Medical billing keeps healthcare running, ensuring providers get paid accurately and on time. However, it has become a bigger challenge as healthcare systems have grown to become more complex. That’s where AI in medical billing changes everything.
Medical billing can get stuck in a world of manual work and errors; with AI, this is no longer the case. Instead, it is getting faster, smarter, and—dare we say—more accurate. AI can identify coding errors in seconds, predict claim denials pre-emptively, and streamline the billing process. It simplifies the complete billing process. These aren’t just enhancements—they’re game-changers for revenue cycle management.
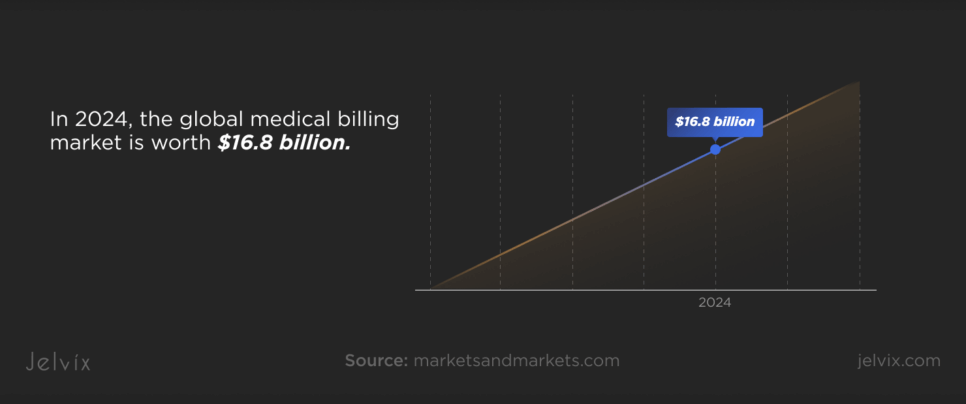
The numbers tell the story. In 2024, the global medical billing market is worth $16.8 billion. By 2029, it’s expected to hit $27.7 billion, growing at a stunning rate of 10.5% annually. What will be fueling this growth? Technology, innovation, and the increasing adoption of AI.
From reducing errors to improving cash flow, AI is redefining what’s possible. In a world where every dollar matters, these advancements are shaping the future of healthcare billing. Want to see how it’s reshaping healthcare payment solutions? Let’s break it down.
What is Medical Billing?
Medical billing is the backbone of healthcare finances. It is critical to ensure that providers are paid for the clinically necessary services they deliver to patients. This process goes far beyond issuing bills; it involves comprehensive work that guarantees accurate claims, proper reimbursements, and financial viability for healthcare organizations.
In its fundamental form, medical billing consists of reviewing a patient’s medical records, identifying billable services, and transforming that information into claims submitted to insurance companies or other payors. This isn’t an easy thing to do; it involves converting medical diagnoses and common procedures into standardized codes, such as CPT and ICD-10. Payors then thoroughly screen these claims to determine coverage, medical necessity, and compliance with their policies. Approved claims result in payments, while rejected ones often need follow-ups or adjustments.
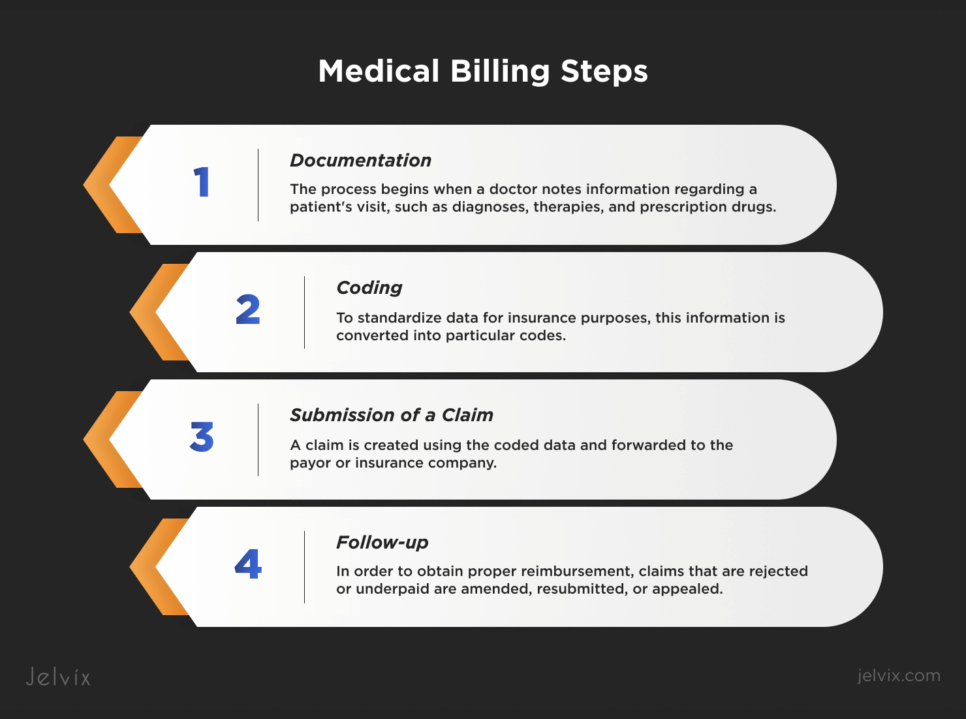
Schematically, we can imagine medical billing in such steps:
- Documentation: The process begins when a doctor notes information regarding a patient’s visit, such as diagnoses, therapies, and prescription drugs.
