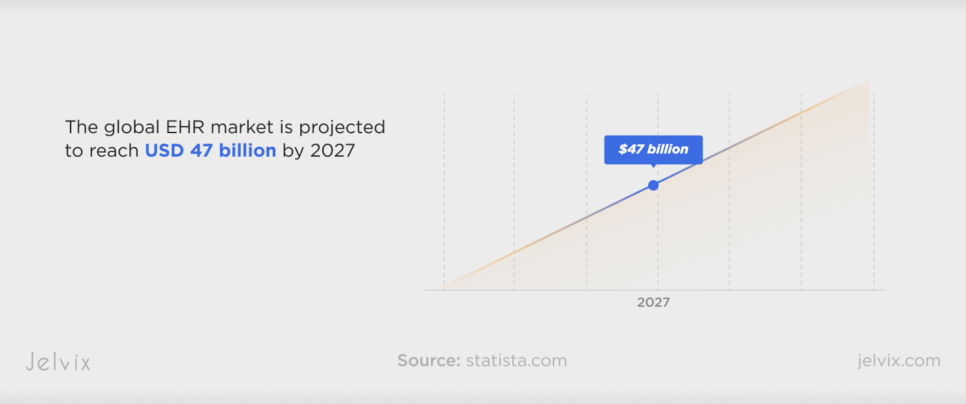
Nowadays, it’s almost impossible to find a clinic or a hospital system that doesn’t use digital tools like EHRs. By 2027, the global EHR market is expected to hit USD 47 billion, with Cerner, Epic, and Meditech remaining the industry-leading vendors. But despite the fact that they offer a vast range of features and strong support to medical facilities, integrating such complex systems can be challenging and costly.
At Jelvix, we couldn’t ignore such a worrying problem. We conducted a series of surveys to understand key preferences and issues in integrating EHRs into set workflows and collaborated with experts in the field to present recommendations for successful integration.
In this article, you’ll find out how to choose the best EHR system for your clinic and reduce the implementation costs at the same time. You’ll also discover key EHR implementation steps to keep up with set timelines and budget constraints.
This giude represents a collaborative effort by the Jelvix team, led by our CEO, Head of Project Management, and other professionals with deep expertise in healthcare software development. The research was further enriched by Dr. Aditi U. Joshi, a physician and telehealth expert with over 10 years of experience.
As the founder of Nagamed Consulting and co-author of Telehealth Success, Dr. Joshi contributed valuable insights in telemedicine and digital healthcare. Together, through comprehensive research and industry expertise, we’ve distilled actionable, forward-thinking strategies for successful EHR integration.
Epic and Cerner EHR Systems: a Short Overview
Epic EHR is one of the leading solutions for healthcare organizations. It serves about 285 million patients worldwide, storing their data within a cloud-based environment. Large-scale medical facilities tend to choose Epic because of its comprehensive and integrated approach to healthcare data management. Larger clinics often have a complex infrastructure, and Epic helps manage it with its advanced integration and scalability capabilities.
Cerner EHR is mostly popular among mid-sized healthcare businesses. It’s more intuitive and flexible, offering advanced and customizable documentation tools to record and retrieve patient info. Cerner provides strong analytics tools to help gain insights from clinical and operational data and is less expensive than Epic, making it a good choice for smaller clinics.
Understanding the Epic USCDI API: Why It Matters
The USCDI API is a standardized programming interface developed by Epic. Its main goal is to ease medical data exchange. It supports key interoperability standards, allowing clinics to access and manage patient data safely.
Another advantage of Epic USCDI API is its ability to comply with federal regulations. For instance, the 21st Century Cures Act makes the use of standardized APIs obligatory, and EPIC’s API already adheres to this demand.
The benefits of using Epic USCDI API also spread to the financial aspects of medical tech. Since standardized data sharing minimizes the need for complex and costly interfaces between different systems, clinics can allocate resources more effectively and save costs as a result.
