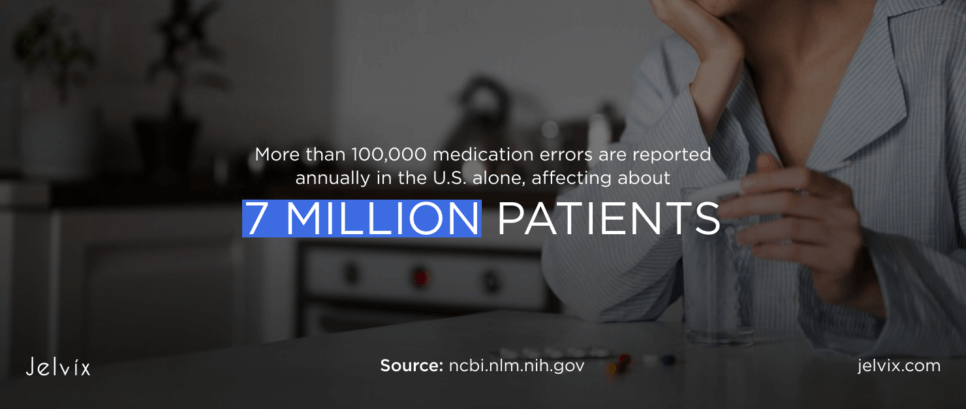
According to the FDA, more than 100,000 medication errors are reported annually in the U.S. alone, affecting about 7 million patients. These errors often happen due to differences between pharmacy and prescriber systems and result in wrong medication consumption potentially followed by patient injuries and deaths.
This became one of the major reasons to switch to e-prescription systems that accurately match patient info with prescribed medicine. Yet, standard e-prescription solutions usually offer a poor design that can result in incorrect patient and drug data, making the situation worse instead of improving it.
If you’re unsure whether you need to build a tailored e-prescribing app for your clinic, read this guide. You’ll find out key reasons and benefits of building electronic prescription software, factors that impact its cost, and proven steps to follow for a seamless development process.
What Is an E-Prescription App and How Does It Work?
An e-prescription app is a digital tool that makes it possible for doctors to write and send prescriptions electronically instead of writing them by hand. These apps make the prescribing process easier, as patients don’t need to visit a hospital to receive their prescriptions.
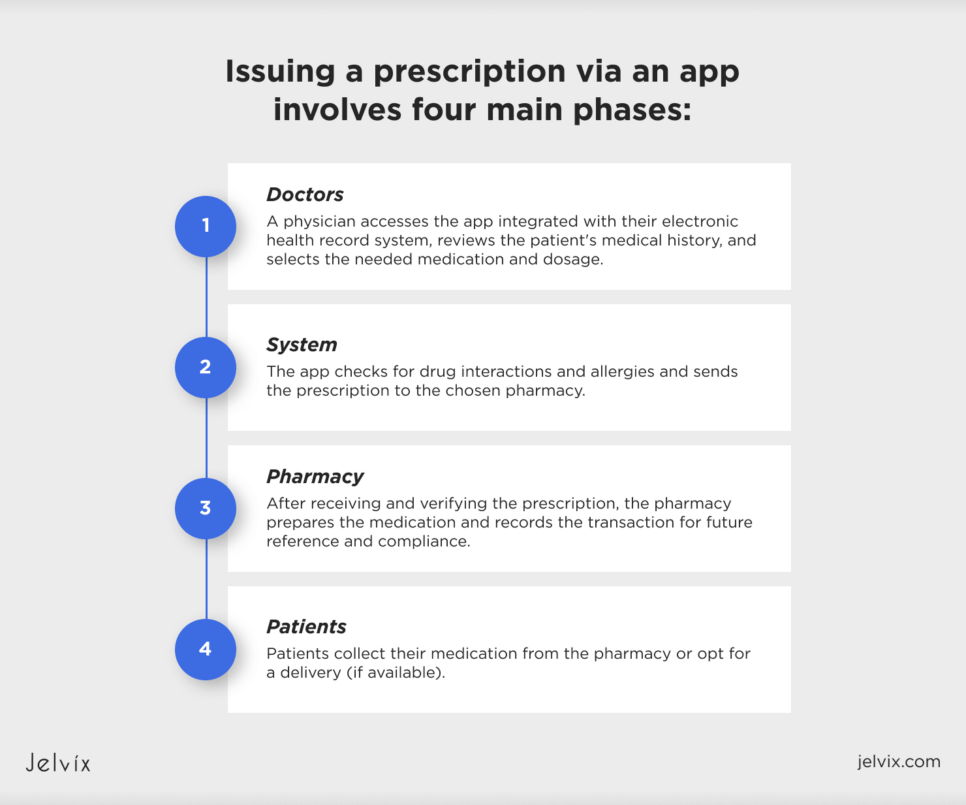
The process of issuing a prescription via an app can be divided into four main phases:
Doctors: a physician accesses the app integrated with their electronic health record system, reviews the patient’s medical history, and selects the needed medication and dosage;System: the app checks for drug interactions and allergies and sends the prescription to the chosen pharmacy;
Pharmacy: after receiving and verifying the prescription, the pharmacy prepares the medication and records the transaction for future reference and compliance;
Patients: a patient collects their medication from the pharmacy or opts for delivery (if available).
Both the clinic and the pharmacy have an electronic record of the issued prescription. They can access this record anytime and use it for refills, insurance claims, and audits.
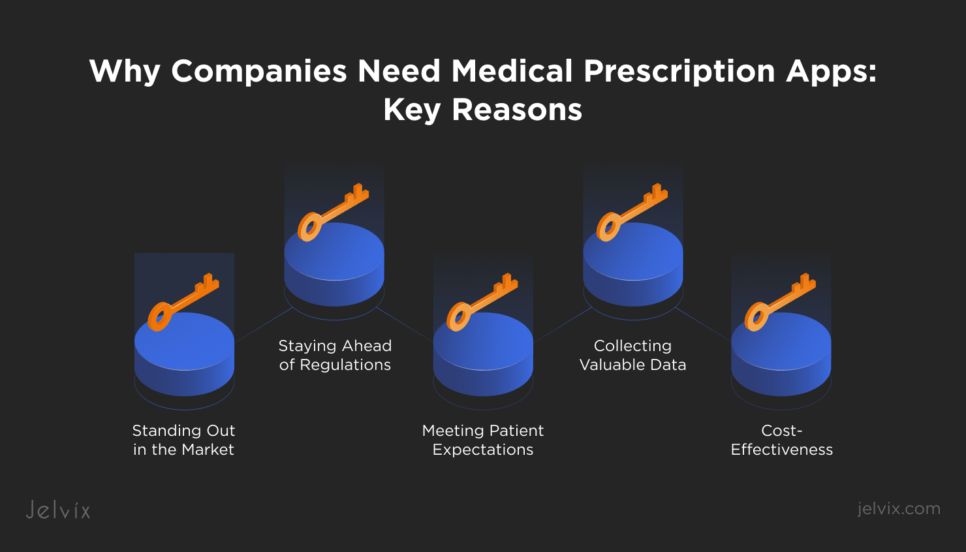
Why Companies Need Medical Prescription Apps: Key Reasons
Healthcare companies may want to integrate e-prescription apps into their settings for multiple reasons. These solutions can be truly beneficial, as they can make the prescription process faster and more accurate, save costs, and help ensure compliance with regulations.
Standing Out in the Market
Patients usually see companies that use prescription apps as user-centered and innovative businesses. This technology helps companies stand out, making medical services more attractive to patients who value convenience and modern care solutions.
Staying Ahead of Regulations
Healthcare regulations around patient data privacy are strict, and prescription apps help medical facilities stay compliant. These apps are designed to meet the latest standards to reduce the risk of costly fines because of compromising patient data.