- Coding: To standardize data for insurance purposes, this information is converted into particular codes.
- Submission of a Claim: A claim is created using the coded data and forwarded to the payor or insurance company.
- Follow-up: In order to obtain proper reimbursement, claims that are rejected or underpaid are amended, resubmitted, or appealed.
Medical billing is not just a payment request; it ensures that healthcare providers are viable. Without it, doctors and hospitals wouldn’t be able to stay in business, let alone invest in new technology or hire the people who will run it. Accurate billing is directly related to the revenue cycle, allowing healthcare providers to concentrate on providing quality patient care instead of chasing after payments.
Mistakes in this process—for example, outdated codes or details gone missing—may cause denied claims, delayed payments, or even financial losses. This is why expertise and precision in medical software development are crucial.
The Human Factor in Medical Billing
Medical billing has long depended on people trawling through codes, regulations, and insurance policies. As important as their expertise is, the human element can also create specific pain points that slow down workflows and can harm a company overall.
Manual billing is a meticulous process. Billers carefully review patient records, select the correct codes, and compile claims meeting insurer requirements. And it doesn’t end there with constant changes in coding standards, insurance policies, and compliance requirements; it keeps getting more demanding. Some of the challenges are listed below:
- Time-Consuming Processes: Manual record review, claims coding, and error resolution are pretty time-consuming and often delay reimbursement.
- Inherent Error Proneness: Mistakes are inherent in even the most skilled billing professionals. Claims can be denied due to missing information, old codes, or even a simple typographical error.
- Stress and Burnout: The repetitive nature of the work and the extreme accuracy requirements put further stress on billing professionals, subsequently affecting their overall productivity.
Errors in manual billing aren’t just inconveniences—they’re costly. Here are some of the most common mistakes:
- Coding Errors: Misusing CPT or ICD codes frequently leads to denied or delayed claims.
- Incomplete Information: Missing patient details, incorrect insurance information, or omitted documentation can cause claims to bounce back.
- Duplicate Claims: Submitting the same claim twice can raise red flags with insurers, complicating the reimbursement process.
- Missed Deadlines: Inconsistent tracking of claim submission and appeal deadlines can result in lost revenue.
This is where AI medical billing comes into play. AI-driven systems remove the bottlenecks of manual processes by automating menial tasks, flagging errors as they occur, and predicting likely claim denials.
How AI Can Be Applied in Medical Billing
AI is shaking up the world of medical billing, turning a traditionally slow and error-prone process into something fast, efficient, and reliable. By leveraging innovative healthcare payment technology, providers can say goodbye to endless paperwork and costly mistakes and hello to a smarter way of managing finances.
