In hospital workflows, every second is crucial, and Electronic Health Records (EHR) play a key role in the process. While EHRs aim to streamline healthcare services and enhance clinical efficiency, they often encounter challenges that can hinder seamless care delivery.
The main issues stem from the complexities of technology adoption and the learning curve associated with new systems. However, there’s a solution in sight. Jelvix offers insights that transform EHR challenges into opportunities for improved operations, enhancing patient care, and bolstering financial health.
Are you ready to turn your EHR system from a hurdle into an asset? Join us as we delve into strategies to optimize your hospital’s workflow, reduce inefficiencies, and raise the quality of your services.
What Are Key EHR Adoption Challenges?
A rapid transition towards a digitized healthcare system brings numerous benefits but also presents several challenges. Electronic Health Records (EHR) are at the center of this transformation, providing a more streamlined, efficient, and comprehensive system for patient care. However, the road to a fully functional EHR system has obstacles.
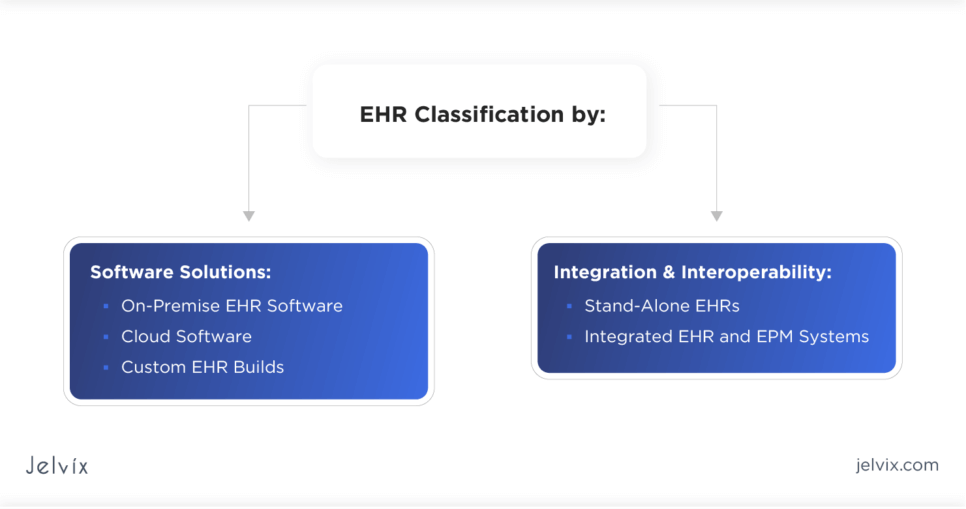
Navigating The EHR Classification
Embarking on the EHR journey propels you into a constellation of tech choices, each with its orbit of complexities. Whether you’re plotting EHR implementation steps or sculpting an EHR workflow, understanding the spectrum of systems is critical. Let’s navigate these terrains to ensure your EHR is a beacon of efficiency in your healthcare galaxy.
Software Solutions
- On-Premise EHR Software:
Consider on-premise EHR systems as a robust and secure solution for managing patient data, offering healthcare providers direct control over their IT environment. It’s a stronghold for data, offering extensive tailoring for EHR in hospitals, ensuring your clinical workflows in healthcare are as unique as your patient care blueprint.
- Cloud Software:
Cloud Software solutions provide a dynamic and scalable option for healthcare data management, with cloud-based agility that supports improving workflow in healthcare without the ballast of hardware. It’s a boon for those pondering how to improve EHR with scalability and remote access.
- Custom EHR Builds:
In the realm of clinical workflows in healthcare and the implementation of electronic health records in hospitals, hybrid EHR software emerges as a versatile choice. This adaptable solution allows organizations to select the hosting approach that best aligns with their needs, seamlessly blending on-premises and cloud-based capabilities.
Integration and Interoperability
- Stand-Alone EHRs:
Stand-alone EHR systems are designed for focused and specialized management of patient records, serving as a dedicated resource for healthcare providers. Their simplicity is their strength, providing straightforward, standalone systems that cater to focused needs without the entanglements of integration.
- Integrated EHR and EPM Systems:
Integrated EHR and EPM systems represent a comprehensive management solution, orchestrating both clinical and administrative tasks within a unified platform. They are pivotal in how to improve workflow in medical office settings, offering a suite of tools in one cohesive unit.
