a smoother transition and enables physicians to deliver better care.
Data Migration Challenges
The process of transferring existing patient records to a new EHR system can be daunting, risking data loss or errors. Meticulous planning and engaging data migration experts will help ensure a smooth transition.
Technical and Usability Issues
Technical problems and poor system usability can impede EHR adoption, affecting efficiency and user satisfaction. Collaborating with vendors for customization and conducting usability testing before full implementation can address these concerns.
Resistance to Change
Users often resist new systems due to comfort with current processes and concerns about the learning curve. Without adequate training, staff may feel unprepared for EHR systems, leading to frustration. Providing detailed, role-specific training and ongoing support helps ensure proficiency and confidence.
Financial Constraints
The cost of EHR adoption, including purchase, implementation, and ongoing maintenance, can be too high for some healthcare providers. Exploring funding options and carefully evaluating the total cost of ownership can help overcome financial concerns.
Case Studies and Lessons Learned
According to the Researchgate report, large and mid-sized hospitals in California adopted EHRs to leverage care outcomes. The adoption was driven by the need to enhance patient care quality, integrate new processes, and comply with health regulations. Both hospitals implemented outsourced modular EHR solutions.
The selection process involved careful evaluation of vendors based on their ability to meet specific requirements, including integration capabilities and cost efficiency. Although they faced typical challenges, such as training, resistance to change, and technical difficulties, the results were satisfactory. The impact of EHR adoption included improved health information management, better decision support, enhanced communication, and patient support.
Future Trends and Evolutions in EHR Technology
As technologies keep developing, ways to enter data into EHR systems transform, too. Researches predict that 90% of U.S. physicians will use AI for data entry and some other purposes.
Another growing trend is integrating EHRs with telemedicine and remote patient monitoring solutions. According to the Insider Intelligence report, more than 70 million U.S. patients will use RPM tools already by 2025.
Finally, the healthcare sector can expect more accurate data integration from wearable devices to EHR systems, as the wearable technology market is projected to reach $428.92 billion by 2030.
A Journey to Digital Transformation with a Tech Partner
Implementing EHRs into healthcare settings can significantly affect both organizational processes and patient health outcomes. Proper implementation enhances patient data management and care quality, while poorly planned integration may provoke obstacles to arise.
At Jelvix, we offer a customized EHR development and adoption approach tailored to your specific needs. Feel free to contact our team if you need expert consultation or support to ensure a seamless transition from paper-based records to EHRs.
Need a qualified team?
Boost your business capacity with the dedicated development team.