In the dynamic landscape of healthcare, providers face a myriad of challenges in their pursuit of optimal EHR systems. From performance issues to the looming threat of data loss, seamless operations can feel like a distant dream. These challenges have led to a compelling call for change, with 59% of US physicians advocating for a complete EHR overhaul.
If you’re navigating the quest for the perfect EHR system and seeking insights into different options, read this article. The Jelvix team will delve into the best off-the-shelf solutions, discuss the benefits and drawbacks of developing custom EHRs, and address the challenges of both solutions.
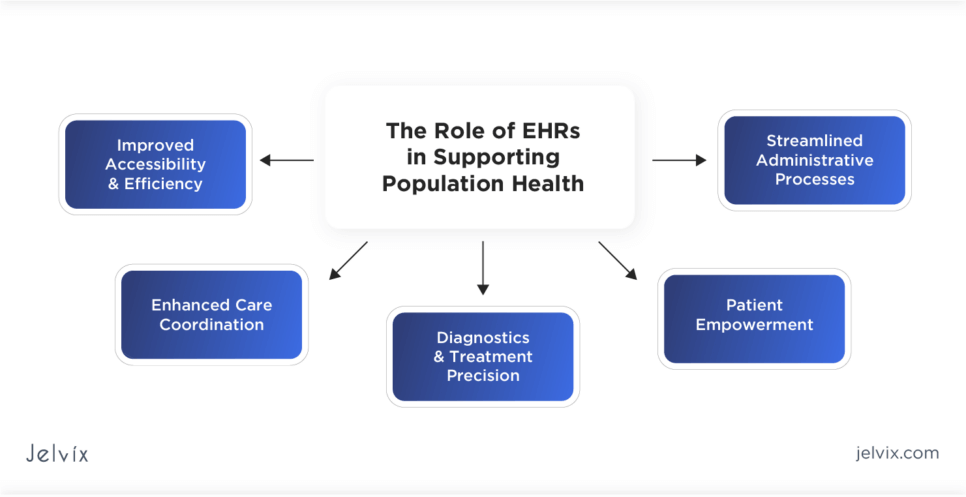
What Is the Role of EHRs in Supporting Population Health?
The implementation of EHRs has shown a transformative impact on healthcare delivery, revolutionizing how patient information is collected and managed. From optimizing daily operations to improving the quality of patient care, EHRs keep enhancing healthcare delivery in numerous ways.
Improved Accessibility and Efficiency
EHR systems grant instant access to comprehensive patient records, reducing delays in diagnosis and treatment. This accessibility enhances the efficiency of healthcare delivery, allowing physicians to make informed decisions swiftly.
Enhanced Care Coordination
Seamless sharing of patient data across departments fosters improved care coordination. Physicians, specialists, and support staff can collaborate effectively, leading to a holistic approach to patient care.
Diagnostics and Treatment Precision
EHR systems empower healthcare professionals with a wealth of patient data, allowing for more precise diagnostics and tailored treatment plans. This accuracy improves health outcomes and minimizes the risk of medical errors.
Patient Empowerment
EHR systems provide patients with secure access to their health records, fostering transparency and enabling them to actively engage in discussions about their care. Patients become active participants in their well-being.
Streamlined Administrative Processes
EHR systems streamline administrative tasks, reducing the burden of paperwork and manual record-keeping. This efficiency translates into focused attention on patient care, as doctors spend less time on administrative routines.
Electronic Health Records vs. Electronic Medical Records
EMRs and EHRs are both digital versions of patient health records, capturing and organizing medical information. Both systems aim to enhance healthcare efficiency, reduce errors, and improve patient care. They share common features like electronic documentation, storage of clinical data, and the potential to improve overall healthcare management.
Key Differences between EHR and EMR
Although there are numerous similarities between EMR and EHR, they differ in scope and functionality.