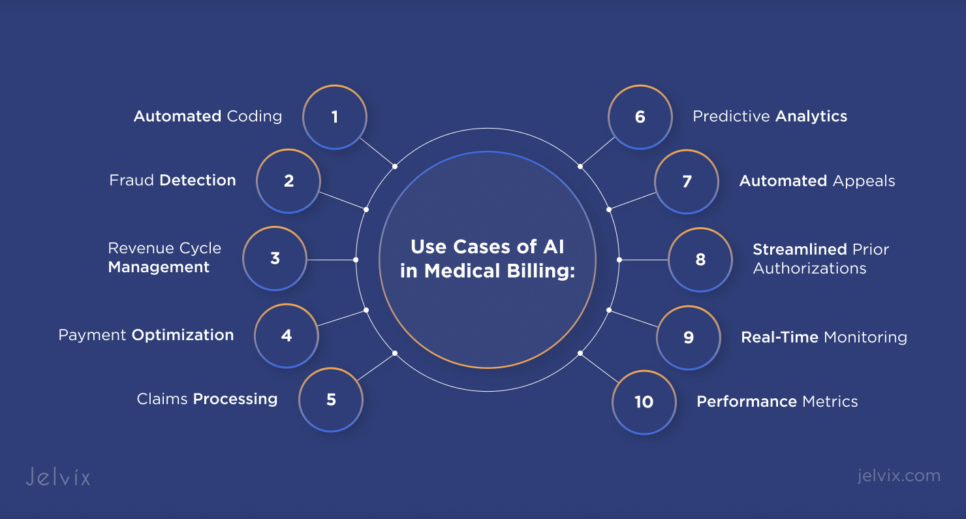
The utilization of AI for medical billing doesn’t know limits. Several use cases include:
- Automated Coding. AI relieves the agony of medical coding. It instantly assigns the correct CPT or ICD-10 codes by analyzing patient records, doctor comments, and procedures. No more endless scrolling through immediate lists or second-guessing; just accurate code in seconds. Not only does this improve efficiency, but it reduces errors, making claims go through much more smoothly.
- Fraud Detection. Fraudulent claims cost healthcare providers millions, but we have an AI solution. It examines claim trends and identifies anything suspicious before it becomes a crisis. Having AI in your court means false claims are flagged and caught almost immediately, which saves time and money.
- Payment Optimization. AI doesn’t just analyze data—it forecasts trends. By processing past payment data, it enables healthcare providers to maximize cash flow, anticipate delays, and plan for future revenue requirements. It’s like having a sleepless financial coach.
- Claims Processing. AI guarantees the accuracy of the claims before they hit the system, identifying minute errors that human sight could have potentially missed. When a process includes automated checks, a rejected claim becomes history, and reimbursement is carried out more efficiently than ever.
- Revenue Cycle Management. AI improves every step of the revenue cycle. It gathers data at each touchpoint—registration, labs, treatment, and prescriptions—so the billing process can be seamless, error-free, and end-to-end.
- Predictive Analytics. AI removes the guesswork from billing. By identifying patterns and spotting potential problems, it can predict whether or not a given claim will be accepted. With this foresight, billers can attend to pre-submission issues, saving time and headaches.
- Automated Appeals. Rejected claims? No problem. AI identifies the errors, corrects them, and resubmits the claims automatically. This permits skipping the tedious manual process, making appeals faster and more efficient.
- Real-Time Monitoring. AI provides real-time updates on claims. Billers receive alerts about potential issues and can resolve them before they cause delays.
- Performance Metrics. AI monitors each stage of the billing lifecycle, creating reports and dashboards to show what is working and what needs to be improved. Providers can utilize these insights to optimize their billing lifecycle and move toward revenue maximization.
- Streamlined Prior Authorizations. Prior authorizations can delay care and infuriate patients. Artificial intelligence automates this process, verifying clinical data against insurance guidelines in real time. This reduces approval times from days to hours, allowing for smoother patient care.
AI is more than a tool—it’s a medical billing software development revolution. It’s addressing challenges that have long tormented the industry: claim errors, delayed payments, and administrative backlogs. Billing with AI is faster, smarter, and more reliable, giving healthcare providers the freedom to do their best—caring for patients.
