Technological innovations have flooded every aspect of our lives. The healthcare industry is no exception. News about robots performing highly complicated surgical procedures or applications forecasting disease risks can barely surprise an average person.
Paradoxically, with all the advantages of technologies, healthcare organizations continue to suffer from siloed data, disjointed software, and the inability to safely share patient information.
The lack of medical data exchange slows down internal and external workflows in medical institutions, creates gaps in patients’ health records, and even leads to medical errors. And the recent global health crisis has only highlighted the need to connect healthcare platforms.
In order to improve the quality of care and bridge gaps among isolated systems, the fundamental focus of the government initiatives has shifted to ensuring healthcare interoperability and advancing data sharing.
Thanks to all these factors, the global market of interoperability in healthcare is expected to grow from $2.9 billion in 2021 to $5.7 billion by 2026, at a CAGR of 13.9%.
In this article, we define interoperability in healthcare and take a closer look at its levels, benefits, standards, and barriers to implementation.
What is Interoperability in Healthcare?
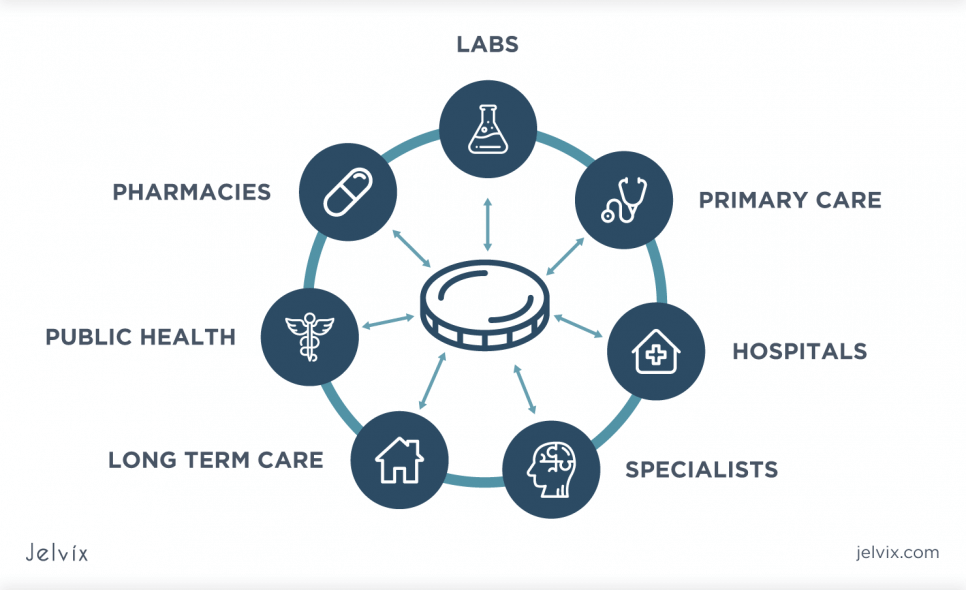
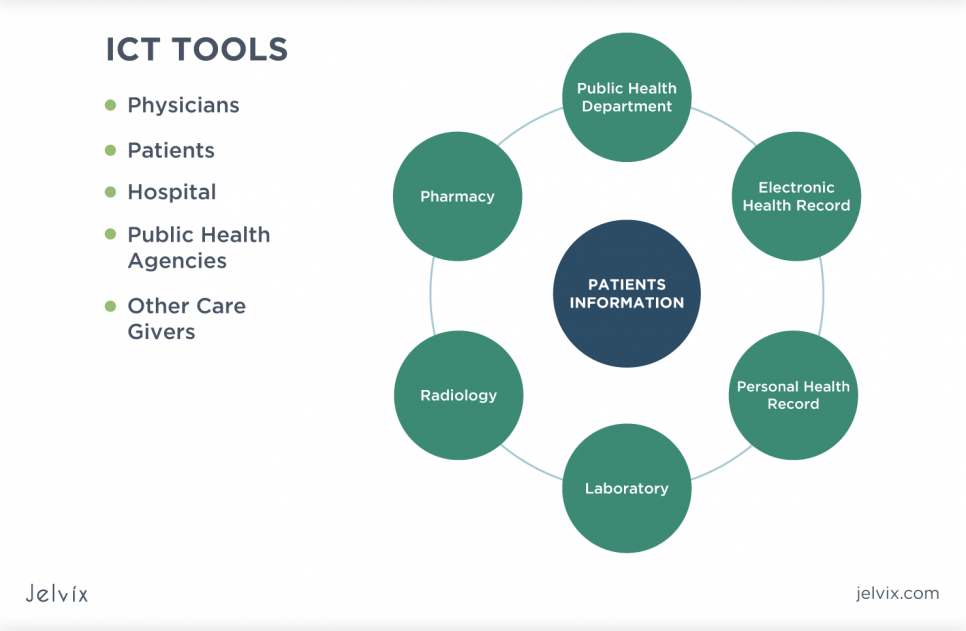
As stated by Health Information and Management Systems Society (HIMSS), interoperability refers to the capability of different medical devices, technologies, and applications to exchange, access, and use health data cohesively.
