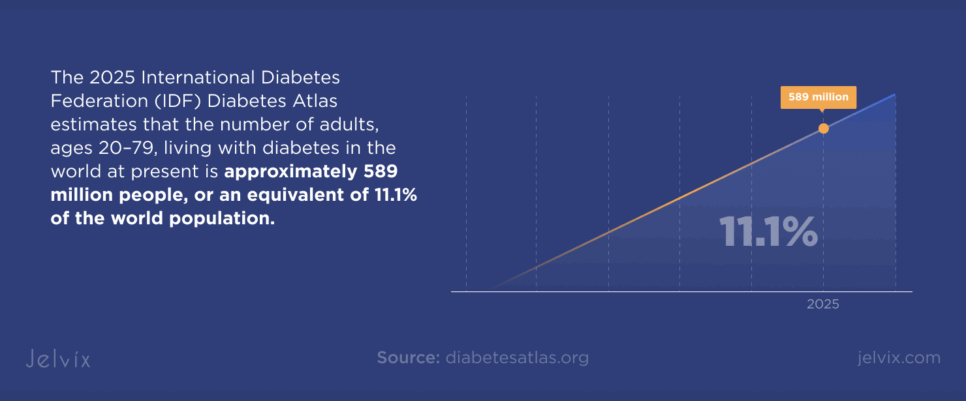
Diabetes is a rapidly escalating global challenge that requires a response that offers precision with technological aid. The 2025 International Diabetes Federation (IDF) Diabetes Atlas estimates that the number of adults, ages 20–79, living with diabetes in the world at present is approximately 589 million people, or an equivalent of 11.1% of the world population. That number is set to reach 853 million in 2050, a 46% increase, leading to a significant burden on healthcare systems.
The scale of the impact extends beyond prevalence. In 2024, diabetes accounted for 3.4 million deaths (one every nine seconds), while driving healthcare expenditure to at least USD 1 trillion, a 338% increase in 17 years.
Type 2 diabetes accounts for over 90 % of all cases and is driven by a host of socio-economic, demographic, environmental, and genetic factors. And urbanization, an aging population, sedentary behavior, and increasing levels of obesity also contribute to this rise.
In this environment, remote patient monitoring diabetes solutions are central to building resilient care models. From continuously monitoring blood glucose to connected insulin pumps, real-time analytics, and patient-facing mobile applications can all converge outside the walls of a clinic and allow an extension of care.
This results in highly secure, interoperable data flows when deployed using advanced API frameworks.
This article will examine how scalable device networks for diabetes care can be designed with APIs as the core enabler of interoperability. It will cover the technical foundations for network architecture, the integration strategies for diverse medical devices, the best practices for security and compliance, and the approaches to ensure performance at scale.
At the end of it, you will have a blueprint that you or your care organization can use to build a patient-centered connected health infrastructure model for diabetes.
Growing Trend of Combining Chronic Care Management (CCM) and Remote Patient Monitoring (RPM)
The integration of RPM diabetes programs with chronic care management strategies is transforming long-term disease oversight. According to the Alliance for Connected Care, in 2023, 81% of clinicians reported using RPM, marking a 305% increase since 2021, driven by its capacity to lower hospital readmissions, improve patient outcomes, expand preventive care, and enable hospital-at-home delivery models.
A CCM medical device connected to a unified platform sends a steady stream of health data directly to care teams. This constant visibility allows for rapid adjustments to treatment plans, with decisions informed by real-time evidence rather than retrospective observations.
Within diabetes care, remote diabetes monitoring shifts the focus from episodic appointments to continuous engagement. Glucose fluctuations, insulin dosing behavior, and patterns in patient activity can each be tracked as individual data streams, then merged into a single actionable record.
At the heart of it all are APIs, which transform numerous outputs from devices into the formats that can be understood by clinical systems.
These systems provide a flexible, performance-based environment in which CCM and RPM work together to create seamless, tech-supported care for those with ongoing medical issues.