Meeting Patient Expectations
Modern patients expect digital solutions that make their healthcare experiences smoother and less stressful. Prescription apps respond to these expectations by providing a simple way to manage prescriptions and enhance patient satisfaction.
Collecting Valuable Data
Similar to wearables and mHealth solutions, e-prescription apps gather data on how patients take their medications. Analyzing this data helps companies make informed decisions about patient care, improving and expanding their services.
Cost-Effectiveness
The WHO reports that the global annual cost of medication errors is about USD 42 billion. E-prescription apps can reduce the likelihood of these errors. What’s more, these apps decrease the administrative overhead associated with traditional prescription processes helping healthcare companies save on operational costs.
Discover the cost factors and considerations for healthcare app development. Explore insights and expert guidance on budgeting and planning for your healthcare app project.
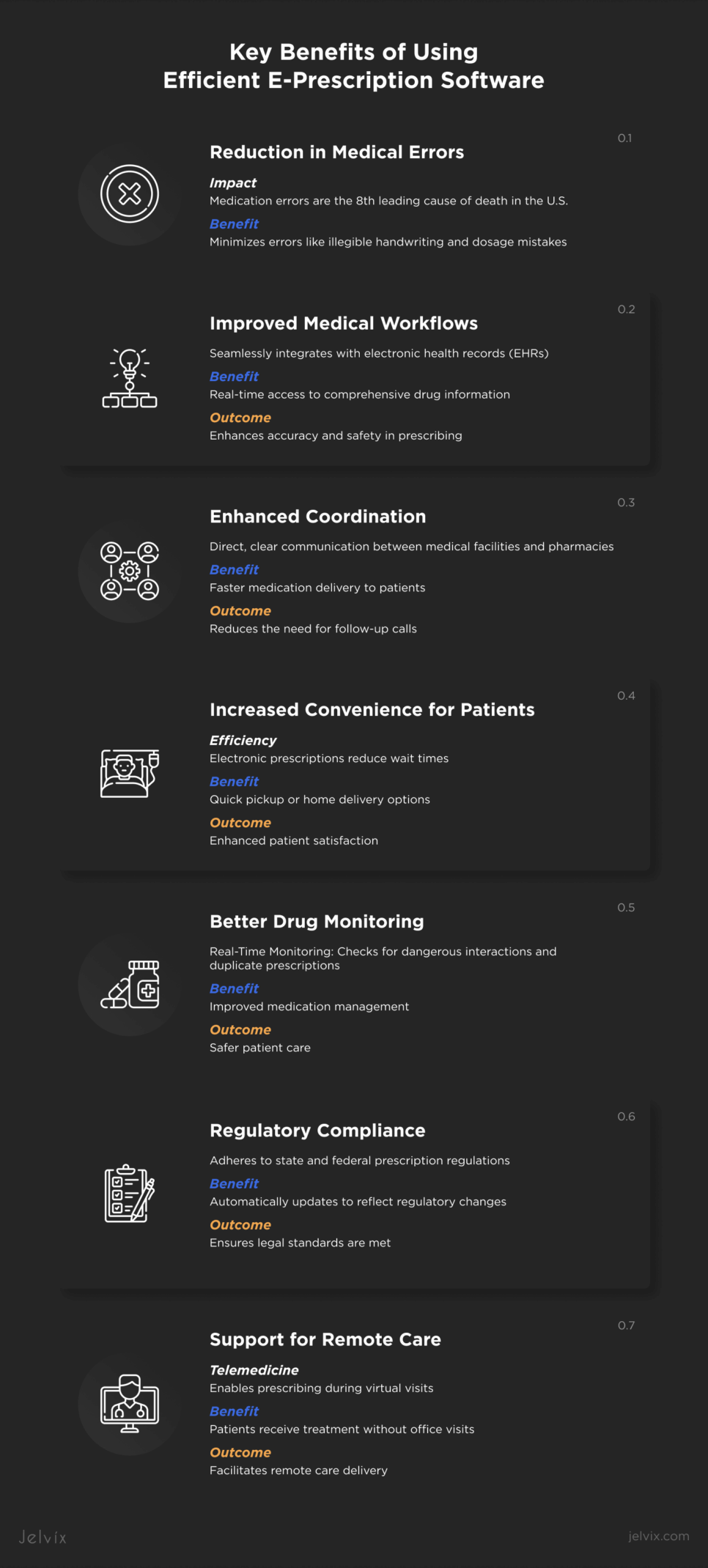
Key Benefits of Using Efficient E-Prescription Software
E-prescribing software provides a safer, faster, and more cost-effective way of managing prescriptions, significantly enhancing the quality of care delivery.