In other words, interoperability aims at making systems communicate with each other. It presupposes seamless data sharing among hospitals, pharmacies, clinics, laboratories, etc.
Basically, healthcare interoperability is achieved through the use of data exchange frameworks and interoperability standards. They enable sharing of data across different systems, irrespective of the software or vendor.
Fully interoperable systems create holistic and complete patient records that can be used across various organizations. In this way, healthcare providers gain the ability to make data-driven, balanced decisions and provide faster and high-quality care to patients.
Levels of Healthcare Interoperability
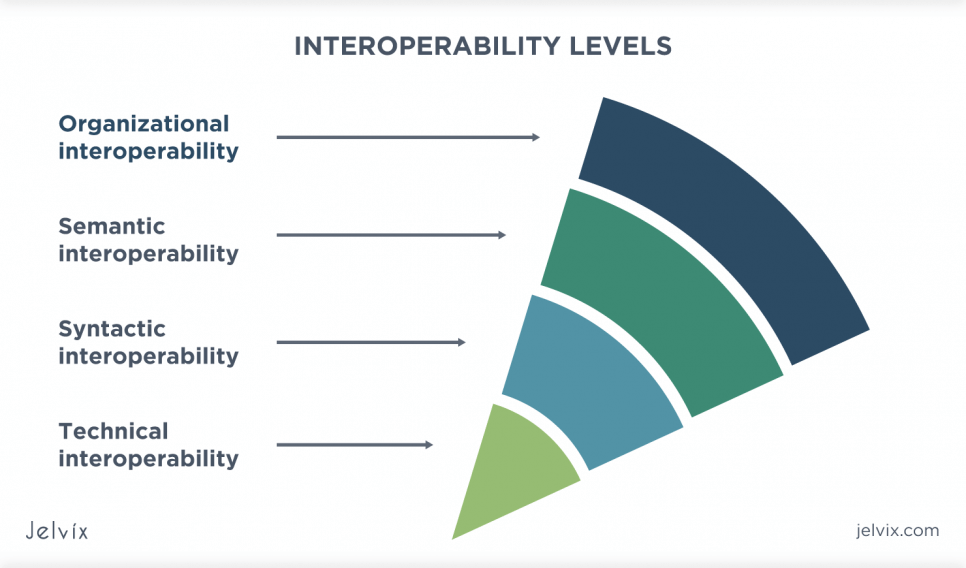
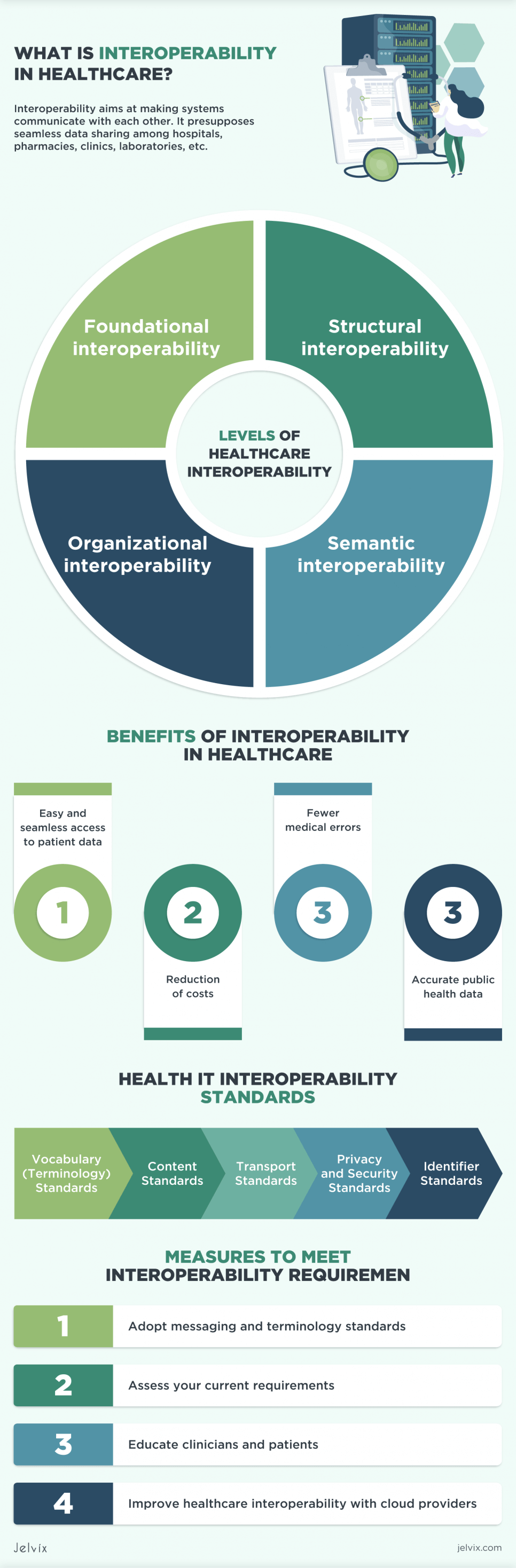
According to HIMSS, these are the following levels of interoperability in healthcare:
– Foundational interoperability. This level is the basic one. It involves the ability of one system or application to receive and communicate data to another in a secure way.
The foundational interoperability does not require the receiving application to be able to decipher or interpret data. Instead, it means that the receiving machine only stores the data that has to be further processed by the receiving physician, clinical laboratory technician, pharmacist, patient, etc.
– Structural interoperability. This level is more complex than the previous one. It implies that the exchanged data can be interpreted at the field level by the sending and receiving machines.
Both systems require the adoption of uniform syntax, organization, and format standards for healthcare data exchange to achieve structural healthcare interoperability. These standards also ensure that the clinical and operational purpose of the exchanged information remains unaltered and preserved at the field level.
– Semantic interoperability. This level is one of the highest interoperability levels. It allows authorized parties to exchange, interpret and utilize healthcare information fully.
Semantic interoperability in healthcare presupposes the use of common, unified models for data codification that allow both systems to interpret data correctly. The electronic data exchange at this level improves the quality and safety of healthcare delivery.
– Organizational interoperability. This level covers social, legal, policy, and organizational components of interoperability. It entails the integration of interoperability into the workflows and processes of an organization.
Together with the technical requirements of the previous levels, organizational interoperability aims at promoting seamless, secure, and accurate data exchange between healthcare organizations and clinicians.