Electronic Health Records:
- Comprehensive: EHRs include a broader range of patient information, pulling data from various healthcare providers;
- Interoperability: they enable seamless information exchange among different healthcare systems, fostering collaboration;
- Patient-centric: they focus on the overall health of the patient, encompassing medical history, diagnoses, medications, treatment plans, and laboratory test results.
Electronic Medical Records:
- Clinic-centric: EMRs primarily focus on the patient’s medical history within a specific healthcare facility or clinic;
- Limited interoperability: they are designed for use within a single healthcare organization, making data exchange challenging across different systems;
- Clinical information: they mainly contain clinical data, including medical history, diagnoses, medications, and treatment plans specific to the facility using the system.
In essence, EHRs offer a more comprehensive and interoperable solution designed to facilitate information sharing across the broader healthcare landscape. EMRs are tailored to the needs of a specific healthcare organization, prioritizing clinical data management within the confines of that facility.
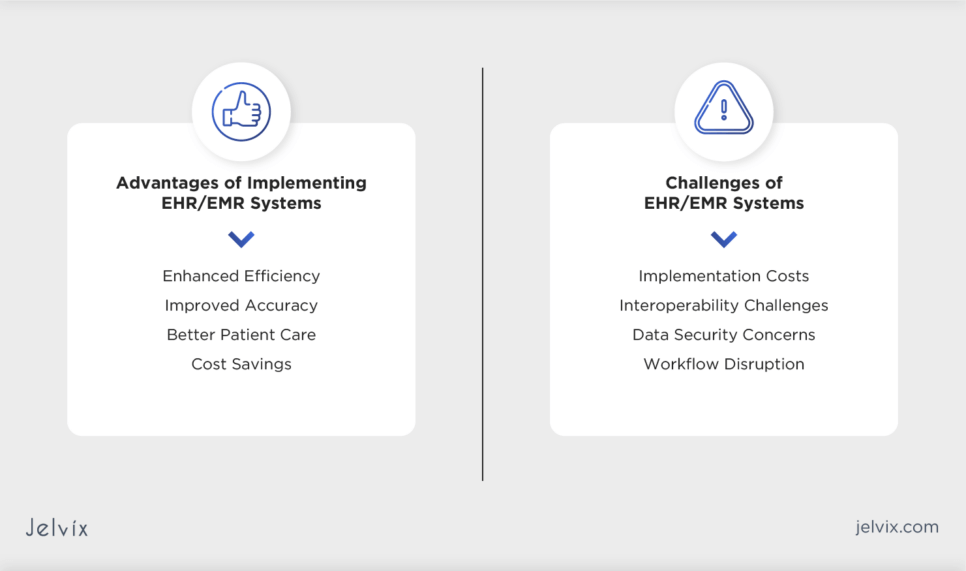
Advantages of Implementing EHR/EMR Systems
Embracing EHR/EMR systems indicates a new era in healthcare management as technologies mean numerous advantages.
Enhanced Efficiency
EHR/EMR systems are aimed at automating complex healthcare workflows. From appointment scheduling to prescription management, these digital solutions significantly reduce the administrative burden, allowing healthcare providers to focus more on patient care and less on paperwork.
Improved Accuracy
By minimizing the reliance on manual record-keeping, these systems mitigate the risk of errors associated with handwritten notes or misplaced documents. The result is a more precise and reliable repository of patient information, contributing to better-informed healthcare decisions.
Better Patient Care
EHR/EMR systems empower healthcare professionals to instantly access a patient’s complete medical history and diagnostic results. This seamless data accessibility fosters informed decision-making, enabling personalized and timely care tailored to individual patient needs.
Cost Savings
The transition to digital records streamlines resource allocation, reduces the need for physical storage space, and minimizes errors that could lead to costly consequences. Over time, these efficiencies contribute to a more cost-effective and sustainable healthcare ecosystem.
Challenges of EHR/EMR Systems
While the benefits of EHR/EMR adoption are substantial, the journey still has its challenges.