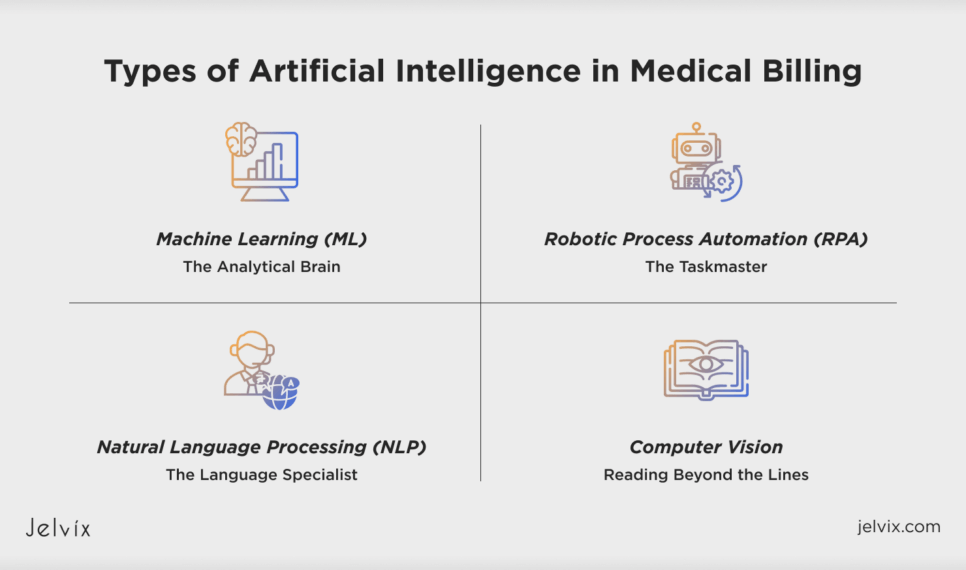
Types of Artificial Intelligence in Medical Billing
Artificial intelligence is diving deep into medical billing with specialized technologies tailored to specific challenges. Every AI type offers unique capabilities that cover the fundamentals and provide real answers to common healthcare billing issues. Let’s explore how these sophisticated tools are shaking up the industry and their place within medical payment solutions.
Machine Learning (ML): The Analytical Brain
Machine learning thrives on data. In medical billing, it becomes a powerful ally by learning from past claims and financial trends to improve processes over time. It doesn’t just process—it predicts, adapts, and refines.
Why It Matters: ML tools identify coding patterns, analyze common claim rejections, and recommend precise corrections before submission.
Example: Train ML software with years of billing data, and it starts predicting how likely a claim is to be denied and why. Fixes happen faster, and billing teams stay ahead of the curve.
Natural Language Processing (NLP): The Language Specialist
Medical notes are often messy, unstructured, and full of jargon. NLP converts this chaos into clear, structured data.
How it Works: Unlike manual transcription, natural language processing reviews doctor notes or patient charts and converts them into billable codes.
Why It Matters: For many industries, having such an NLP (Natural Language Processing) system that underlines main points, checks inconsistencies, and provides corrections (all returned by an NLP bot) could prove to be a huge game-changer, cutting hours off manual coding time and freeing resources to concentrate on the important stuff.
Robotic Process Automation (RPA): The Taskmaster
RPA uses AI-driven bots to handle repetitive, rule-based tasks. In medical billing, RPA is often used for:
- Claim Submission: Automatically filling out and submitting claims to insurers;
- Data Validation: Cross-checking patient data and insurance information to ensure accuracy;
- Follow-Ups: Sending reminders or updating claim statuses without human intervention.
RPA saves time, frees up billers to focus on complex tasks that require critical thinking, and enhances overall productivity.
Computer Vision: Reading Beyond the Lines
Computer vision helps machines understand visual data like scanned images, PDFs, and handwritten notes. In medical billing, this technology excels at:
- Data Extraction from Images: Computer vision software can process scanned medical reports or patient forms within seconds and extract the relevant billing information;
- Feeding Data into EHR Systems: Computer vision processes digital versions of handwritten notes or scanned documents, automatically generating accurate data for electronic health records rather than manually entering it.
Imagine that a medical billing team uploads scanned insurance forms, and moments later, computer vision software locates, interprets, and transfers the data into their billing system—cutting hours of manual entry.
Not only can these AI technologies function independently, but they could also improve one another. For instance, computer vision digitizes paper data for smooth integration, while machine learning can work in tandem with NLP to process patient notes and recommend codes. Because of these developments, all parties benefit from speedier, more accurate, and less stressful medical payment solutions.
Benefits of Artificial Intelligence in Medical Billing
Medical billing is incredibly complex, but machine learning simplifies it due to its unmatched precision. AI tools catch mistakes in code, missing details, or duplication of claims, drastically reducing rejection rates. According to recent research, AI-backed billing systems improve coding accuracy by up to 96% and process claims 10 times faster than traditional workflows.
The speed and accuracy of AI also bring substantial financial benefits. The longer it takes to process a claim, the higher the costs in both time and resources are. AI-powered systems take this on by automating repetitive, entry-level work (like data entry and claim follow-ups) and can reduce billing overhead by up to 30 percent. According to some estimations, processing times for claims are 50–70% faster when wait times are expedited since this results in an accelerated claim payment timeframe.