Also, EHRs can be certified and non-certified:
Certified EHRs are the gold-sealed emissaries of the EHR domain, adept at deciphering the interoperability codes. They exemplify electronic medical records best practices, easing the EHR workflow between departments and facilities.
Understanding the nuances of these EHR types is not just for tech aficionados; it’s an essential quest for any healthcare practice. It’s about ensuring that your chosen EHR not only houses your data but also amplifies the symphony of care you provide, resonating through every interaction and intervention, improving communication, and setting the stage for excellence in patient care.
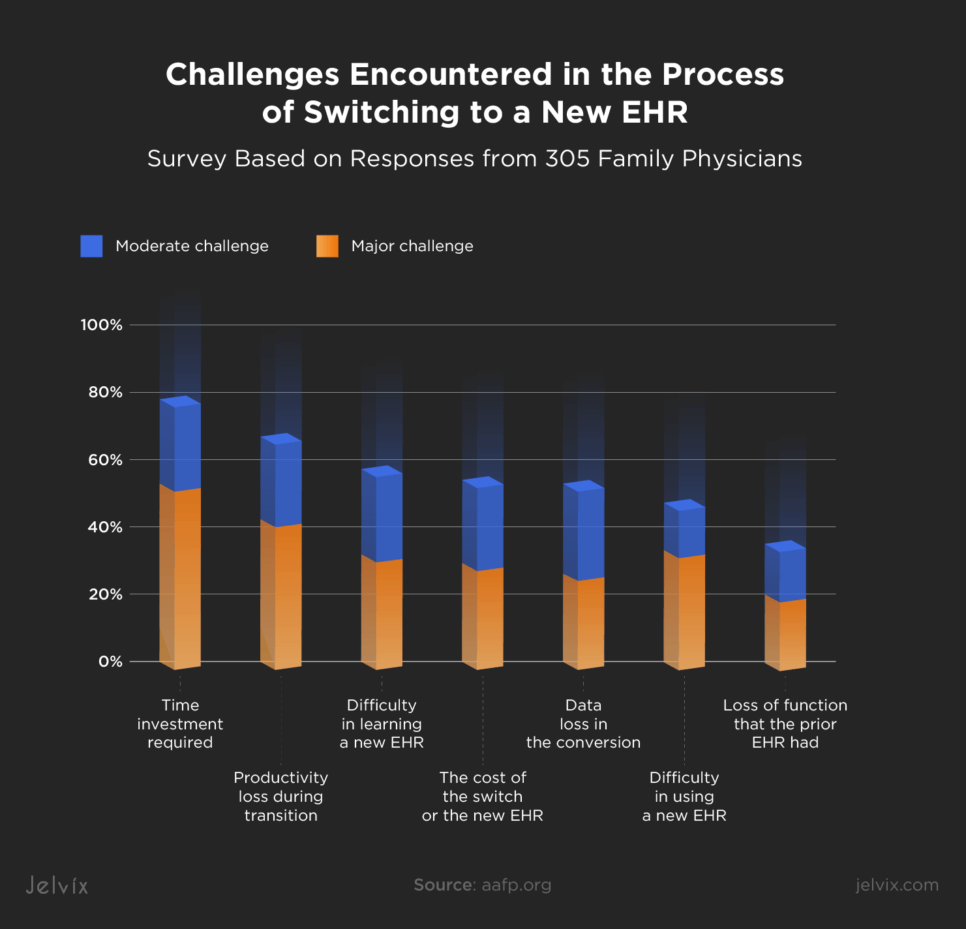
Why Are Some Physician Practices Not Switching to EHR Yet?
Despite the clear advantages of Electronic Health Records (EHR), a number of physician practices have yet to embrace this technology. Their hesitance is largely due to a variety of practical concerns that, when properly addressed, could facilitate a more efficient adoption process. Let’s break them down and take a look at some potential solutions you may implement.
- Investment Anxiety: High initial costs and the anticipated ongoing expenses for maintenance and updates can be intimidating, especially for smaller practices.
-
- Solution: Utilize financial aid like grants and structure payments flexibly. Emphasize long-term savings and improved billing accuracy. Real-world success stories can also illustrate the financial viability of EHR systems.
- Implementation Complexities: The numerous EHR implementation steps required can be daunting, with practices fearing data mishandling and compliance issues.