Reduction in Medical Errors
Medication errors are the 8th leading cause of death in the U.S. resulting in up to 98,000 people dying annually. E-prescribing apps can minimize the errors linked to traditional prescriptions, such as illegible handwriting or dosage mistakes by automatically checking prescriptions against patient allergies and drug interactions.
Improved Medical Workflows
E-prescribing software optimizes medical workflows by integrating with electronic health records. This technology ensures real-time access to comprehensive drug information, enhancing the accuracy and safety of the prescribing process.
Enhanced Coordination
An e-prescribing app enables direct and clear communication between medical facilities and pharmacies. This immediate data exchange helps ensure patients receive the correct medication quickly, reducing the need for follow-up calls.
Increased Convenience for Patients
With prescriptions sent electronically to pharmacies, patients no longer struggle with wait times. They can pick up their medications without delay, and even opt for home delivery options in some cases.
Better Drug Monitoring
E-prescription software improves how physicians monitor medications. It allows for real-time checking of prescriptions, which helps prevent issues like dangerous drug interactions and duplicate prescriptions.
Regulatory Compliance
E-prescription software helps healthcare companies comply with state and federal regulations regarding prescription drugs. These systems are updated to reflect changes in drug regulations, ensuring that all prescriptions meet current legal standards.
Support for Remote Care
E-prescribing is valuable for telemedicine as it supports remote care delivery. Doctors can prescribe medications during virtual visits, ensuring that patients receive the necessary treatment without the need to visit the doctor’s office.
Developing a Medical Prescription App: Cost Breakdown
Building an e-prescription app involves various costs that vary depending on the app’s complexity, tech features, and compliance requirements.
Software Development
The bulk of the costs usually come from software development, where they vary depending on developers’ location and expertise. The complexity of the app, such as API integration with existing systems, multiple platform support, or real-time data analytics, will significantly affect the total cost.
UX/UI Design
User interface (UI) and user experience (UX) design are critical for ensuring the app is user-friendly for both medical staff and patients. Professional design services can be costly, depending on the complexity and the designer’s expertise.
Compliance and Security
Complying with healthcare regulations, such as HIPAA in the U.S. and GDPR in the EU, is essential for e-prescription apps. Ensuring high levels of security and compliance can add significantly to development costs. This includes implementing secure communication channels, data encryption, and secure data storage solutions.
Testing and Quality Assurance
You’ll need to conduct thorough testing to ensure the app works correctly and securely, which involves both automated and manual testing phases. Costs vary depending on the scope of testing.
Project Management and Administration
Overseeing the development process involves project management, which can add about 10-15% to the overall project costs. This covers planning, coordinating with developers and designers, and ensuring the project meets its deadlines and budget.
Maintenance and Updates
After launching, the app will require regular updates and maintenance to add new features, fix bugs, and ensure it remains compatible with new versions of operating systems. This can cost anywhere from 10-20% of the initial development cost per year.
If you want to know the approximate cost of developing an e-prescription app and check out client reviews, visit our page on Clutch. However, if you need details on healthcare software development for your project, check out our guide on choosing a technical partner. Just fill out a contact form on our site, and download the guide to make sure you select a partner that can fulfill your development needs.