Benefits of Interoperability in Healthcare
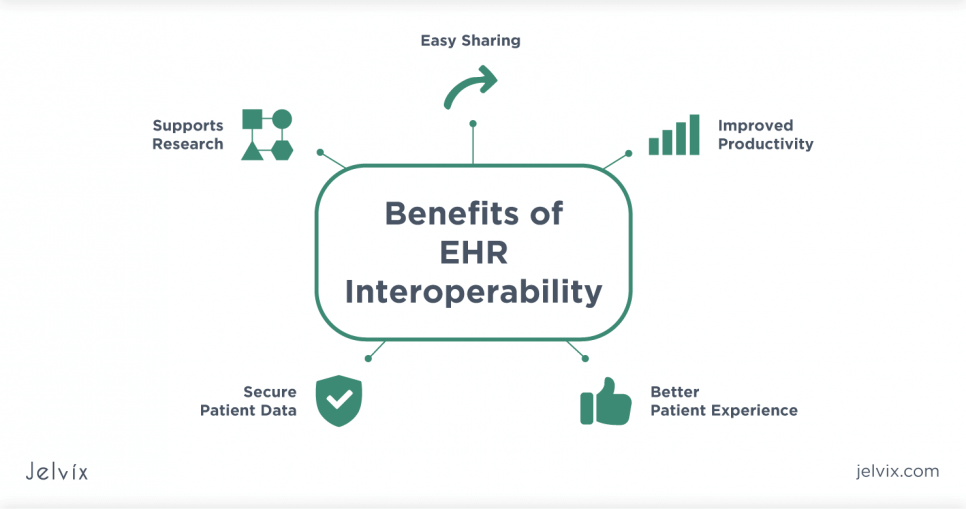
There’s no need to mention that healthcare relies on having the right data at the right time as no other industry. Adopting interoperability in medical practice can ensure quick and seamless access to information. It will also positively influence diagnosing, treatment, ongoing care, and patient outcomes.
Here are several benefits that come with smooth and effective data exchange:
-
Easy and Seamless Access to Patient Data
An average patient tends to use a wide range of healthcare providers, including hospitals, urgent care centers, pharmacies, laboratories, solo physicians, etc. When changing providers, patients are supposed to either bring their health records with them or fill out the documents with their medical history in each healthcare institution.
In these situations, the health data may get lost and be incorrectly or incompletely identified by patients. All of this leads to patient data fragmentation that has negative effects on the continuity of care. Not to mention its detrimental consequences in case of emergency when every second matter.
Healthcare interoperability provides a complete and clear picture of patient data to multiple healthcare givers. By seamlessly exchanging data between healthcare systems and providers, clinicians will be able to make balanced medical decisions, provide better treatment and save many resources.
At the same time, the complete history of prior treatment, medications, and procedures allows the new doctor to start treatment immediately from the point where the previous one left off.
With interoperability in place, the providers and patients gain timely and secure access to health records regardless of the system or geographical locations.
-
Reduction of Costs
The financial impact of interoperability is also immense. Effective data sharing among various healthcare stakeholders helps prevent a lot of adverse drug events and workflow inefficiencies.
Firstly, successful communication among applications reduces the amount of redundant testing caused by the inaccessibility of patient’s data. According to the research, it will save up $3 billion annually.
Secondly, healthcare interoperability lowers the amount of time allotted for manually filling in the data into the system. Consequently, it results in improved productivity of clinicians and better workflows in the organization.
Thirdly, fast and smooth data exchange decreases the length of stays due to delays in information transfer. Doctors do not have to wait for the laboratory to send paper-based tests. With complete interoperability, these data are automatically transmitted and updated across platforms.
-
Fewer Medical Errors
When it comes to healthcare, medical and medication errors can, at times, be a matter of life or death. Clinicians will agree that the lack of real-time access to medical history or lab results can sometimes pose serious health threats.
Interoperability guarantees a high level of data accuracy by eliminating human factors and limiting the risks of mistakes. The records transferred across disparate applications meet the international data standards in healthcare. These standards ensure that the structure and content of data will be interpreted correctly.
-
Accurate Public Health Data
Smooth healthcare data sharing improves health reporting and monitoring in case of a crisis. By connecting the clinic’s internal software to the healthcare networks used for research, the care providers may help scientists to conduct studies on the effectiveness of treatment and medication methods.