Blue Cross Blue Shield, for instance, used AI-driven solutions to shorten the previous authorization period from nine days to less than one, which improved cash flow and decreased administrative expenses. Consequently, AI assists healthcare providers in maintaining consistent income streams despite increasing administrative demands by speeding up payment processes.
The impact of AI extends beyond the back office, creating a better experience for both patients and providers.
- For patients, more accurate and prompt billing translates to fewer mistakes in medical bills and speedier dispute resolutions. In addition, AI automates prior authorizations so patients receive care sooner without prolonged delays.
- For Providers: AI streamlines the billing process, allowing billing teams to spend more time with patients. With fewer rejected claims and a standardized reimbursement process, providers can keep their finances in check while still delivering excellent service.
The data speaks for itself: AI medical billing software is improving accuracy, reducing costs, and simplifying procedures in ways manual methods cannot. AI is a lifeline for healthcare providers, not just an improvement. Medical billing transforms from a hassle to a dependable, effective procedure that benefits all parties.
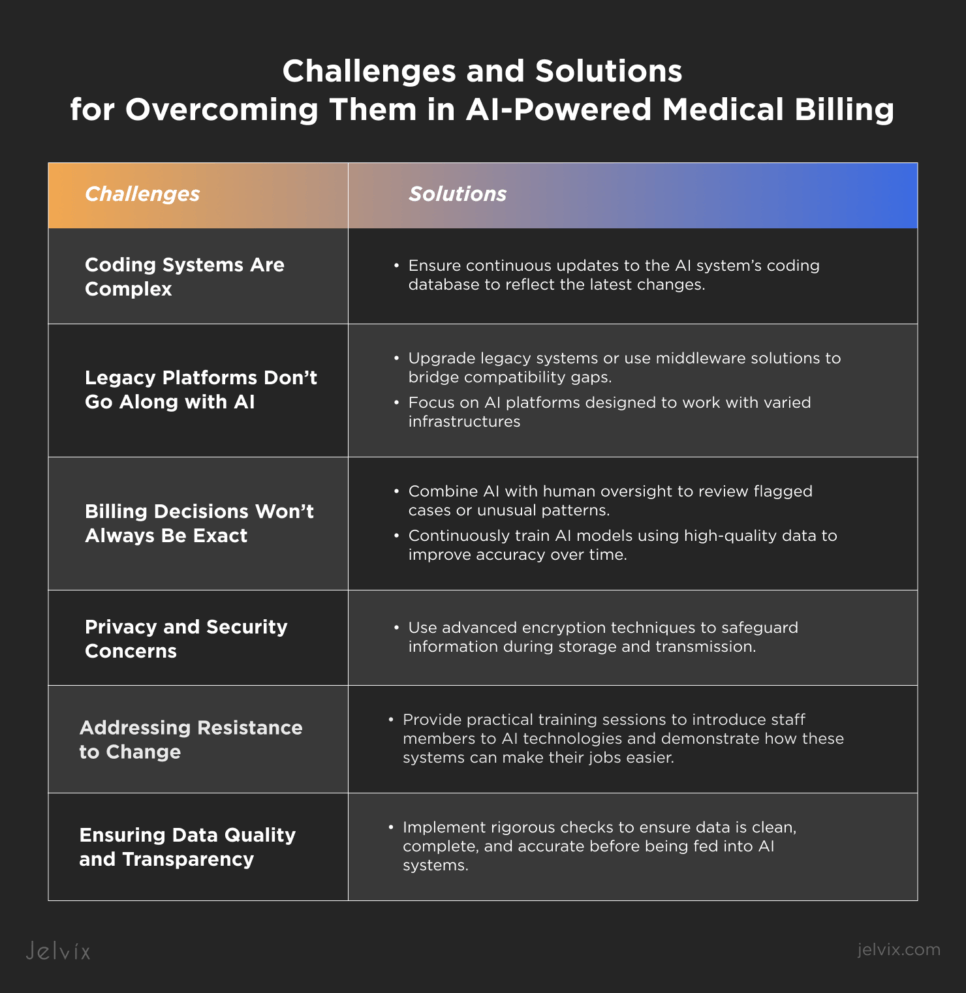
Challenges and Solutions To Overcome Them
AI in medical billing is a game-changer, but like any innovation, it comes with challenges. From privacy concerns to adapting to new systems, there are things to overcome. The good news? Each challenge has practical solutions that can turn potential roadblocks into stepping stones.
