The HITECH Act led to a huge increase in the use of digital technology in U.S. healthcare. According to the Office of the National Coordinator for Health Information Technology, 96% of hospitals and 78% of doctors’ offices had switched to certified EHRs, turning once-disorganized paper records into useful data assets.
Healthcare interoperability—the capacity to easily share data between different systems—still eludes us, even if progress has been made. Fewer than one in three hospitals in the U.S. can electronically find, send, receive, and combine patient data from external sources. Transitions of care still typically use paper or fax, which leaves dangerous gaps in patient information and makes professionals’ work less efficient.
Europe has similar problems. Not many EU hospitals can share patient data with other organizations. Cross-border exchange is even less developed, especially with governmental pushes like the European Health Data Space (EHDS). Different standards, private systems, and broken implementation still make it hard for data to flow freely across both national and regional healthcare systems.
These interoperability gaps are especially expensive for rehabilitation treatment, where outcomes depend on coordinated team involvement and smooth care transitions. IT systems that aren’t connected properly make clinicians’ jobs harder, put patients at greater risk, and squander an estimated $36 billion a year in the U.S. alone.
In the following sections, we’ll discuss what “true interoperability” entails, its significance in rehabilitation, where current systems still fall short, and the new strategies—technological, operational, and regulatory—that can help bridge the gap.
What Is True Interoperability?
“Interoperability in healthcare” is a widely used term, but not always a well-understood one. The industry too often sees any kind of data interchange, no matter how small or manual, as proof of progress. Sending a CCD through a gateway or downloading a PDF into an EHR is not enough for true interoperability.
The 21st Century Cures Act gives a better definition: interoperability must allow electronic health information to be accessed, exchanged, and used across different systems without any extra effort from the user and without any artificial obstacles like information blocking.
That bar is still high in practice. A lot of post-acute care software can import a clinical summary, but they can’t combine separate pieces of data, like functional scores or therapy progress notes, into a long-term patient record.
Many EHRs for acute care can send data out, but they can’t easily combine data that comes in from rehab or long-term care partners. These gaps are caused by both technical problems and the fact that different vendors and care settings have different ideas about what interoperability means.
Levels of Interoperability
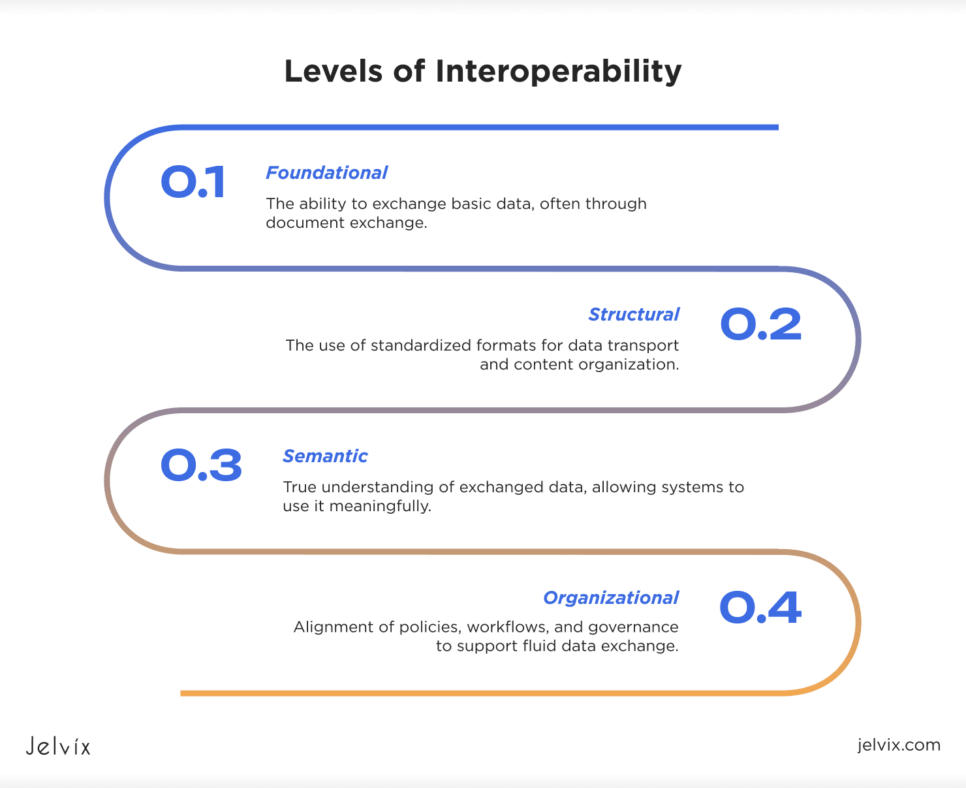
The industry commonly recognizes four levels of interoperability:
- Foundational: The ability to exchange basic data, often through document exchange.