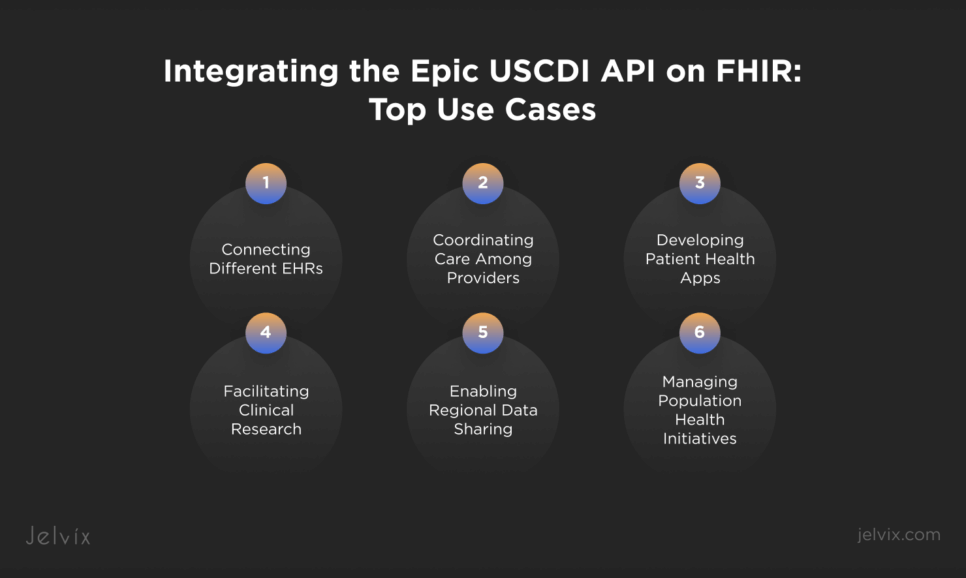
Integrating the Epic USCDI API on FHIR: Top Use Cases
APIs allow disparate systems to communicate with each other, letting all medical teams be on the same page. Epic USCDI API on FHIR goes even further, allowing any clinic that uses Epic EHR to connect any app or platform that supports FHIR.
Connecting Different EHRs
Hospitals often use various EHRs which leads to data silos and slowers down treatment processes. Epic’s FHIR API resolves this problem by offering physicians seamless and safe access to patient information, such as treatment history, medications, and allergies, whenever they need it.
Coordinating Care Among Providers
Thanks to Epic USCDI API on FHIR, different medical teams can exchange patient data in real time. It means that all doctors have up-to-date and correct data that helps them make informed treatment decisions. This integration supports collaborative care, reduces the risk of medical errors, and improves patient safety.
Developing Patient Health Apps
About 63% of adult patients in the U.S. seek access to their health data through mobile apps. Epic’s API allows developers to create and integrate patient-centered apps that provide secure access to health records, lab results, and medication lists.
Facilitating Clinical Research
Epic USCDI API on FHIR also aids researchers, providing them with access to comprehensive patient data for conducting studies and trials. As a result, research teams can aggregate patient data from various sources, ensuring its consistency and quality.
Enabling Regional Data Sharing
Electronic health information exchange aids the sharing of health data across different medical entities within a region. By integrating the Epic USCDI API on FHIR, HIEs can ensure that shared data is standardized and interoperable.
Managing Population Health Initiatives
Population health management focuses on improving health outcomes for specific groups of people. The Epic USCDI API on FHIR supports the aggregation and analysis of health data, allowing clinics to identify trends, manage chronic diseases, and implement targeted interventions for better community health outcomes.
Discover expert tips and key steps to streamline EHR implementation, improve workflows, and enhance patient care.
Cerner vs Epic vs Other EHR: What To Choose for Your Clinic
Choosing the right EHR system depends on the specific needs and size of your facility. You need to evaluate your clinic’s requirements, budget, and long-term goals to make the best choice.
According to a survey conducted by the Jelvix team, the majority of medical businesses prefer Epic over other EHRs. Its comprehensive and integrated data management features make it a perfect choice for enterprises that require extensive customization.
Cerner is known for its innovative technology solutions that help improve workflows and patient care. It best suits providers who need advanced data analytics, clinical documentation tools, and revenue cycle management features.
If your clinic isn’t that big, consider choosing less extensive solutions. EHRs like Meditech offer reliable and cost-effective tools for small to medium-sized healthcare businesses. They usually focus on providing essential features without the complexity of larger systems.
Sometimes, clinics can face a situation when none of the ready-made EHRs meet their needs. In this case, they can opt for developing a custom system. If you need help in creating a tailored solution for your hospital, feel free to request a consultation from the Jelvix team. Our experts will guide you through the healthcare software development process and help integrate your custom EHR without disrupting your clinical workflows.
Dr. Joshi Quote:
“What advice would you give to clinics and healthcare systems just starting to integrate digital technologies? What are the key steps they need to take for successful adoption?”