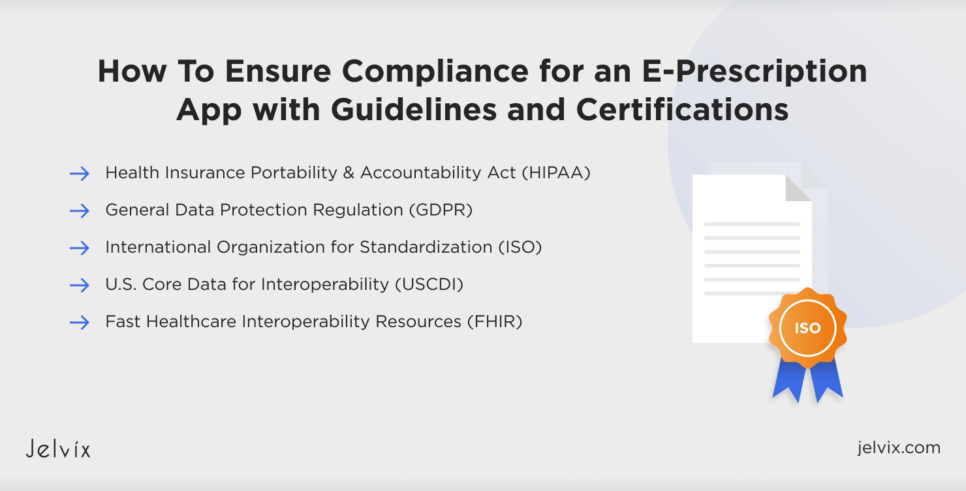
How To Ensure Compliance for an E-Prescription App with Guidelines and Certifications
Patient data is sensitive to leaks and vulnerable to security breaches. That’s why your medical software, including prescribing apps, must comply with key healthcare industry regulations.
Health Insurance Portability and Accountability Act
HIPAA is the U.S. federal law that requires protecting patient data through encryption, maintaining audit trails for monitoring and compliance checks, and conducting regular risk assessments.
General Data Protection Regulation
GDPR is the EU regulation that demands that apps get clear permission from users before using their data, use only the necessary data for their function, and quickly inform users if their data is compromised.
International Organization for Standardization
To prove the high level of security within your medical app, you need to obtain a certification like ISO 27001. Getting this certification involves documenting security procedures, training staff regularly, and having external experts check for the app’s security measures.
U.S. Core Data for Interoperability
The USDI standard focuses on making sure different healthcare systems can work together seamlessly. The app must be able to share data in a standardized way and be transparent about how information is used.
Fast Healthcare Interoperability Resources
FHIR involves using APIs that help different healthcare systems communicate efficiently and securely. The app needs to consistently check that these communications meet the latest health data standards.
Explore the significance of healthcare interoperability using FHIR standards. Learn how adopting FHIR enhances data exchange and integration across healthcare systems.