Implementation Costs
EHR/EMR adoption involves substantial initial expenses. Beyond the cost of the technology itself, significant investments are required for the setup, implementation, and training of staff. To prevent extra spending, focus on essential functionalities during the initial implementation, deferring non-critical features to later stages.
Interoperability Challenges
Ensuring seamless compatibility and interoperability between EHR/EMR systems and existing healthcare infrastructures is a complex challenge. Variations in data formats and standards across providers can lead to integration complexities. Collaborate closely with EHR/EMR vendors to align systems with existing infrastructure to address interoperability issues effectively.
Data Security Concerns
EHR/EMR systems store sensitive health information, making them lucrative targets for cyber threats. Maintaining robust cybersecurity measures and ensuring compliance with privacy regulations, such as HIPAA, are ongoing challenges. Consider employing encryption, access controls, and regular security audits to fortify the EHR/EMR systems against potential cyber threats.
Workflow Disruption
The introduction of EHR/EMR systems often brings about a period of adjustment for healthcare professionals and staff. Established workflows may undergo disruptions, leading to short-term productivity challenges. Adequate training, change management strategies, and phased implementations are crucial to mitigating these disruptions and ensuring a smoother transition to the new digital workflows.
Customization Limitations of EHR/EMR Systems
As you probably know from EHR/EMR software reviews, these systems offer extensive customization options, allowing healthcare providers to tailor the software to their specific needs. However, certain limitations may prevent them from smooth performance:
- Fundamental system architecture: сore elements of the system architecture, such as the underlying database structure or fundamental functionalities, may be challenging to customize extensively without compromising system integrity
- Vendor restrictions: some EHR/EMR systems may have limitations imposed by the software vendor, restricting certain deep-level customizations to maintain system stability and supportability;
- Regulatory constraints: compliance with healthcare regulations, such as HIPAA, may limit customization options in areas that could compromise patient privacy or data security;
- Interoperability standards: customization that differs significantly from interoperability standards may hinder seamless data exchange with other healthcare systems and providers.
To navigate customization limitations in EHR/EMR systems, healthcare providers should engage in thorough pre-implementation assessments. Collaborating closely with vendors, understanding regulatory nuances, and aligning customization needs with interoperability standards will help strike a balance between tailoring the system and maintaining regulatory compliance, stability, and effective data exchange.
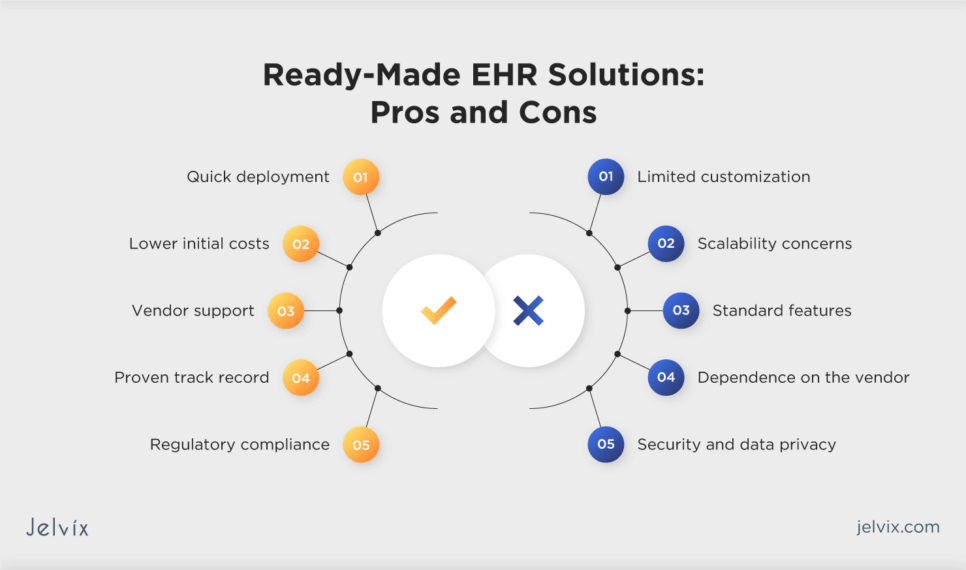
Ready-Made EHR Solutions: the Convenience Factor
Navigating the complex landscape of healthcare technology often involves critical decisions about the type of EHR solution to adopt. The convenience of ready-made EHR solutions comes with its own set of advantages and drawbacks. Understanding both is crucial for making informed decisions in adopting off-the-shelf EHR solutions.