- Solution: A tailored, step-by-step guide and a dedicated support team can simplify the EHR implementation steps. Success stories add credibility and reassurance
- Training Hurdles: Shifting to a digital system disrupts established workflows, leading to a temporary dip in productivity and patient service delays.
- Solution: Tailored training and ongoing support can ease this transition. By involving staff in EHR selection and providing quick-reference materials, practices can maintain their EHR workflow during the switch.
- Productivity Concerns: Adjusting to a new EHR system can temporarily slow clinic operations – a worry for fast-paced environments.
- Solution: Partner with tech providers to ensure robust protections and educate staff on digital security practices.
- Cybersecurity Woes: The risk of data breaches during the digital transition is a significant barrier
- Solution: Gradual implementation and setting realistic productivity goals during the transition can help maintain a functional EHR workflow.
Now, moving from why practices are holding back, let’s delve into the digital realm’s actual performance. When it comes to EHR systems, speed is a game-changer. That’s why it’s critical to pinpoint and untangle the most common bottlenecks that might slow down EHR operations, ensuring that these digital tools don’t just work but work efficiently, keeping pace with the bustling life of a busy clinic.
Most Common Bottlenecks Causing Slow EHR Performance
In the fast-paced world of healthcare, enhancing clinical workflows through EHR systems is pivotal, but inefficiencies can arise, stymieing their potential to streamline care. Tackling these bottlenecks not only refines EHR workflow but can also be a catalyst for improved practice revenue.
- Server Overload. The crux of EHR in practice, particularly for on-premises systems, is maintaining performance under heavy data loads. Scalable services on cloud-based solutions can prevent slowdowns, ensuring that the EHR workflow remains uninterrupted and patient care is delivered efficiently.
- Software Glitches. Even with robust EHR implementation steps, software issues can crop up if EHR systems are not updated consistently. Thinking through possible future problems and doing regular compatibility checks with other in-house tools are vital for a smooth EHR workflow and are considered electronic medical records best practices.
- Inadequate Hardware. Robust hardware underpins an effective EHR system, directly influencing the speed and efficiency of the EHR workflow. Upgrading outdated machinery and fortifying network strength can alleviate this issue, enabling faster patient data processing and contributing to improved workflow in healthcare. But, you can always turn to cloud-based solutions and concentrate on software only, leaving hardware as a headache for others.
- Data Clutter. Data clutter is a common challenge in EHR systems. It can slow down system performance and hinder quick data access. To tackle this, consider AWS’s storage options like S3, which offers various speed and cost ratings. For instance, S3 Standard (3/3) suits frequently used files, while S3 Glacier Deep Archive (1/1) is for rarely accessed data. AWS’s “Intelligent Tiering” can automate data migration for cost-effectiveness, aligning with EHR best practices.
- Integration Issues with Other Systems. Optimal EHR workflow hinges on the EHR’s ability to integrate with other software tools used in healthcare settings. Fostering a seamless link with systems handling billing and scheduling avoids duplication of effort and fuels more efficient clinical workflows in healthcare.
By proactively resolving these EHR bottlenecks, healthcare providers can markedly refine their EHR workflow. Next, we’ll explore strategic approaches to leverage EHR features effectively to boost medical practice revenue.
How Leveraging EHR/EMR Can Boost Your Medical Practice’s Revenue
Electronic Medical Records (EMR) are digital versions of paper charts in a clinic detailing patient histories and treatments. While EMRs focus on one practice, Electronic Health Records (EHR) share patient data across multiple healthcare settings. Both systems streamline patient care and administration, which can boost a practice’s revenue through efficient billing and improved patient management.
- Efficient Billing. Automated billing processes reduce errors, ensuring that practices are not leaving money on the table. Accurate coding and billing diminish the risk of claim rejections and denials.
- Enhanced Patient Experience. An efficient EHR workflow and EMR workflow leads to shorter waiting times, quicker diagnosis, and more time for patient-physician interactions. This improved patient experience can lead to higher patient retention and referrals.
- Data-Driven Decision Making. EHR systems provide a goldmine of data. By analyzing this data, practices can identify patterns, understand patient demographics better, and optimize services for maximum profitability.
- Reduced Overhead Costs. With the digitization of records, the costs associated with paper, storage, and manual labor decrease. Additionally, EHR systems can help identify inefficiencies in operations, leading to further cost savings.