What is even more, full data visibility allows preventing or lessening the effects of the epidemiological outbreaks. It enables researchers to evaluate the scope of the health crisis, find the most effective ways of resolving it, and communicate this information to all healthcare organizations faster.
Health IT Interoperability Standards
Like in any other industry, data exchange in medicine is governed by a range of standards. Interoperability standards provide a common set of rules for transferring and interpreting patient data across various systems.
Interoperability standards are developed, updated, and maintained by a wide range of different standard development organizations (SDOs). Creating an interoperability standard is usually a complex process involving collaboration with experts and healthcare stakeholders that will actually adopt the standard.
According to HIMSS, all currently available interoperability standards can be subdivided into the following types:
Vocabulary (Terminology) Standards. The vocabulary standards aim to ensure that both sending and receiving machines will interpret the medical concepts without ambiguity.
According to these standards, health and clinical concepts (such as diseases, diagnosis, medications, etc.) are represented by structured sets of codes and terminologies. The standards guarantee that the health data will be interpreted correctly by all the systems.
Among the most popular vocabulary standards are SNOMED-CT (intended for clinical terms), LOINC (intended for laboratory and clinical tests), CPT (intended for billing procedures), and ICD-10 (intended for diseases and injuries).
Content Standards. These interoperability standards are geared towards unifying the structure and location of the content in shared documents. They also indicate common sets of data that should be used in specific types of messages.
The most widely used content standards include Consolidated CDA (C-CDA) and HL7’s Version 2.x (V2). They allow streamlining inter-provider and provider-patient communication by specifying the semantics and organization of exchanged documents.
Transport Standards. These standards contain specifications for data format, architecture, templates, user interfaces of electronic messages that enable smooth data sharing across systems. In this context, a message pertains to the unit of information transmitted from one software to another.
Transport standards enable interoperability by using push and pull approaches to health data exchange. The common examples include DICOM (intended for transmitting medical images), Direct Standard (intended to carry C-CDA formatted data), and FHIR (that uses RESTful APIs to share documents in XML, JSON, or RDF formats).
Privacy and Security Standards. These interoperability standards address the issues of patient data safety and security. They are aimed at defining who, when, and with what purpose can collect, access, process, and disclose patient health data.
Privacy and security standards are established by two main laws. In the USA, the Health Insurance Portability and Accountability Act (HIPAA) sets standards that protect health information privacy.
In the EU, the General Data Protection Regulation (GDPR) establishes the privacy and security regulations related to information storage and processing in all areas, including healthcare.
Identifier Standards. These standards relate to universal methods of identifying healthcare providers and patients across various platforms.
Among the examples are EMPI (used to maintain patient’s records in healthcare organization), MRN (used for keeping patients’ history throughout their stay in a hospital), NCSBN ID (intended for verifying nurse licenses), and National Provider ID (NPI) (representing the 10-digit identifier for healthcare providers).
Barriers to Interoperability in Healthcare
While there is no question that healthcare interoperability offers a range of benefits both for clinicians and patients, the process of its achieving is challenging for many healthcare organizations. Let’s take a closer look at barriers that impede interoperability in healthcare.
-
Resistance to Change & Information Blocking
Despite all the innovations in healthcare, this industry still heavily relies on paper-based records. And though maintaining paper-based records is error-prone, a huge number of healthcare providers confront adopting electronic health records. The major reasons for resistance are:
– the lack of administrative IT support;
– the limited ability of different systems to talk to each other;
– patient data security and privacy concerns.
And even when interoperable electronic systems are implemented, a new issue called information blocking may arise. There have been many cases in practice when healthcare providers hampered the electronic health data exchange by demanding money for it.
Much effort was made to address these two issues. The final rules introduced by the US Department of Health and Human Services (HHS) aim at promoting efficient access to health information and pose financial penalties for information blocking.
-
Lack of Consistency of Healthcare Standards
Another barrier to achieving interoperability in healthcare is related to the lack of a single standard for data exchange. Different healthcare organizations use different and sometimes even multiple data sharing standards.