- Structural: The use of standardized formats for data transport and content organization.
- Semantic: True understanding of exchanged data, allowing systems to use it meaningfully.
- Organizational: Alignment of policies, workflows, and governance to support fluid data exchange.
Most of the time, EHR interoperability solutions work on both the foundational and structural levels. Very few systems can really work together semantically, especially in acute and post-acute settings. This is where purpose-built post-acute software is really important.
It needs to fill in technical gaps, make data consistent across different systems, and help coordinate care that goes beyond the walls of any one organization.
Why Interoperability Matters in Post-Acute and Rehab Settings
Post-acute interoperability is not a minor issue; it is essential for the quality, safety, and efficiency of treatment. Patients moving to rehab, skilled nursing, or home health facilities typically have complicated medical histories, such as polypharmacy, going to therapy, having trouble moving, or having other health problems.
Yet too often, their information arrives incomplete or late. Missing treatment records, gaps in prescription lists, or delays in functional assessments might all cause bad occurrences, extra tests, or therapy plans that aren’t as good as they could be.
The effect on finances is considerable. Inconsistent documentation in fragmented post-acute care leads to unnecessary hospital readmissions, longer rehab stays, and more denied claims. In the U.S., one in five Medicare beneficiaries discharged from acute care to a post-acute setting is readmitted within 30 days.
Many of these readmissions are due to problems with coordination. Lost bed days due to late referrals and incomplete discharge data make revenue loss worse for both acute and post-acute providers.
Interoperability has a direct impact on the patient experience at the clinical level. For true patient-centered care to work, there needs to be data transparency. Patients and their families need to be able to comprehend the treatment plan, see how things are going, and talk to each other across care teams.
But many rehab providers use separate EHRs or standalone post-acute software, which makes it hard for patients to see the whole picture of their health journey. Not only is closing these data gaps a compliance goal, it’s also necessary for contemporary, responsible post-acute care.
Interoperability Market Landscape in 2025
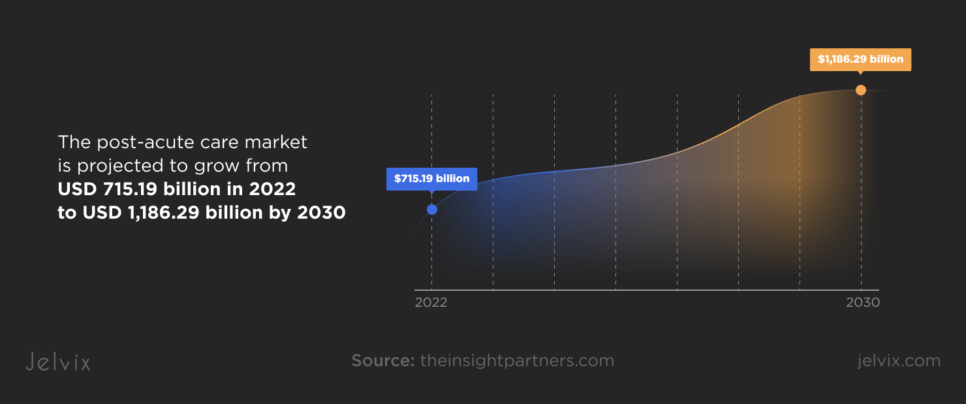
The post-acute care market is projected to grow from USD 715.19 billion in 2022 to USD 1,186.29 billion by 2030, at a CAGR of 6.5%, according to Insight Partners. As this market expands, demand for advanced rehabilitation technology and interoperable post-acute software is accelerating.
But this increase isn’t even: big hospital networks spend a lot of money on modern rehabilitation equipment and enterprise EHRs, but many smaller post-acute providers still use outdated technologies or systems that don’t work well together.
Interoperability in post-acute care is still a big problem. Less than 40% of post-acute providers can easily share structured data with upstream acute care EHRs. Cross-sector interoperability is even worse in Europe. Without smooth data flow, care transitions remain vulnerable to mistakes, delays, and patient dissatisfaction.