Off-the-Shelf Software Advantages
Ready-made EHR solutions present a compelling option, offering convenience, quick deployment, and vendor support.
- Quick deployment: ready-made solutions allow for swift deployment, reducing the time needed for implementation;
- Cost-effectiveness: off-the-shelf solutions often come with lower initial costs compared to custom development, making them budget-friendly;
- Vendor support: vendors provide ongoing support, updates, and maintenance, soothing the burden on healthcare organizations;
- Proven track record: established off-the-shelf solutions typically have a track record of successful implementations across various healthcare settings;
- Regulatory compliance: reputable vendors ensure that their off-the-shelf solutions adhere to industry regulations, minimizing compliance concerns for healthcare organizations.
Ready-Made EHR Drawbacks
Limited customization, potential scalability issues, and dependence on vendor roadmaps are considerations that healthcare providers must weigh against the immediate benefits.
- Limited customization: off-the-shelf solutions may lack the flexibility required to adapt to unique workflows and processes in specific healthcare settings;
- Scalability concerns: healthcare organizations with significant growth may find these solutions less scalable, potentially leading to limitations as operations expand;
- Standard features: some included features may not be relevant to all users, leading to unnecessary complexity for certain healthcare practices;
- Dependence on the vendor: organizations must rely on the vendor’s development roadmap, limiting their ability to influence the introduction of new features or functionalities;
- Security and data privacy: while vendors prioritize security, healthcare organizations may have less control over the implementation of specific security measures, potentially raising concerns about data protection.
10 Steps to Choose the Right EHR/EMR Solution
Choosing the right EHR/EMR solution is a complex process crucial for effective healthcare management. The Jelvix team created this brief step-by-step guide to assist you in choosing the most suitable EHR/EMR solution.
Step 1. Needs Assessment
Dive deep into your organization’s specific requirements. Understand not only current workflows but also potential future needs. Prioritize functionalities crucial for delivering optimal patient care.
Step 2. Feature Analysis
Assess electronic health records features offered by vendors, ensuring they align with your healthcare organization’s unique needs and workflows.
Step 3. Regulatory Compliance Review
Ensure potential EHR/EMR solutions comply with healthcare regulations like HIPAA. This includes not only basic compliance but also considerations for future regulatory changes.
Step 4. Vendor Reputation
Research and evaluate the reputation of EHR/EMR vendors. Consider user reviews, testimonials, and the vendor’s track record in the healthcare industry.
Step 5. Data Security
Implement robust security protocols, including encryption and access controls, to protect sensitive patient information. Choose solutions that prioritize data security and maintain compliance with healthcare regulations.
Step 6. Interoperability Standards
Confirm that the chosen solution adheres to interoperability standards, enabling seamless data exchange with other healthcare systems and providers.
Step 7. Scalability
Evaluate the scalability of a healthcare solution to accommodate the growth of your healthcare practice and evolving data storage needs.
Step 8. Usability and Training
Prioritize user-friendly interfaces and assess the training and support provided by the vendor to ensure efficient adoption by healthcare staff.
Step 9. Cost Analysis
Conduct a thorough cost analysis, considering both initial implementation costs and ongoing expenses, to ensure the chosen solution aligns with your budget.
Step 10. Pilot Implementation
Consider a pilot implementation or trial period to assess the practical usability and effectiveness of the EHR/EMR solution within your healthcare setting.