Coding Systems Are Complex
Medical billing involves two main sets of codes—ICD-10 and CPT—that are updated annually. AI systems must access the most current coding information to ensure accuracy.
The solution:
- Ensure continuous updates to the AI system’s coding database to reflect the latest changes.
- Partner with vendors that provide real-time updates for coding systems.
Legacy Platforms Don’t Go Along with AI
Older systems in many healthcare practices lack the modern architecture required for seamless integration with AI. This creates challenges in accessing and processing data.
The solution:
- Upgrade legacy systems or use middleware solutions to bridge compatibility gaps.
- Focus on AI platforms designed to work with varied infrastructures.
Different Data Formats Create Sync Issues
Data from different systems may have unique formats, making synchronization challenging.
The solution:
- Standardize data formats across systems to ensure smooth integration.
- Use AI tools that can process and harmonize diverse data inputs.
Billing Decisions Won’t Always Be Exact
AI models are powerful but not infallible. They may misinterpret complex cases or lack the human reasoning for nuanced decisions.
The solution:
- Combine AI with human oversight to review flagged cases or unusual patterns.
- Continuously train AI models using high-quality data to improve accuracy over time.
Privacy and Security Concerns
AI systems are dependent on huge amounts of sensitive patient data. One breach could cause thousands of dollars in losses and damage to patients’ trust in providers. Meeting the requirements of strict healthcare privacy laws, such as HIPAA, is another level of complexity.
The solution:
- Data Encryption: Use advanced encryption techniques to safeguard information during storage and transmission.
- Regular Audits: Conduct routine security audits to identify vulnerabilities.
- Compliance Assurance: Partner with AI vendors who meet healthcare industry standards and provide transparent documentation of their security protocols.
Addressing Resistance to Change
Because employees may find the new technology intimidating or fear losing their jobs, healthcare workers used to traditional billing operations may be reluctant to embrace AI solutions. Even the most sophisticated ones may encounter resistance without adequate support.
The solution:
- Staff Training: Provide practical training sessions to introduce staff members to AI technologies and demonstrate how these systems can make their jobs easier.
- Effective Communication: Emphasise observable advantages like fewer denied claims, quicker payouts, and less administrative work.
- Incremental Implementation: Let employees get used to AI gradually by introducing it into a few processes at first.
Ensuring Data Quality and Transparency
High-quality data is essential for AI systems to generate precise findings. Errors like improper billing codes or denied claims might result from incomplete, out-of-date, or inaccurate data. Additionally, opaque algorithms may breed mistrust if users are unaware of the decision-making process.
The solution:
- Data Validation Processes: Implement rigorous checks to ensure data is clean, complete, and accurate before being fed into AI systems.
- Regular Audits: Periodically review AI outputs to catch and correct errors.
- Transparent Algorithms: Use AI solutions that clearly explain decisions, fostering users’ confidence.
Every one of these challenges offers a chance to get better. Healthcare providers may fully utilize AI in medical billing by resolving privacy concerns with strong security, reducing resistance through efficient training, and guaranteeing high-quality data with robust validation procedures. The outcome? An easy-to-use, effective billing system that helps patients, providers, and the entire healthcare system.
Ensuring Regulatory Compliance with AI
Healthcare is one of the most regulated industries, and for good reason—it handles sensitive patient information that requires the highest level of protection. Laws like HIPAA demand that all patient data systems maintain confidentiality, integrity, and security. Similarly, ethical questions take this even further, and there is an emphasis on transparency and fairness in decision-making.
For AI, this means explaining why and how it processes data and doing so in a way that avoids accidentally creating discrimination or making biased decisions.
But here’s where the difficulty lies: AI systems base their outputs on massive volumes of data, and they often extract that data not from one place but from several sources. However, if these systems are not built with compliance, they risk unintentionally breaking the law.
For instance, an AI tool may help you extract records from the patient database. Still, if by simply having that tool installed, it logs in to records not on your account, whether by accident or sheer malice, and any part of that information is leaked outside the company, you are liable for that breach.
AI’s Role in Supporting Compliance
AI doesn’t merely need to fulfill regulatory requirements–it has the potential to keep healthcare providers in compliance on an active basis. Here’s how:
- Data protection: Using sophisticated AI technologies and algorithms can help encrypt data, monitor access to sensitive information, and flag possible breaches when they occur in real time, making sure that sensitive data remains protected.