This is a big question, but I will take learning from design thinking. Understand that your user is both the patient and the clinician. Research the community you serve and the workforce that is going to deliver care. From there, find out the greatest needs. Once you know that, creating a program has the same steps as any other project.
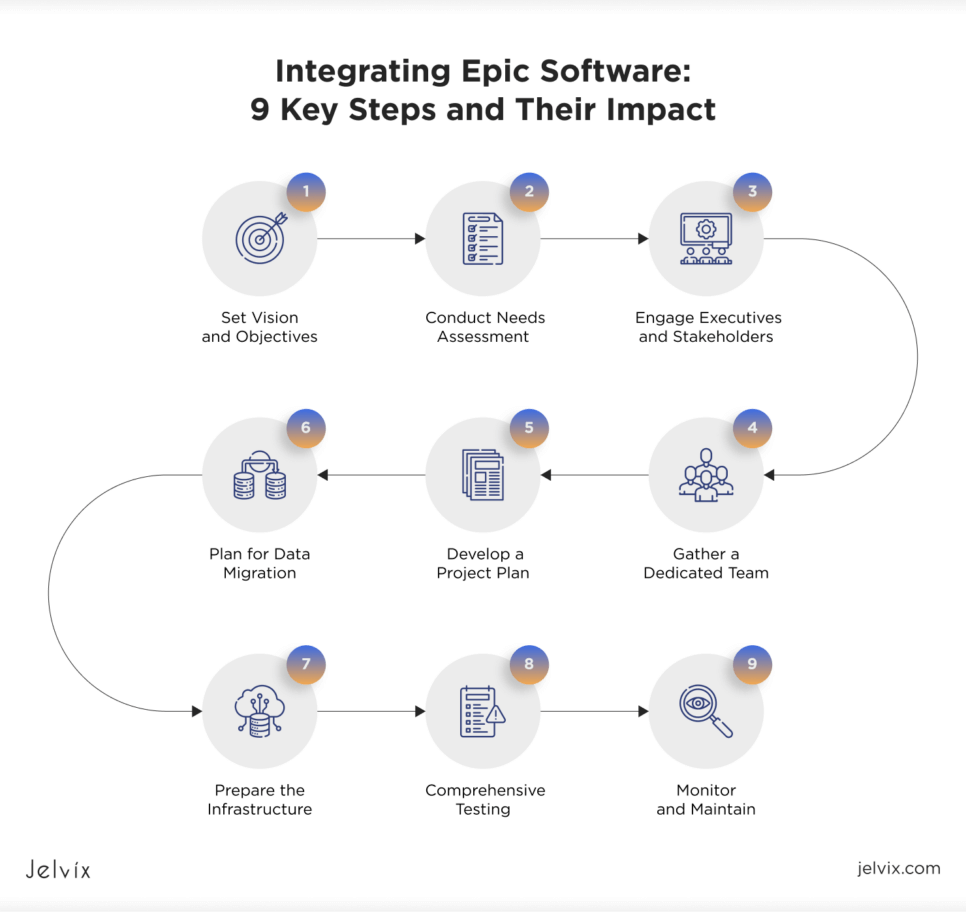
Integrating Epic Software: 9 Key Steps and Their Impact
Implementing a ready-made EHR like Epic requires careful planning and preparation. The Jelvix team recommends that you follow a gradual approach and consider the influence of each step on the whole integration process.
1. Set Vision and Objectives
Identify what your clinic or hospital system aims to achieve with EHR integration. This can be improved patient care, smoother workflows, or enhanced data analytics. A clear vision and well-defined objectives provide direction for the entire project.
2. Conduct Needs Assessment
Perform a detailed assessment of your current systems, workflows, and processes. Identify gaps and areas for improvement that the Epic EHR system can address. Such an assessment provides a clear understanding of what functionalities and features are required from the new system.
3. Engage Executives and Stakeholders
Gain the support of executive leaders and engage key stakeholders, including physicians, nurses, administrative staff, and IT personnel. Executive sponsorship ensures that the project has the necessary resources, budget, and authority to proceed. Stakeholder buy-in is critical for overcoming resistance to change and ensuring that all departments are on board with the new system.
4. Gather a Dedicated Team
Form a project team from various departments, including clinical, administrative, and IT staff. Assign clear roles and responsibilities to enhance accountability and ensure that tasks are completed efficiently. If a Clinical Informatics team is available, make use of their expertise early on.