Regulatory pressure is mounting. The 21st Century Cures Act and the CMS Interoperability and Patient Access Rule in the U.S. are making it more and more necessary for open data sharing to happen not just in hospitals, but all throughout the continuum.
Rehabilitation providers will not be exempt. Increasingly, rehabilitation EHRs must work with national health information networks like TEFCA. At the same time, payers, especially Medicare Advantage plans, are pushing for the use of quality criteria that rely on interoperable data, such as tracking therapeutic outcomes and functional status.
Payers and provider networks are very important. Many accountable care organizations (ACOs) now require the software partners of rehab centers to be able to provide data in real time for episodes of care. Bundled payment models make interoperability even more appealing.
If health systems can’t see how therapy is going and how the patient is doing, they could face financial penalties based on post-acute outcomes.
At the same time, the vendor landscape remains fragmented. Some rehab software platforms, especially those that deal with scheduling for inpatient and outpatient treatment, still don’t have current API frameworks or FHIR-native architectures. A lot of rehabilitation vendors have only concentrated on billing or paperwork, which has left big gaps in their capacity to work with other systems.
But the leaders in the market are evolving. Both new companies and existing EHR suppliers are putting money into creating EHR connection layers, modular APIs, and cloud-based data hubs that are meant to fill in these gaps that have been there for a long time.
The Role of EHRs in Post-Acute Interoperability
Many acute care EHR vendors have not paid enough attention to the special needs of rehabilitation facilities in the past. It is not common for acute EHR systems to have data items that are easy to convert to post-acute care EHR. These include tracking functional status, therapy intensity, mobility progression, and psychosocial metrics across time.
Rehab workflows also require a lot of paperwork from many teams, such as PT, OT, speech therapy, nursing, and case management. Because of this, even systems that are theoretically “integrated” typically don’t put rehab data together in ways that make sense for clinical use.
Even when industry standards are in place, EHR interoperability challenges persist. An increasing number of individuals are using FHIR interoperability frameworks; however, the fact that various vendors implement FHIR in different ways makes it hard to have meaningful semantic exchange.
For instance, an acute EHR might use FHIR Observation resources to send functional status, but a rehab software might not have the right fields or normalization logic to take in and show this data properly. As a result, doctors and nurses in the post-acute setting still have to rely on scanned papers or manual abstraction, which makes care transitions even more challenging.
Many post-acute EHR solutions also have issues with bidirectional interoperability. It is common for rehab centers to receive structured admission data from acute partners, yet lack mechanisms to return timely, granular progress updates. This impedes not only clinical visibility but also payer-required reporting under value-based models.
Closing these gaps will require more than basic data transport; it demands purpose-built mappings, smarter APIs, and deep collaboration between EHR vendors across the acute and post-acute sectors.
Where Rehab Centers Are Still Disconnected and What It Costs
The reality on the ground: Many rehabilitation centers still operate with fragmented EHRs that are poorly integrated with upstream acute care systems. Discharge summaries may arrive as scanned PDFs. Medication lists may require manual reconciliation.
Therapy plans and functional assessments often fail to flow electronically between partners. These gaps produce systemic communication breakdowns that directly undermine care quality.
Missing or incomplete handoff data is a major risk to patient care. Without timely, structured transmission of medication changes, therapeutic progress, or social variables, post-acute specialists often start care treatments with insufficient context.
This can cause adverse drug events, inappropriate therapy intensity, or difficulties that could have been avoided, especially in rehab populations who are already medically complicated. Even when there is apparent integration of rehabilitation EHRs, anomalies in data mapping and a lack of common terms often lead doctors to go back to phone calls, faxes, or manual abstraction.
The situation gets worse because of operational inefficiencies. Sending referral packets late makes it harder to place patients, which keeps acute beds occupied longer than necessary and causes wasted bed days on both sides of the care continuum.
Case managers and intake coordinators spend a lot of time on manual data validation, which is a waste of resources that are already stretched thin. In markets with a lot of demand, delayed post-acute data exchange can mean lost revenue as referrals are diverted to more connected competitors.
Costs in the system have a ripple effect. Lack of robust post-acute care interoperability contributes to avoidable hospital readmissions, many tied to gaps in medication management or therapy coordination. Claims are denied because of missing paperwork and data that don’t match up between systems, which costs a lot of money to fix.