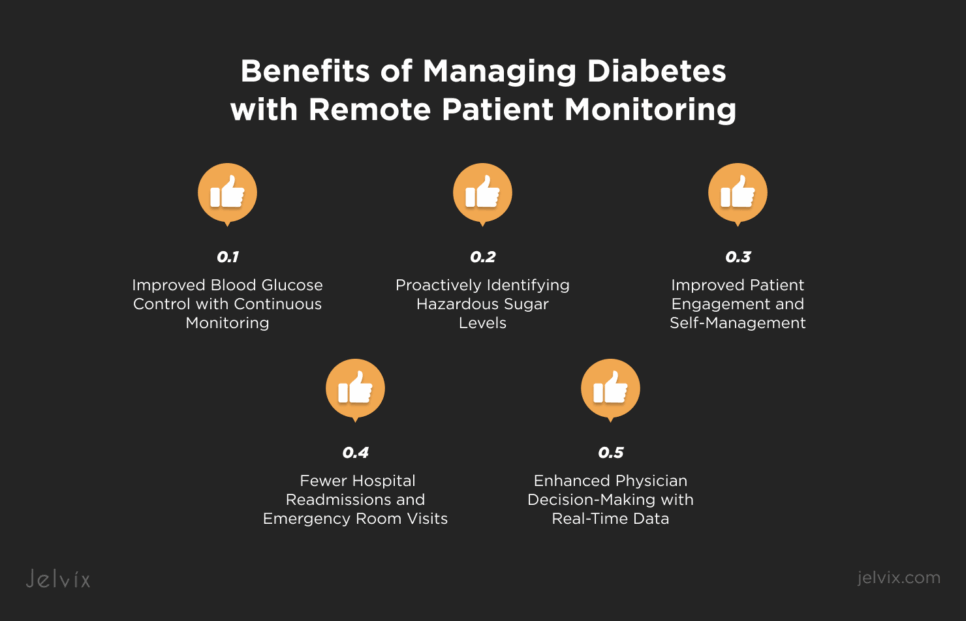
Benefits of Managing Diabetes with Remote Patient Monitoring
Improved Blood Glucose Control with Continuous Monitoring
Among more modern remote patient monitoring ecosystems, continuous glucose tracking serves as a signal within a connected data architecture. The sensors send readings to a secure platform, where clinicians can access both real-time and historical data, with no latency. This allows for manipulation of therapy on a definitive trend instead of ballpark numbers.
Proactively Identifying Hazardous Sugar Levels
When it comes to glucose readings, data pipelines in RPM systems can immediately set off automated red flags as soon as the levels pass critical thresholds. These thresholds are set up by physicians case-by-case so that they (the alerts) pertain only to clinically relevant data. The feedback loop means intervention can be swift, before things go too far.
Improved Patient Engagement and Self-Management
Patients who can see their own glucose data in real time gain a stronger sense of control over daily decisions. Mobile platforms display patterns and provide prompts that support informed actions. This experience is most effective when supported by robust integration frameworks, such as the seamless integrations of a chronic care management solution, where devices work as part of a unified ecosystem.
Fewer Hospital Readmissions and Emergency Room Visits
As a result of this and the continuous digital connection between patient and provider, clinical teams can intervene when changes occur well in advance of other health crises. Remote interventions are delivered aligned to treatment and help reduce the need for hospital admission.
Enhanced Physician Decision-Making with Real-Time Data
With all monitoring devices converging under one interface, healthcare providers can make decisions with the full picture in mind. APIs guarantee that all data points are in sync and validated to form a reliable foundation for treatment planning.
Common Devices Enabling RPM in Diabetes Care
Continuous Glucose Monitors (CGMs)
These are among the most sophisticated diabetes remote monitoring devices because they deliver uninterrupted glucose data without manual input. A small sensor under the skin measures interstitial glucose through electrochemical reactions, then sends readings via Bluetooth or NFC to a receiver or mobile app.
This, in turn, relays the values to a diabetes management system where these are analyzed historically. This method enables physicians to track glycemic changes as they occur and intervene at the right time.
Smart Insulin Pens and Pumps
Smart insulin pens record every administered dose, including the exact time and quantity. Additionally, pumps take it one step further by providing basal and bolus insulin delivery automatically up to 0.05 units at a time (or even more finely).
These devices connect to CGM data via secure APIs, providing care teams a real-time look at the glucose impact of insulin delivery. The integration furthers home health diabetes management programs and serves as the infrastructure that vendors use for automated dosing recommendations.
Wearable Fitness and Activity Trackers
Wearables expand the scope of monitoring by adding physiological context to glucose trends. Devices with an accelerometer, gyroscope, and heart rate monitor analyze movement patterns, effort intensity, and recovery profiles.
By logging their data in the chronic disease management system, they can cross-reference their activity with changes in insulin sensitivity. This other dimension lends some more nuance to both lifestyle advice and pharmacologic changes.
Mobile Health Applications and Connected Glucometers
Connected glucometers transmit fingerstick readings directly to cloud-based platforms, creating a seamless flow of information even when CGMs are offline or not in use. Mobile health apps act as the central access point, showing patients their data in real time while providing providers with an aggregated clinical view.
For diabetes telehealth companies, this software layer unifies device inputs and communication channels, turning fragmented measurements into a coordinated home health diabetes management process.