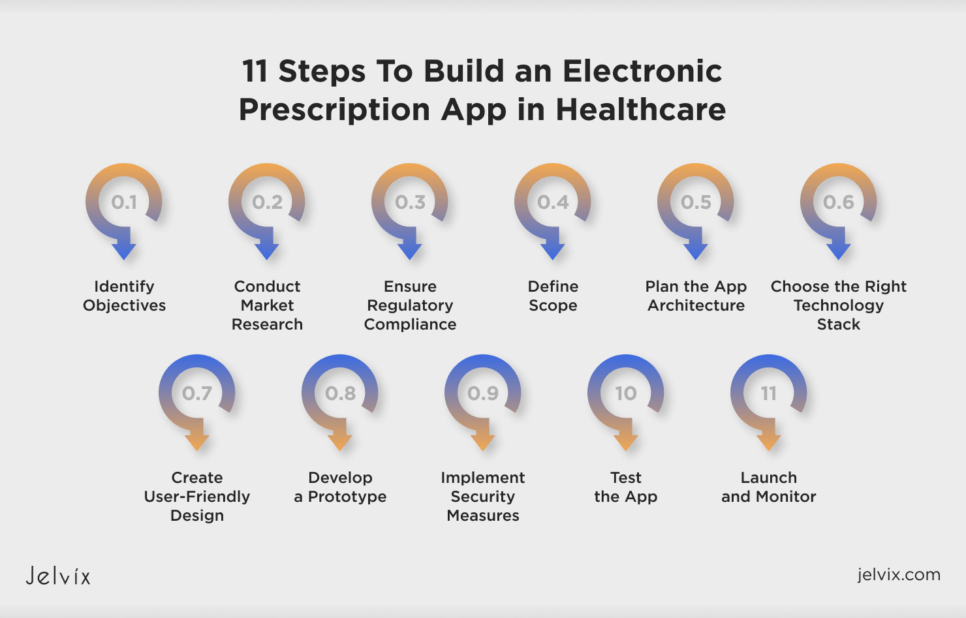
11 Steps To Build an Electronic Prescription App in Healthcare
Creating an e-prescription app requires careful planning to ensure it meets industry standards and provides a seamless experience for users. The Jelvix team recommends that you follow a step-by-step approach to ensure nothing is left out during the development process.
1. Identify Objectives
Start by defining what your app aims to achieve, the features it should include, and the problems it intends to solve. Consider the needs of all stakeholders, including healthcare pros, pharmacists, and patients.
2. Conduct Market Research
Research the market to understand the competition, potential challenges, and the latest trends in e-prescription technology. Evaluate the solutions your competitors have developed, find gaps in them, and use this info to make your app flawless.
3. Ensure Regulatory Compliance
Understand and incorporate all regulatory requirements, such as HIPAA and GDPR, to ensure the app complies with data protection and privacy laws. This also includes meeting the standards set by health authorities for electronic prescriptions.
4. Define Scope
Once you gather all the requirements, it’s time to define your project scope. This involves analyzing the collected information to outline what exactly needs to be developed. Establishing a well-defined scope will guide your development team, ensuring alignment with the initial objectives and compliance requirements.
5. Plan the App Architecture
Plan the app architecture considering scalability, security, and integration with existing healthcare systems. Ensure the architecture supports current needs and future expansions.
6. Choose the Right Technology Stack
Select the appropriate technology stack that aligns with your app’s requirements. This includes deciding on the development platforms, programming languages, databases, and cloud services.
7. Create User-Friendly Design
Focus on UI/UX design to ensure the app is intuitive and easy to use for everyone, from tech-savvy individuals to those less familiar with digital tools. Design with the Web Content Accessibility Guidelines in mind to make sure people with disabilities can also use your app.
8. Develop a Prototype
Create a prototype of your app to visualize the basic design and functionality. This early model helps stakeholders and potential users give feedback that can be used to refine the app before the full-scale development.
9. Implement Security Measures
Develop robust security protocols to protect sensitive medical information. This includes implementing strong encryption, secure data transmission, and safe storage practices.
10. Test the App
With the design and plan in place, start the development phase. Ensure thorough testing, including unit, integration, and user acceptance testing to identify and fix any issues before the public launch.
11. Launch and Monitor
After development and testing, launch your app on the chosen platforms. Continuously monitor its performance after launch and gather user feedback to make improvements. Regular updates are essential to add new features, address emerging issues, and adhere to new regulations.
Integrating E-prescription into Telemedicine Platforms: Useful Tips
The COVID-19 pandemic became the major factor for adopting telehealth and favoring remote care. Since patients can receive medical advice from the comfort of their homes, it is logical to integrate prescription capabilities into telehealth platforms for better convenience and accuracy.