Learn how to successfully implement EHR systems to improve patient care, optimize workflows, and meet compliance standards.
EHR/EMR Software Reviews: Top 5 Solutions for Healthcare
There are numerous ready-to-work EHR solutions on the market, each having standout features that make these platforms the top choices for healthcare providers. From robust customization options to seamless integrations, this Top 5 Guide highlights key functionalities that define the best EHR/EMR software.
1. Epic Systems Corporation
Epic offers a comprehensive EHR system with modules for various healthcare functions, including clinical documentation, order entry, and revenue cycle management. Its interoperability capabilities enable seamless data exchange between different healthcare entities. Epic is widely used in large healthcare systems and academic medical centers.
2. Cerner Corporation
Cerner provides an extensive suite of solutions, from EHR and population health management to data analytics. Known for its interoperability initiatives, Cerner facilitates the exchange of health information across disparate systems. It is often chosen by healthcare organizations looking for advanced clinical functionalities and robust analytics.
3. Athenahealth
Athenahealth offers a cloud-based EHR platform coupled with medical billing and practice management solutions. It is recognized for its user-friendly interfaces and streamlined workflows. Athenahealth caters to practices of various sizes and specialties, focusing on enhancing operational efficiency and revenue cycle management.
4. Allscripts Healthcare Solutions
Allscripts provides EHR, practice management, and revenue cycle management solutions. Its EHR system is customizable to meet the unique needs of different healthcare settings. Allscripts is known for offering flexible solutions that cater to both ambulatory and acute care settings.
5. NextGen Healthcare
NextGen Healthcare offers an EHR platform integrated with patient engagement tools and population health management features. It is recognized for its adaptability to diverse healthcare practices, allowing customization to suit specific workflows. NextGen Healthcare focuses on improving patient outcomes through enhanced care coordination and data-driven insights.
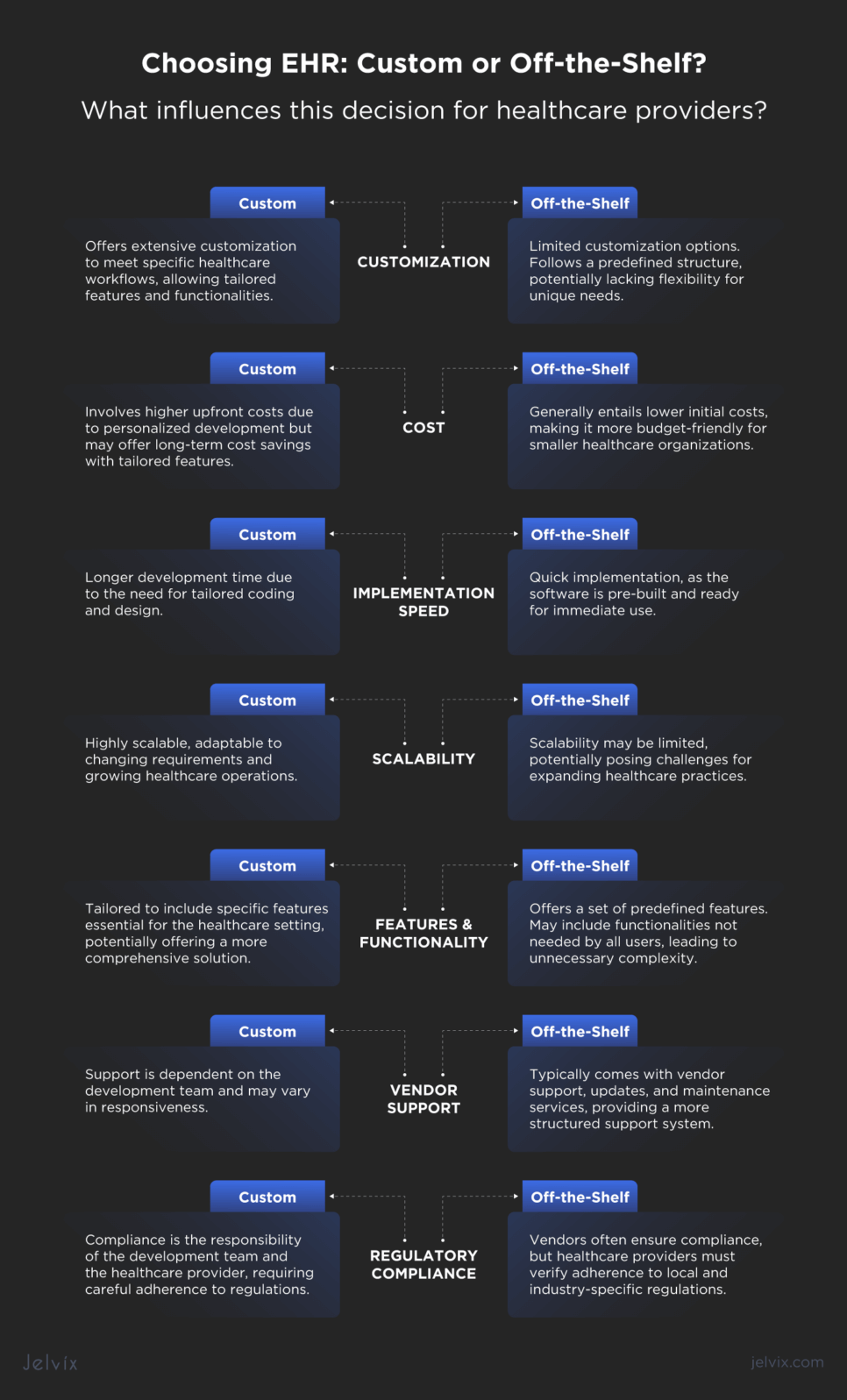
Custom Medical Software vs. Off-the-Shelf Product Solutions
When it comes to adopting EHR solutions, healthcare providers encounter the choice between custom software and ready-made solutions. The decision hinges on key factors, such as company-specific needs, budget constraints, and flexibility.
Customization