- Streamlined Scheduling. With EHR systems, practices can better manage patient appointments, reducing no-shows and ensuring optimal utilization of resources.
Top Metrics to Track the Return on Investment in EHR
While EHR systems offer numerous qualitative benefits, it’s equally essential to have quantifiable metrics in place to gauge the exact ROI. These metrics can be assessed short-term post-EHR system implementation and evaluated for long-term impacts as more data accumulates.
- Increased Revenue. The primary evidence of a successful ROI from EHR is an uptick in revenue. EHR systems provide superior automation capabilities, from record-keeping and scheduling to patient messaging. Such enhancements allow healthcare professionals to work with greater efficacy. Adding one to two consultations daily can augment around $80,000 in procedural revenues for each physician, as per EHR Intelligence.
- Lower Expenses. UCSF’s research indicates that EHR adoption leads healthcare establishments to slash annual administrative costs by approximately $42,500 per FTE provider. EHR implementation facilitates savings in:
- Infrastructure and Administrative Costs. Cloud-based EHR systems obviate the need for on-premise servers and constant infrastructure enhancements. Plus, electronic records liberate spaces previously cluttered with paper documents.
- Labor Costs. EHR-powered medical teams operate faster, diminishing the necessity for extra specialists and inflated working hours.
- IT Costs. EHR systems offer comprehensive solutions that reduce IT costs by eliminating the need to manage multiple disparate software applications. Custom-developed EHRs, tailored to specific practice needs, can provide even greater value by replacing a myriad of limited-function tools, ensuring seamless integration and functionality aligned with the unique workflows of a practice.
- Human Error Costs. EHR reduces the likelihood of costly mistakes, thus safeguarding funds that might otherwise be lost to incorrect treatments or data breaches.
- Operational Efficiency. Advanced software facilitates healthcare institutions to track variables like patient flow and bed availability, allowing for better resource allocation. Efficient use of equipment, bolstered by scheduling and analyzing usage data, is another advantage. Such indicators can echo the ROI. When internal systems perform optimally, the ROI invariably escalates.
Tips on How To Maximize EHR ROI
EHR systems are designed to revolutionize healthcare by streamlining operations and improving care coordination. To maximize their ROI, healthcare providers should adopt these strategic steps:
- Get Buy-In Across the Board. The impact of EHRs isn’t limited to clinical activities. EHRs must enhance numerous operations and harmonize workflows across departments to truly harness their ROI. Engage all stakeholders, from IT and Finance to Front Office staff, during decision-making.
- Provide Strong Leadership, Communication, and Training. Ensure clear articulation of the EHR implementation strategy. Be prepared for an adjustment phase and design an effective training program to acquaint all users with the system’s nuances.
- Improve Staffing Efficiency While Enhancing Operating Margins. Labor costs form a substantial portion of a provider’s operational expenses. Utilize insights from EHR and ERP data to optimize staffing, potentially saving U.S. healthcare providers over $77 billion in the coming five years, as estimated by Accenture.
- Development of custom EHR solutions. Tailor-made systems ensure a perfect fit for specific clinical workflows, patient management needs, and data analysis, avoiding the one-size-fits-all limitations of off-the-shelf software. Custom development can offer scalability, flexibility, and integration capabilities that can significantly drive up long-term savings and efficiency, leading to a stronger ROI.
- Integrate Practice Management. Interlinking EHRs with practice management solutions can greatly enhance ROI. Such integration offers a centralized system, promoting efficient billing, effective revenue cycle management, and participation in value-based care programs.
- Discover New Value from EHR Data. EHR systems house invaluable data. Utilizing analytics can yield insights into optimizing value-based incentive schemes, refining billing processes, and enhancing population health initiatives. Investing in staff skilled in both technical and clinical domains is paramount to unlocking these insights.
It’s important to remember that mere EHR adoption doesn’t guarantee heightened profitability. Select a vendor offering continued support and ensuring their product adapts to the establishment’s evolving needs. By initially addressing specific requirements and challenges, practices can better leverage the information within the EHR, guaranteeing an optimal return on their tech investments.