Staffing problems get worse: clinicians spend hours tracking information by hand that should happen automatically, which increases the risk of burnout and turnover. As payment models move toward value-based care, these hidden expenses will eat away at the profits of both acute and post-acute providers.
The business case for solving these gaps is clear, but achieving true rehabilitation EHR integration requires moving beyond basic document exchange to smart, structured, and bidirectional post-acute data exchange. The rehab sector has much to gain—and much to lose—depending on how quickly it addresses these persistent disconnects.
Smart, Dynamic Integrations Across Post-Acute Settings
For post-acute providers, the question of how to improve interoperability in healthcare centers on moving beyond simple data sharing to smart, dynamic integration—real-time, bidirectional interoperability that enables intelligent workflows across all care settings.
This requires moving beyond legacy HL7 v2 interfaces or static CCD document pushes to modern architectures based on FHIR APIs, event-driven messaging, and cloud-based data services.
Key Steps to Seamless Integrations Across Post-Acute Care
The first step to being able to share data in real time is to use FHIR-based RESTful APIs. These APIs let systems query and write structured clinical data (Observations, Medications, Care Plans) whenever they’re required to. More advanced models leverage FHIR Subscriptions, where systems automatically notify subscribed partners of data changes (for example, a medication change or new lab result).
For full clinical safety, this needs to be done along with transactional logging and identity resolution across disparate patient identifiers. This is a common challenge in post-acute networks operating across multiple EHRs.
It’s easy to see how managing bed availability and patient flow might work. Rehab intake teams have to manually follow the data provided by referring hospitals without a real-time connection. This often leads to missed referral windows or lost income.
Integrated systems can automate this process. For example, when the acute EHR updates the discharge-ready status, the post-acute availability and bed-matching logic can start dynamic referral workflows. This reduces delays, increases throughput, and decreases the number of wasted bed days.
Integrated surveillance tools are becoming more important for finding out about infection risk and preventing readmissions. These platforms need both streaming lab data (HL7 ORU^R01 messages or FHIR DiagnosticReport resources), combined with location and movement data.
Event-driven architectures let infection control dashboards send notifications as soon as relevant results are posted, which helps with early intervention. At the same time, sending therapy milestones, mobility scores, and socioeconomic factors back to primary care networks via FHIR Observation and Goal resources allows for coordinated prevention of readmission.
For advanced risk stratification and targeted resource deployment, modern implementations integrate real-time FHIR Bulk Data API (Flat FHIR) extracts into predictive analytics engines—often in a cloud-native data lake architecture (using platforms like AWS HealthLake or Azure Health Data Services).
This allows post-acute organizations to run machine learning models that continuously update patient risk scores, driving dynamic care plan adjustments and optimized resource allocation.
Achieving this level of integration requires not just technical capability but robust governance and data stewardship. Master patient index (MPI) reconciliation, data provenance tracking, and API security (OAuth 2.0, SMART on FHIR profiles) are critical to ensure that dynamic data flows remain accurate, secure, and auditable.
In short, rehabilitation EHR integration must evolve from static interfacing to true platform interoperability—modular, standards-driven, and architected for real-time, actionable intelligence.
Dive into the process of developing an AI-integrated FHIR data model designed to support cancer treatment.