5. Develop a Project Plan
Create a comprehensive project plan that outlines timelines, milestones, resource allocation, and risk management strategies. This plan serves as a basis for the whole implementation process helping track progress, manage resources, and ensure that the project stays on schedule.
6. Plan for Data Migration
Develop a data migration strategy to transfer patient records and other essential data from existing systems to the new EHR system. Validate and clean the data to ensure accuracy. A well-prepared data migration reduces the risk of data loss, errors, and inconsistencies.
7. Prepare the Infrastructure
Assess and upgrade your IT infrastructure to ensure it can support the new EHR system. This may involve enhancing network capabilities, upgrading hardware, and ensuring robust cybersecurity measures. A well-prepared infrastructure makes the operation of Epic EHR smoother.
8. Comprehensive Testing
Conduct testing of the integration to identify and fix any issues before going live. Test all possible scenarios, including data retrieval, data entry, and error handling, to ensure smooth operation. Involve end-users in the testing phase to gather feedback and make necessary adjustments.
9. Monitor and Maintain
After the integration goes live, continuously monitor its performance to identify issues and ensure smooth operation. Regularly update your medical system and the integration components to add new features, fix bugs, and maintain compatibility with updates from Epic.
Oleksandr Andrieiev Quote:
“Successful EHR integration is more than a technical endeavor—it’s a cultural transformation. Engaging stakeholders, ensuring infrastructure readiness, and prioritizing user training can make the difference between a system that disrupts workflows and one that enhances care delivery.”
When Epic Medical Software Is Not a Good Fit: Common Cases
Although integrating Epic or Cerner EHR can bring numerous benefits to clinics, there are a few cases where these systems might not be the best fit. Make sure your medical company isn’t on the list below before you start the integration process.
Smaller Clinics with Limited Budgets
Both Epic and Cerner offer extensive functionalities designed for larger organizations with significant budgets. For smaller clinics, the high costs of implementing and maintaining these EHRs can be too much to bear.
Simple Workflows and Basic EHR Needs
Entities with straightforward workflows and basic EHR needs may find Epic and Cerner overly complex and unnecessary. A simpler EHR solution could be more appropriate and cost-effective for them.
Lack of Technical Infrastructure
Healthcare facilities without robust infrastructure and technical expertise may struggle with Epic and Cerner. These systems require significant technical support, which can be challenging for facilities lacking these resources.
Rapid Deployment Needs
Organizations needing quick EHR deployment might find Epic and Cerner impractical due to lengthy implementation time. Custom-made and faster-deploying EHR systems can be more suitable in this case.
Limited Customization Requirements
For providers with minimal customization needs, the extensive configuration of Epic and Cerner may be unnecessary. Justifying the time and effort to customize these systems can be hard.
Niche Specialties with Unique Requirements
Clinics in niche specialties with unique workflows may need tailored EHR solutions. Epic and Cerner may not cater to these specific needs as effectively as custom-made systems.
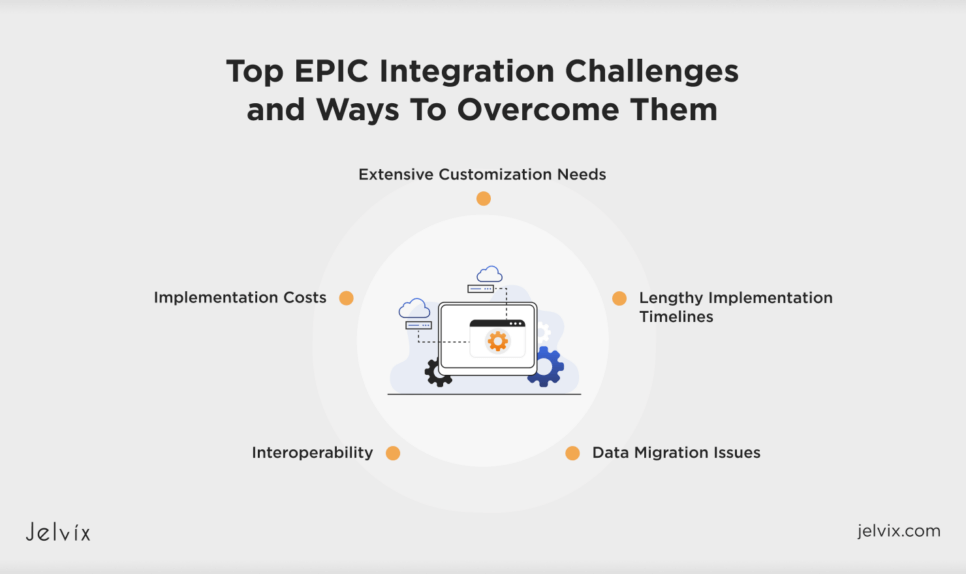
Top EPIC Integration Challenges and Ways To Overcome Them
Integrating EPIC and Cerner EHRs can significantly enhance healthcare operations, but the process comes with a set of challenges. Addressing them allows medical organizations to achieve a smoother integration process, leading to better operational efficiency and patient care.