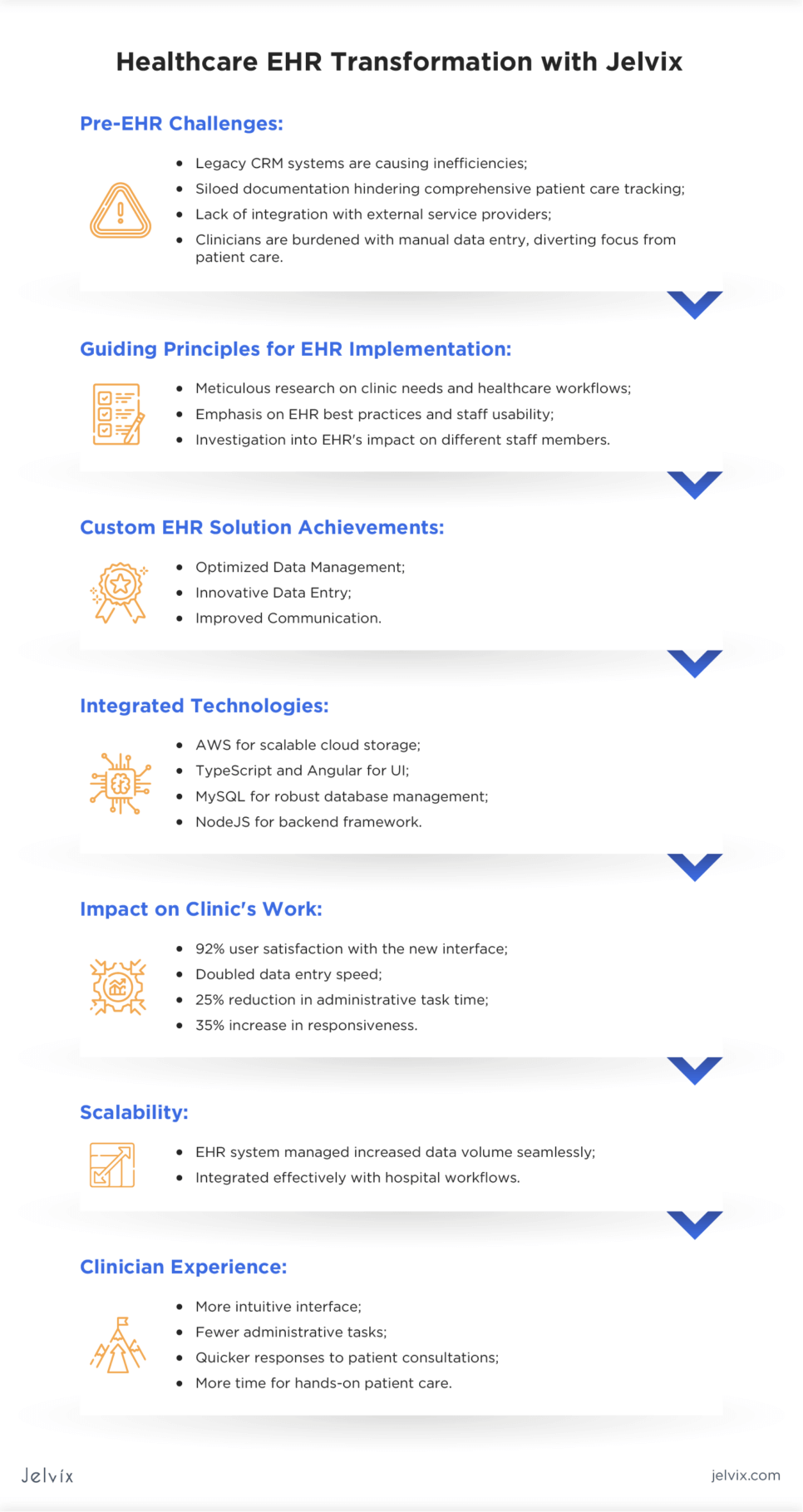
Jelvix’s Case Study: The Transformation of Healthcare with Electronic Health Records
Jelvix, leveraging technology to streamline UK healthcare, successfully transitioned numerous clinics from traditional to electronic records. Our collaboration addressed specific challenges such as data migration, system integration, and user adoption, resulting in enhanced efficiency and patient care. Dive into our case studies for detailed insights into our approach and tangible benefits realized by our partners. For a deeper understanding of our methodologies, visit our Principles Page.