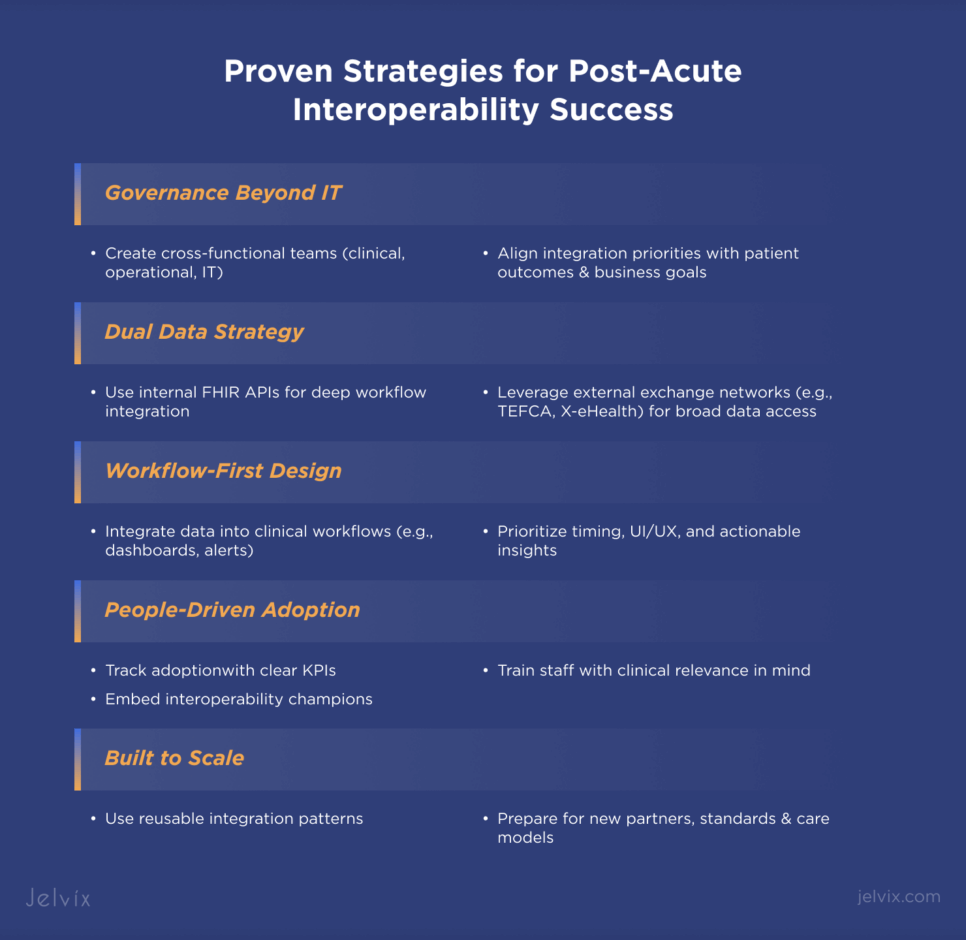
Proven Strategies for Post-Acute Interoperability Success
Post-acute interoperability that works is never just an IT initiative; it’s a change in the way the whole business works. Building interdisciplinary governance that connects clinical, operational, and technical leadership is one way to get started that has worked in the past.
A lot of the time, different IT teams are in charge of interoperability on their own. Cross-functional governance models, where therapy directors, infection control, intake coordinators, revenue cycle, and IT leaders all have a say in integration priorities, help high-performing rehab networks better align with both patient results and corporate goals.
Another thing that sets you apart is knowing how to use other exchange networks along with your own API development. Internal FHIR APIs make it possible to connect systems in a very detailed way. On the other hand, national or regional exchange frameworks like TEFCA in the U.S. or X-eHealth in Europe make it easy to get data from many different organizations.
Leading post-acute providers use two strategies: API-based rehabilitation EHR integration for deep operational workflows and external exchange participation for broad situational awareness.
Forward-thinking companies focus on integrating workflows, not merely moving data. Just moving data between systems isn’t enough; adoption will be slow if that data doesn’t show up at the correct time in the clinician’s workflow.
For instance, sending functional progress data to a care navigator dashboard or showing therapy adherence alerts in case management worklists gives you useful information that you can act on. These need careful UI/UX design and precise workflow mapping.
Lastly, training, managing change, and being able to grow are all important for long-term success. Even the best integrations won’t work if frontline staff don’t use them. Embedding interoperability champions in clinical teams, giving tailored training that links new workflows to clinical value, and monitoring acceptance with clear KPIs are all proven ways.
Scalability also requires architectural discipline, which means creating reusable integration patterns that can handle new referral partners, new data standards, and changing care models without having to recreate them all the time.
To sum up, getting real interoperability in post-acute care is as much about technology as it is about governance, user-centered design, and flexible workflows. Organizations that take this all-around strategy always do better than those that only care about following the rules.
Learn how we built a real-time risk assessment and Shadow AI control solution for rehabilitation center.
Generative AI in Post-Acute Care
Generative AI is likely to be a key part of the next generation of rehabilitation software. AI-driven technologies can simplify the time-consuming process of charting while improving clinical accuracy in post-acute settings, where diverse teams create a lot of narrative documentation like therapy notes, care plans, and patient progress reports.
Advanced rehabilitation technology uses AI for smart decision support in addition to documentation. For instance, AI models built into motion capture systems can look at the success of patients’ gait training and advise changes to their therapy plans in real time.
Generative models can develop individualized training situations for each patient in cognitive rehab. When integrated thoughtfully into clinical workflows, these capabilities shift rehab from static care plans to dynamic, data-driven interventions.