Better Access to Medications
Integrating e-prescription software with a telehealth solution ensures patients have quicker and more convenient access to medications. After a virtual consultation, prescriptions can be immediately sent to a pharmacy near the patient, eliminating the need for physical visits to the doctor’s office just to pick up a prescription.
Quality Help
E-prescription systems integrated within telemedicine platforms enhance the quality of care by ensuring that prescriptions are accurate and based on up-to-date patient health records. Because the prescribing doctor has immediate access to the patient’s complete medical history during the telemedicine consultation, their decisions are better informed and likely to be more effective.
Scalability
The e-prescription integration can enhance the scalability of telemedicine services greatly. As telemedicine platforms grow to serve a larger number of patients, integrated e-prescription capabilities can easily expand to handle increased demand without the need for additional resources.
Building a Custom E-Prescribing Software vs. Integrating Ready-Made into Your EHR System
When you decide to implement e-prescription software into your medical settings, you’ll need to decide between developing custom software and integrating a ready-made solution into your EHR. Each option has advantages and drawbacks, and the choice should depend on your specific needs.
Developing a Custom E-Prescribing Software
Developing a custom app means creating an independent system for managing electronic prescriptions.
The main advantages of a custom software include:
- Customization: developing a custom system allows for tailor-made features that meet your specific workflows and requirements;
- Control: you have complete control over the development, updates, and security measures, which can make meeting specific regulatory compliance needs easier;
- Independence: a custom system does not depend on the limitations of existing EHR systems, providing you with the freedom to innovate and adapt to changes.
The most warning drawbacks of such solutions are:
- Higher costs: developing a custom system can be expensive due to the need for extensive resources in development, maintenance, and security;
- Integration issues: custom software may involve challenges integrating with other healthcare systems, which can lead to data silos and inefficiencies;
- Need for careful management: developing a custom app is a nuanced process full of technical and legal pitfalls. Without the proper management, it can become a headache rather than help you achieve business goals.
Integrating a Ready-Made E-Prescribing Solution into Your EHR
Integrating a ready-made e-prescribing solution into your existing EHR can optimize the implementation process and offer robust compatibility with established healthcare workflows.
Key advantages of such integration are:
- Speed of deployment: ready-made solutions can be deployed quickly compared to custom-developed software, allowing for rapid implementation and minimal disruptions;
- Cost-effectiveness: typically, integrating a ready-made solution is less costly than developing a custom system. This can be a more budget-friendly option, particularly for smaller healthcare facilities or those with limited resources;
- Proven reliability: since ready-made solutions were used and tested in various environments, they often come with a certain level of reliability and standardization.
The common drawbacks of integrating a ready-made solution include:
- Limited customization: one of the main limitations of ready-made solutions is that they may not perfectly fit your specific needs or workflow. The scope for customization is usually narrower than with a custom system;
- Dependency on a vendor: relying on a third-party solution can make you dependent on the vendor’s timelines for updates, improvements, and security patches. This can affect the agility of your medical organization;
- Compatibility issues: while these solutions are designed to integrate with various EHR systems, there are compatibility challenges that require additional configuration.
The choice between developing a custom e-prescribing software and integrating an existing one should consider your financial resources, technical capability and expertise, and long-term goals. Integrating a ready-made app can be a practical choice that balances cost, efficiency, and reliability, while a custom system might be better for specific functionalities.
How Jelvix Helps Develop Medical Prescription Software
Although e-prescription apps are relatively new on the mHealth market, their adoption will definitely increase. It means your app should be competitive and safe to win the market.
At Jelvix, we help healthcare entities build new medical solutions using innovative tech and our vast expertise in software development. Our strategy for developing and integrating medical apps into existing EHR/EMR systems centers around personalization, compliance, and better patient experience.
If you need assistance in creating a custom e-prescription app from scratch or integrating a ready-made solution into a telehealth platform or EHR system, contact us. Our experts will provide you with a consultation tailored to your company’s unique needs.
Seeking a skilled team of developers?
Elevate your development capacity with high-caliber expertise and resources.