- Audit Trails: AI can generate extensive logs of anything it does—who accessed what kind of data, when, and why. This simplifies the compliance process during audits.
- Minimize Errors: Compliance is not only about security; it’s also about accuracy. By automating and codifying validation processes, AI minimizes human error while ensuring compliance with legal protocols.
Building trust with patients, providers, and regulators is more important than simply adhering to the law. Here, AI can be quite helpful by increasing the transparency of procedures. Billing teams can better comprehend how codes were allocated or why a claim was flagged when specific AI systems, for example, can clearly explain their decisions. This openness promotes trust and ensures that moral principles are respected.
When properly developed and applied, AI becomes more than just a tool; it becomes a partner in compliance. It helps healthcare professionals fulfill and surpass regulatory criteria by promoting moral and legal behavior, resulting in an effective and reliable system.
Dive into our case study to see how we developed an AI-powered chatbot designed to streamline clinical operations while prioritizing patient data security and ethical AI practices.
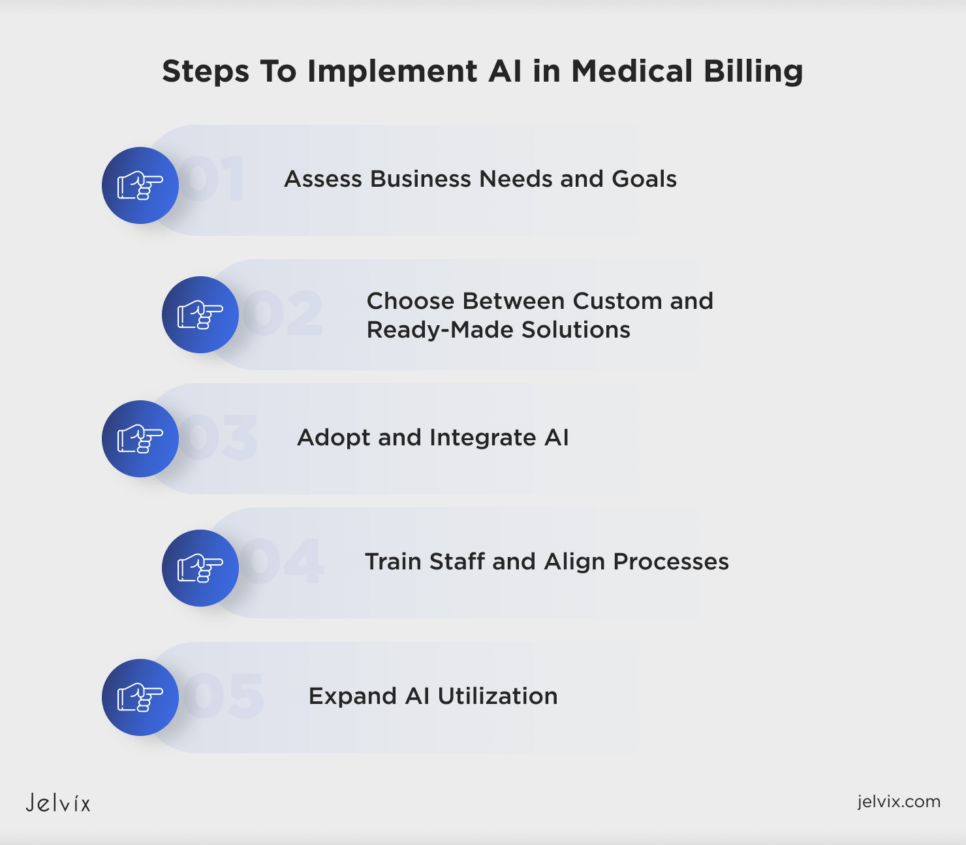
Steps To Implement AI in Medical Billing
Bringing AI into medical billing can feel like a giant leap, but with the right approach, it’s easier than you think. By breaking the process into clear, actionable steps, healthcare providers can ensure a smooth transition to smarter, faster billing. Here’s how to make it happen.
- Assess Business Needs and Goals. Start by understanding the challenges in your billing process. Identify pain points like claim errors, delayed payments, or high administrative costs. Set specific goals, like lowering denial rates or reducing processing times. Such a move will ensure that your AI investment is targeted and driven by measurable outcomes.