Ethical Considerations of Generative AI in Post-Acute Care
However, using generative AI in post-acute care brings up important ethical and operational considerations. Automated content needs to be able to be checked, be clinically correct, and follow the rules for regulatory documentation. Guardrails are necessary to keep people from relying too much on AI-generated text or unintentionally making bias worse.
Also, patient privacy measures must cover AI training data and outputs, especially in rehabilitation software that may deal with sensitive information like mental health or functional status.
To use AI effectively, you need to have strong change management. Clinicians need clear training on when and how to use AI outputs, and the EHR systems need to show AI-generated content clearly. Governance frameworks should define who is responsible for AI-enhanced documentation and decision support.
The goal is not to replace human clinical judgment but to make it better so that doctors can focus more on direct patient care while making sure that documentation is timely, accurate, and useful.
How Technology Partner Can Help Rehab Providers Close the Gap
Choosing that partner requires discernment. First, put vendors who have a proven track record in rehabilitation EHR integration and cross-continuum interoperability at the top of your list. This means they should have experience in more than just acute care or ambulatory settings.
The partner needs to know the many types of data, workflows, and rules that apply to rehab settings, as well as how to make sure that integrations support both clinical and operational goals.
Second, look at how the partner handles customization and configuration. Custom solutions that are too specific may work well in the short term, but they can become fragile and expensive to keep up. Look for modular platforms that let you customize them a lot by using open APIs, FHIR-native services, and reusable integration patterns. These platforms should also have as little custom code as possible, which can make it hard to change architectures.
Finally, look at how deep the support, maintenance, and long-term results are. Integration isn’t a one-time job; it needs continual governance, tracking of changes to standards, and optimization of performance. Leading partners offer more than just technical SLAs.
They also offer clinical adoption support, proactive monitoring, and strategic roadmapping. They are long-term partners who help rehab providers keep up with modifying interoperability standards, payer requirements, and service models.
In a post-acute ecosystem that is becoming more connected, the choice of healthcare tech partner will directly affect an organization’s capacity to compete, provide better patient care, and thrive under value-based care. Choosing the right partner is one of the most important strategic choices that rehab networks that are ready to lead will have to make.
Conclusion
Interoperability is no longer a choice in post-acute care; it is necessary for clinical excellence, operational efficiency, and financial stability. Rehab providers who remain locked in fragmented systems will struggle with higher readmissions, avoidable revenue leakage, and clinician burnout.
Investing in connected, dynamic interoperability will lead to improved results, such as easier transitions of care, more accurate therapy management, and happier patients.
To make this change happen, you need more than just technology. You need partners who are experienced with the challenges of integrating rehabilitation EHRs, can keep pace with evolving standards, and can provide solutions that are scalable and clinically aligned. Jelvix possesses that knowledge, which helps rehab providers bridge the interoperability gap and establish their networks for long-term success.
Get in touch with the specialists at Jelvix to find out how we can speed up your interoperability strategy and help you on your way to completely connected post-acute care.
FAQ
What are the risks of ignoring interoperability in rehab care?
Ignoring interoperability can cause care delays, more readmissions, fragmented patient experiences, billing mistakes, lost revenue opportunities, and non-compliance with evolving healthcare regulations.
How can custom interoperability solutions benefit rehab centers?
Custom solutions let rehab facilities make integrations that fit their specific workflows and patient demographics. This makes data more accurate, increases clinician productivity, and speeds up and makes care coordination more accurate compared to off-the-shelf systems.
Are there proven strategies to improve post-acute interoperability?
Yes. Some of the most important measures are to use standardized data formats like FHIR, take advantage of national health information exchanges, get everyone on the same page about governance, train personnel, and work with technology suppliers who know the ins and outs of post-acute care.
How can rehab centers measure the ROI of interoperability initiatives?
Value-based care initiatives can help you assess ROI by lowering the number of hospital readmissions, improving patient outcomes, making workflows more efficient, lowering administrative costs, and raising payment rates.
How do regulatory requirements affect interoperability efforts in rehab centers?
The 21st Century Cures Act and CMS regulations are examples of rules that call for better sharing of data and easier access to records for patients. To avoid penalties and fully participate in value-based reimbursement models, rehabilitation clinics must adhere to the rules.
Need high-quality professionals?
Fill the expertise gap in your software development and get full control over the process.