Custom: Offers extensive customization to meet specific healthcare workflows, allowing for tailored features and functionalities.
Off-the-Shelf: Limited customization options. Follows a predefined structure, potentially lacking flexibility for unique needs.
Cost
Custom: Involves higher upfront costs due to personalized development, but may offer long-term cost savings with tailored features.
Off-the-Shelf: Generally entails lower initial costs, making it more budget-friendly for smaller healthcare organizations.
Implementation Speed
Custom: Longer development time due to the need for tailored coding and design.
Off-the-Shelf: Quick implementation, as the software is pre-built and ready for immediate use.
Scalability
Custom: Highly scalable, adaptable to changing requirements and growing healthcare operations.
Off-the-Shelf: Scalability may be limited, potentially posing challenges for expanding healthcare practices.
Features and Functionality
Custom: Tailored to include specific features essential for the healthcare setting, potentially offering a more comprehensive solution.
Off-the-Shelf: Offers a set of predefined features. May include functionalities not needed by all users, leading to unnecessary complexity.
Vendor Support
Custom: Support is dependent on the development team and may vary in responsiveness.
Off-the-Shelf: Typically comes with vendor support, updates, and maintenance services, providing a more structured support system.
Regulatory Compliance
Custom: Compliance is the responsibility of the development team and the healthcare provider, requiring careful adherence to regulations.
Off-the-Shelf: Vendors often ensure compliance, but healthcare providers must verify adherence to local and industry-specific regulations.
When to Consider Custom EHR Development
Developing a custom EHR solution is a serious decision that will impact the whole healthcare organization’s performance. Healthcare providers need to evaluate all benefits and drawbacks, and also keep in mind key reasons for custom software development:
- Unique workflow requirements: a healthcare organization has distinctive workflows that demand tailored solutions for seamless integration and optimized operations;
- Specific features: off-the-shelf products lack essential features crucial for your healthcare processes, requiring a custom solution catering to your specific requirements;
- Scalability demands: you anticipate significant growth, and your healthcare systems need to scale dynamically to accommodate expanding operations efficiently;
- Integration complexity: the integration of healthcare systems with existing infrastructure, third-party applications, or specialized devices demands a customized approach for seamless connectivity.