Separate systems are not able to interpret exchanged information properly if the files use mismatched fields or fonts, for example. To prevent this, the information has to be checked and converted into the correct format before it is transmitted into another system.
-
Legacy Systems
Legacy systems can be found in many healthcare organizations. Most of the time, these systems are designed for specific tasks and have minimal network connectivity.
Built with the help of outdated programming languages, they are difficult to maintain and adjust to meet present standards. Therefore, their use significantly hinders healthcare digitalization and interoperability.
-
High Implementation Costs
Achieving healthcare interoperability often requires developing and optimizing multiple interfaces that have to work with a number of different systems. The cost of implementing all standards and building customized interfaces may become a prohibitively high barrier, especially for smaller practices.
The recent CMS estimations show that the cost of API implementation and maintenance only can reach about $1.6 million per healthcare organization.
Read more about the role of the app development companies in medical diagnostics.
Measures to Meet Interoperability Requirements
Although the transition to a fully interoperable healthcare system is a complex process, hindered by many factors, the following measures may help to meet interoperability requirements in your healthcare organization.
- Adopt Messaging and Terminology Standards
Unified semantic terminology and standards for data messaging are crucial for achieving full interoperability in the healthcare domain. Standardization of content and format of health-related data will allow different systems to interpret shared information correctly.
What’s even more, the common standards for semantics, format, and structure of shared laboratory tests, medication, or diagnosis details will make data more understandable for patients and care providers.
- Assess your Current Requirements
Before plunging into healthcare interoperability implementation, it is a good practice to think about the cases in which information will be shared, determine what type of data is exchanged (clinical or non-clinical), what parties will participate in the exchange and what they will do with this information.
This will help you see whether you need to build your own interoperability solution or you can make use of the existing options. Moreover, it will aid in defining the technological approach to data exchange (a point-to-point connection, portal, etc.) and the standards to adopt.
- Educate Clinicians and Patients
Healthcare providers and patients should be taught how to use health tools in proper ways. As sharing health data presupposes some security issues, both parties should understand the benefits and potential dangers related to the health-data exchange across platforms.
- Improve Healthcare Interoperability with Cloud Providers
In healthcare, data – be it text, note, image, prescription, lab results, etc. – is generated exponentially. As the volume of information increases, healthcare providers face the need to invest more in internal equipment to store health records.
One of the ways to reduce cost expenses is by using cloud storage providers that support FHIR services. They serve as a medium that allows exchanging data between applications in a scalable and low-cost computing environment.
The leading IT corporations such as Google, Microsoft, IBM, Oracle are providing sets of cloud tools to foster interoperability and help caregivers, patients, developers, and everyone who deals with healthcare data.
Among the most popular and secure cloud services are IBM FHIR Server, Azure API for FHIR, Oracle Healthcare Data Repository, Google Cloud Healthcare API, and Connected Consumer Health Solution.
Final Thoughts
Modern healthcare is a data-driven industry that heavily relies on seamless and timely access to health records. To remain truly effective, every healthcare organization has to adopt interoperability in its workflows.
By achieving interoperability, healthcare providers enable smooth data flow across platforms without user intervention. As a result, it brings a range of benefits, including significant cost savings, reduction of errors, the ability to make timely, balanced decisions, and 24/7 real-time access to health records.
Interoperability in healthcare is essential for creating a connected and efficient healthcare ecosystem, where data flows seamlessly between different systems and providers. Jelvix’s Healthcare software development services are at the heart of this transformation, ensuring that healthcare organizations can share, interpret, and utilize health data to its full potential.
However, incorporating interoperability is a complex process that may contain a lot of potential pitfalls. Therefore, if you want to avoid the development of complications and start reaping the benefits of fully interoperable healthcare systems as soon as possible, we recommend that you take advantage of professional IT experts.
Our team of developers has extensive experience in building medical solutions and is always ready to consult and help with implementing technologies in your organization. Just drop us a line, and let’s head for interoperability adoption together.
Need a qualified team?
Access the talent pool, start digital transformation now.