- Choose Between Custom and Ready-Made Solutions. Custom solutions are great when possible as they allow flexibility and may resolve unique challenges, but they take much longer and cost more to implement. Off-the-shelf tools are faster to implement and usually have validated features in the market. Your choice will depend on the size of your budget, the amount of time you have to become accustomed to the software program, and the difficulty level of your payment procedures.
- Adopt and Integrate AI. Begin implementing AI into your existing systems, such as electronic health records or billing platforms. Work closely with your IT team or AI vendor to ensure that the new system works perfectly with your existing tools. Tip: Conduct a pilot project first to see if it works for your organization before rolling it out to the enterprise.
- Train Staff and Align Processes. Train your team to leverage the new AI tools correctly. Provide practical training sessions to show how AI can simplify tasks like coding, claims processing, and error detection. Address their worries and emphasize benefits like immediate payments and lighter workloads. Adapt workflows to the AI system as part of the wider transition for all stakeholders.
- Expand AI Utilization. Once the basic functions of AI—automated coding and claim submission, for example—are operating seamlessly, identify more advanced applications. Artificial intelligence can be used as a tool for insightfulness, prediction of payment trends, or facilitation of prior authorizations by analyzing billing data. Continuously assess the system’s performance and seek new opportunities through AI to optimize your billing operational processes.
Medical billing AI implementation doesn’t have to be complicated. You may realize its full potential by taking it step by step, from determining your needs to extending its utilization. With AI in place, you’ll be able to focus more on providing high-quality treatment and less on paperwork.
Why “Now” Is the Time for AI in Medical Billing
Medical billing is at a turning point, and AI is the catalyst for change. The industry isn’t just ready for innovation—it’s demanding it.
Healthcare providers are under pressure to do more with less. Insurance requirements are becoming stricter; patients expect faster resolutions, and administrative costs are ballooning. Meanwhile, the demand for efficiency has never been greater. AI meets these needs, turning slow, error-prone billing systems into seamless operations.
Add to this the post-pandemic digital shift. Organizations everywhere are leaning into automation to manage resources better and eliminate inefficiencies. AI is no longer a luxury; it’s becoming a standard expectation for healthcare providers looking to stay competitive.
The tech itself has evolved. AI is more than “smart”; it is adaptable, intuitive, and scalable. Machine learning, too, can forecast claim outcomes with frightening accuracy. Natural language processing (NLP) scrubs messy doctor notes into clean and ready-to-code data. RPA is a form of process automation technology based on the notion of a virtual robot that facilitates humans in different routine tasks, like follow-ups.
But AI tools are becoming more widely available, too. You don’t have to be a tech giant to adopt them. Simplified cloud-based solutions mean even the smallest clinics can access this transformative technology without spending an arm and a leg. Which results in bridging the gap between high expectations and limited resources
The question isn’t whether AI will dominate medical billing—it’s how soon. The future is one where claims are processed in minutes, not days. Rejections are rare, and payments flow smoothly. AI will push medical billing beyond simple automation to true optimization.
The best part? AI doesn’t just fix problems; it anticipates them. From reducing claim rejections to enhancing cash flow, it transforms the way medical billing works, ensuring providers stay ahead in an industry that never stops evolving.
In a world of rising challenges, AI is your best ally in medical billing. Jelvix offers more than technology—we provide a partnership built on deep industry knowledge and proven results. Let’s take your billing process to a new level of precision and reliability. Connect with us and explore how we can make AI work for you.
FAQ
Can AI handle complex billing cases?
Yes, AI can handle even the trickiest billing situations. It quickly analyzes medical records, understands detailed coding rules, and processes complicated cases accurately, all without missing important details.
Is AI cost-effective for small healthcare practices?
Definitely. AI saves small practices money by automating repetitive tasks and reducing billing mistakes. This means they can do more with less staff, making AI an affordable option for improving efficiency.
How does AI improve accuracy in medical billing?
AI makes billing more accurate by automatically filling in data, spotting mistakes, and using the right codes based on medical records. This helps reduce rejected claims and speeds up payments.
How secure is AI in handling sensitive patient data?
AI systems are built to keep patient information safe. They use encryption, secure storage, and follow strict rules like HIPAA to make sure data stays private and protected.
How does AI impact the patient experience in billing?
AI makes billing easier for patients by speeding up the process and reducing mistakes. Patients get clear and accurate bills, which means fewer problems and a better overall experience.
Need a high-quality professional?
Boost your business capacity with the dedicated development team.