- Regulatory compliance specifics: healthcare operations necessitate adherence to specific regulatory standards, and a custom solution ensures precise compliance tailored to your organization’s requirements;
- Enhanced data security: healthcare organization handles sensitive patient data, and a custom solution allows for robust security measures tailored to your unique data protection needs;
- Long-term cost efficiency: while the initial investment may be higher, a custom solution offers long-term cost efficiency by eliminating expenses associated with unnecessary features and providing scalability without hefty licensing fees.
In case you decide to develop a custom Electronic Health Record solution, consider what end users think, too. A study by Stanford Medicine revealed that physicians in the US advocate for four main improvements in their existing systems:
- Improving user interface design for streamlined workflows;
- Delegating EHR data entry to support staff;
- Implementing voice recording to act as a real-time scribe during patient visits;
- Creating an AI assistant to support physicians in delivering personalized and efficient patient care.
Make sure to share these insights with your tech partner and discuss the possibilities of their implementation into your custom EHR system.
See how Jelvix developed a cutting-edge EHR system to streamline patient care, improve data management, and enhance healthcare efficiency.
Custom EHR Software Costs Overview
According to EHR/EMR research by HealthIT, the expenses associated with acquiring and implementing an EHR fall within the range of $15,000 to $70,000 per provider. The cost variation is influenced by the choice between on-site EHR and web-based EHR deployment.
Web-based deployment, commonly referred to as Software as a Service, usually entails providers paying a fixed monthly subscription fee. On the other hand, on-site deployment requires providers to cover ongoing expenses related to the support and management of on-site data servers.
5 Key Factors that Influence the Cost of Custom EHR Development
The cost of custom EHR development is impacted by numerous factors that healthcare providers should not ignore. Understanding how each factor influences the price may enable informed decision-making and effective budget planning throughout the development lifecycle.
Technology Stack
The selection of technologies, frameworks, and tools affects both development efficiency and licensing fees. Opting for cutting-edge or specialized technologies may increase costs due to higher licensing fees and potentially longer development timelines.
Development
The complexity of coding determines the functionality of the custom EHR. More complex features and functionalities increase development time and, consequently, costs.
Testing and Quality Assurance
Rigorous testing is a crucial step to ensure the reliability and security of the EHR. The more comprehensive the testing process, including usability, security, and integration testing, the higher the associated costs.
Integration with Existing Systems
Compatibility with diverse existing systems requires additional development efforts. The need for adaptability and interoperability increases complexity and development time, contributing to higher costs.
Ongoing Maintenance and Compliance
Continuous maintenance and compliance efforts are essential for the EHR’s longevity and adherence to industry regulations. Regular updates, security patches, and ongoing compliance measures contribute to recurring costs post-development.
How to Choose the Right Healthcare Software Development Company
Choosing the right healthcare tech partner involves evaluating their expertise, understanding of healthcare regulations, and track record in delivering secure, scalable solutions.
At Jelvix, we highly value both healthcare providers’ requirements and the needs of EHR end-users. That is why over 50 companies entrusted their healthcare projects to us. We developed a telehealth solution for a US-based clinic that reduced daily administrative tasks by 25%. With our innovation, the clinic achieved a 30% decrease in unnecessary patient visits, capturing data from their medical wearable devices.
We are dedicated to enhancing healthcare access and outcomes through technology and are ready to assist you in achieving your business goals. Get in touch with our managers for a detailed consultation. They are always happy to help.
Need a tailored EHR cost estimation?
Whether you are building a new EHR from scratch or upgrading an old solution, Jelvix’s healthcare IT consultants and EHR developers are here to help you create a winning feature set.