Pre-EHR Challenges Identified
- The legacy CRM systems were not designed for modern healthcare, causing inefficiencies;
- Documentation was siloed across departments, making comprehensive patient care tracking challenging;
- A lack of integration with external service providers hindered smooth information exchange;
- Clinicians were bogged down with manual data entry, diverting their focus from patient care.
Guided by the importance of EHR in hospitals, Jelvix dove into the intricate EHR implementation steps. We began with meticulous research, understanding the unique needs of each clinic and the nuances of hospital and clinical workflows in healthcare. Our approach was two-fold: we emphasized the EHR best practices and investigated how does EHR make different staff members work easier.
Jelvix’s customized the EHR solution significantly advanced clinical efficiency and patient engagement. Key achievements included:
- Optimized Data Management. Advanced data storage solutions ensured robust handling of medical records, establishing a new standard for best practices in EMR.
- Innovative Data Entry. Integration of cutting-edge text recognition and voice input technologies minimized manual data entry, saving time and reducing errors.
- Improved Communication. Enhanced communication tools facilitated better patient-physician interactions, leading to more effective use of health records and improved clinical outcomes.
What Technologies We’ve Integrated:
- AWS for scalable cloud storage solutions;
- TypeScript and Angular for a responsive user interface;
- MySQL for robust database management;
- NodeJS for the backend framework.
Custom EHR Solution’s Impact on Clinic’s Work:
User Satisfaction:
92% of users expressed satisfaction with the new user-friendly interface, enhancing the EHR workflow for staff and patients.
Time Savings:
Data entry speed doubled due to advanced recognition technologies, boosting EHR workflow efficiency.
Improved Efficiency:
Time for completing administrative tasks dropped by 25%, aligning with EHR best practices and allowing more focus on patient care.
Seamless Communication:
Integrated tools increase responsiveness by 35%, improving clinical workflows in healthcare.
Scalability:
The EHR system managed the increase in data volume and seamlessly integrated with the hospital workflows, demonstrating the effective scalability of EHR implementation.
For clinicians, the EHR transformation was palpable. A more intuitive interface meant fewer administrative tasks, quicker responses to patient consultations, and more time for hands-on patient care.
Learn how CRM-EHR integration optimizes healthcare by combining patient insights and improving workflow efficiency for better care delivery.
Consider Jelvix as Your Trusted Tech Partner
In the evolving landscape of healthcare digitization, picking the right partner is paramount. Jelvix stands as a testament to bridging technological brilliance with healthcare expertise. Our journey in EHR implementation showcases not only our prowess in software development but also an in-depth understanding of the intricate EHR workflows that drive healthcare.
The Technology and Team Required for EHR Development
The genesis of any successful EHR implementation lies in the backbone of a skilled and dedicated team. Before delving into the nitty-gritty of the implementation, it’s crucial to gather a qualified team capable of designing the EHR’s workflow and overseeing its software development.
Lead Physician. At the heart of this team is the Lead Physician. This isn’t just any medical expert. This tech-savvy healthcare specialist will steer the EHR implementation steps from a medical lens. Their pivotal role is to act as a bridge – a mediator between the tech developers and the end-users, which predominantly include doctors and patients. Their insights ensure that the system is tailored to cater to the real-time needs of EHR in practice, thereby guaranteeing optimized user experience and functionality.
Project Manager. Complementing the Lead Physician is the Project Manager. This stalwart serves as another crucial bridge between the software vendor and the client. Their task list is exhaustive, from tracking the project’s progress and overseeing the EHR implementation timeline to troubleshooting any potential hiccups. Their role ensures the smooth transition of the project from the drawing board to real-world application.
Choosing Jelvix as your tech ally means entrusting your project to a team that understands the delicate balance between EHR best practices and practical hospital workflows. Their approach isn’t just about integrating electronic health records in hospitals but also ensuring that these systems facilitate improved patient care and seamless communication across the healthcare spectrum.
Conclusion
Adopting EHR systems is a transformative step towards smarter, patient-centric healthcare delivery. It’s not just about installing new software; it’s about mastering EHR implementation steps and refining clinical workflows for enhanced care. While the journey may present hurdles, with expert guidance and in-depth resources like those offered by Jelvix, healthcare providers can confidently embrace digital evolution. For a comprehensive understanding and to explore our full case studies, we invite you to connect with us. By completing a simple feedback form, you can gain exclusive access to our detailed case analysis, sent directly to your inbox.