Interoperability
Achieving seamless data exchange between EPIC and other healthcare systems can be difficult, leading to data silos. Ensure using standardized protocols like HL7 and FHIR to support interoperability. Engage in planning and collaboration with IT teams and third-party vendors to ensure smooth data integration and exchange.
Implementation Costs
The high costs of implementing and customizing EPIC or Cerner can strain budgets, especially for smaller clinics. Conduct a cost-benefit analysis to identify essential features at first and consider phased implementation to spread costs over time.
Extensive Customization Needs
Customizing EPIC and Cerner can be time-consuming and complex. Work closely with experienced consultants who can provide expertise in such implementations. Use their professional advice to ensure that configurations meet your exact requirements without unnecessary delays.
Lengthy Implementation Timelines
The integration process for EPIC and Cerner can take several months to over a year, delaying operational benefits. To tackle this, develop a detailed project plan with clear milestones and deadlines. Assign project managers to oversee the process and regularly make adjustments as necessary to stay on track.
Data Migration Issues
Transferring data from legacy systems to EPIC or Cerner can be complex and prone to errors. You can develop a data migration strategy that includes data cleaning, mapping, and validation. Perform careful testing to ensure data integrity and accuracy before the final migration.
How To Integrate EPIC EMR with Your Health App?
Integrating Epic EHR with your health app can enhance patient care and improve data accuracy. However, you need to be attentive and follow a strict process for successful integration.
Ensure Epic Compatibility
The first thing to do is confirm that your app is compatible with Epic EHR. This involves understanding Epic’s technical requirements and making sure your system can meet them. Compatibility helps prevent technical issues during integration and ensures effective communication between your app and the EHR.
Register with Epic
The next step is to create an account on the Epic website. The registration process typically involves providing details about your app and its intended use. Registration ensures your app complies with interoperability standards, enabling seamless data exchange.
Assess Available Data
Evaluate the types of data your health app needs to access from the Epic system. Identify key data points such as patient records, appointment schedules, and clinical notes vital for your app’s functionality. This assessment aids in planning the integration and ensures your app can retrieve and use the necessary information freely.
Get the API Key
Request an API key from Epic to access their FHIR endpoints. Once you have the key, test the endpoints to ensure they provide the data your app requires. This will help validate the connection between your app and the Epic EHR, ensuring reliable data access and integration.
Integrate Your App with Epic
Developing the integration between your app and Epic includes configuring API calls, mapping data fields, and ensuring secure data transfer. Proper implementation ensures that data flows seamlessly. Testing during this phase helps identify and resolve any issues.
Explore effective strategies to optimize EHR systems and maximize your software investment for improved efficiency and better healthcare outcomes.
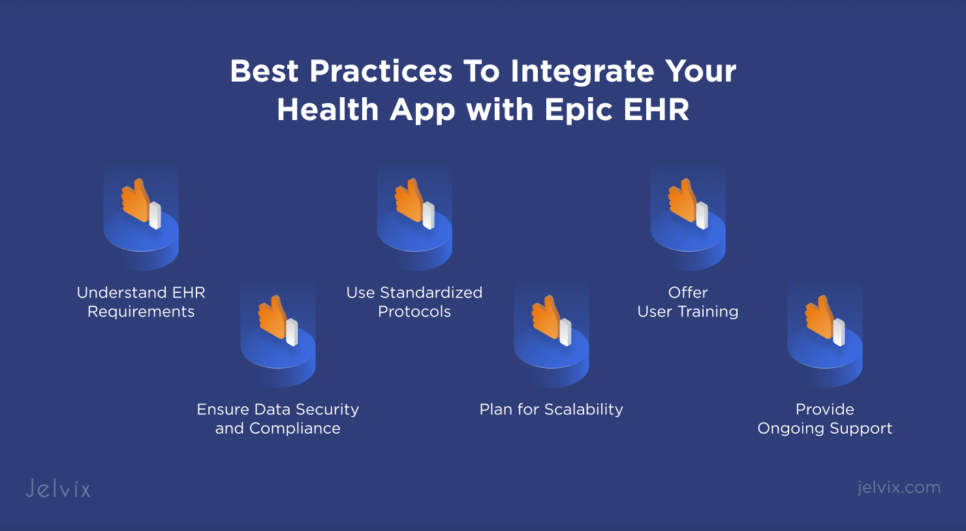
Best Practices To Integrate Your Health App with Epic EHR
Integrating your app with EHR systems like Epic and Cerner can greatly enhance the functionality and efficiency of your services. Make sure to follow the best practices to make this integration truly valuable.
Understand EHR Requirements
Before starting the integration, make sure you understand the technical requirements and capabilities of the chosen EHR. Get familiar with their APIs, data formats, and integration protocols. This will help your app interact with EHR seamlessly.
Ensure Data Security and Compliance
Make sure to comply with healthcare regulations like HIPAA. Ensure that your integration meets all security standards to protect patient data. Implement encryption protocols, secure access controls, and audit logs to maintain data integrity and confidentiality.
Use Standardized Protocols
Use standardized protocols like HL7 and FHIR for data exchange. They support interoperability and ensure that your app can communicate effectively with Epic or Cerner, depending on which one you choose.
Plan for Scalability
Design your integration with scalability in mind. As your user base grows, your app must handle increased data volume and transaction loads. Ensure your infrastructure can scale seamlessly to accommodate growth without compromising performance.
Offer User Training
Offer comprehensive training for all users to ensure they understand how to use the integrated system effectively. Provide user manuals, tutorials, and hands-on training sessions to help users become comfortable with the new system and workflows.
Provide Ongoing Support
Offer ongoing support to address any issues that arise post-integration. Ensure that users have access to technical support and resources to help them navigate any challenges and maximize the benefits of the integrated system.
Cost Considerations for Epic and Cerner Integration
Integrating your health app with Epic or Cerner involves significant investments. Understanding and planning for these cost considerations can help you manage your budget effectively.
Software Licensing Fees
Both Epic and Cerner require licensing fees for using their software and APIs. These fees can vary based on the scope of integration and the size of your company. Make sure to account for initial licensing costs as well as any recurring fees.
Implementation and Customization
Customizing the EHR system to fit your specific needs involves substantial development work. This includes configuring the system, developing custom interfaces, and tailoring workflows to match your operational requirements. All these add to the cost of integration.
Data Migration
Depending on the volume of data, transferring it from legacy systems to the new EHR can be complex and costly. Data migration costs include data extraction, cleaning, mapping, and validation to ensure accuracy and integrity.
Training and User Education
Training healthcare, administrative, and IT staff on the new system is another thing to consider. The associated costs usually include developing training materials, conducting workshops, and providing ongoing support to ensure users are comfortable with the new EHR.
Ongoing Maintenance and Support
Post-implementation, ongoing maintenance, and support are necessary to keep the system running smoothly. This includes regular software updates, troubleshooting, and technical support. Budget for these recurring expenses to ensure the long-term success and reliability of the integrated system.
Consultant and Professional Services
Hiring external consultants or professional services can provide valuable expertise and ensure a smoother integration process. Costs for these services include consulting fees, project management, and specialized technical assistance.
Compliance and Security
Ensuring compliance with healthcare regulations like HIPAA and implementing robust security measures involves additional costs. These include security audits, encryption technologies, and compliance certifications. Investing in security and compliance helps protect patient data and avoid legal penalties.
Contingency Budget
You can face unexpected issues during the integration process, leading to additional costs. Setting aside a contingency budget helps manage unforeseen expenses and ensures that the project can keep going smoothly.
How Jelvix Can Assist You with Epic EHR Integration
Every healthcare organization has specialized needs and goals that influence the whole EHR integration process. At Jelvix, we focus on helping enterprises implement EHRs like Epic and Cerner, taking into account their specific requirements, limitations, and budget constraints.
If you’re having trouble integrating a ready-made EHR into your settings or aim to develop a custom FHIR-based EHR solution, our experts are here to help. Contact us for a personalized consultation on your unique business needs.
Looking to grow your business?
Hire a team of professionals dedicated to delivering exceptional results.