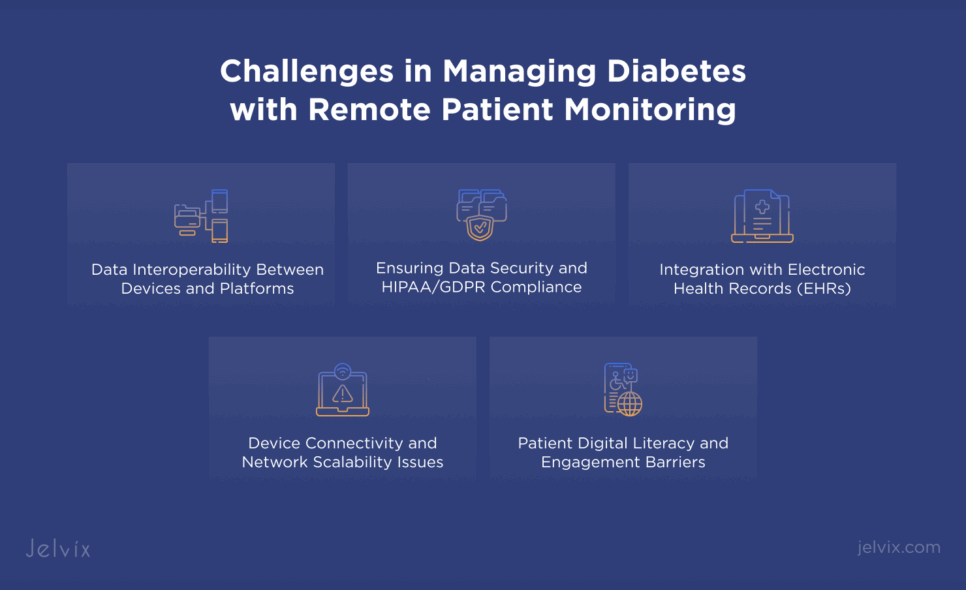
Challenges in Managing Diabetes with Remote Patient Monitoring
Data Interoperability Between Devices and Platforms
Typically, device vendors opt to utilize proprietary protocols that can obstruct cross-platform interfaces for data exchange. Without standardized formats like HL7® FHIR®, integrating sensor outputs into central dashboards requires complex translation layers.
Apart from the fact that this decreases data velocity, it results in synchronization problems and introduces further development effort between surfaces by the interoperability middleware.
Ensuring Data Security and HIPAA/GDPR Compliance
Real-time transmission of patient health data gives rise to a number of attack surfaces, all the way from device firmware to cloud APIs. Finally, being compliant with HIPAA and GDPR means encryption in transit and at rest, token-based authentication, and key rotation on a regular schedule.
This is also where the aspect of detecting malicious traffic patterns in your network layer comes in, and that is something a security model would entail to help prevent an issue from exploding further.
Integration with Electronic Health Records (EHRs)
Integration of RPM outputs into EHR workflows will involve a bidirectional data exchange with minimal lag time. EHR systems have limited data models that cannot accommodate data-rich (longitudinal and dynamic glucose streams) along with device-generated metadata, all in a structured manner.
APIs with event-oriented architectures enable data freshness while also taking care of the throttling limits that legacy systems still require.
Device Connectivity and Network Scalability Issues
Continuous transmission of glucose and dosing data demands high network reliability, especially for home-based deployments. However, if latency spikes or packets are lost, this results in incomplete datasets affecting the accuracy of decision-making.
Edge processing should be needed for scaling to beyond hundreds or thousands of connected endpoints, preventing the consumption of edge bandwidth and central server loading.
Patient Digital Literacy and Engagement Barriers
Good technical solutions can still be suboptimal if patients experience difficulty with onboarding, calibration routines, or the interpretation of visualized trends. Poor understanding of how the device works can easily lead to people not using the device consistently, and hence compromise data quality.
One way to maintain engagement, of course, is with adaptive user interfaces that deliver behavior-tailored complexity over time.
The Role of APIs in Building Scalable Remote Patient Monitoring Networks
API-Driven Interoperability for Multi-Device Ecosystems
Connected devices come in all shapes and sizes, from continuous glucose monitors and insulin pumps to activity trackers and glucometers that transmit data in different formats. Functions as APIs translate proprietary protocols into standard structures like HL7 FHIR or optimized JSON schemas. With LLS, this is maintained while requiring no change to the communication layers on the hardware vendor.
Secure Data Exchange Between Medical Devices and Cloud Platforms
The key to this is APIs, which allow the encrypted exchange of data in both directions between medical devices and cloud services. By using transport-level security with TLS 1.3 along with payload encryption like AES-256, the patient information is protected at every exchange.
Security paradigms based on tokens. For example, OAuth 2.0 and JWT are used to make sure that only authentic systems interact with the data pipeline. API gateways can enforce compliance policies at the edge, logging transactions for HIPAA and GDPR audits while having zero impact on performance.
Real-Time Alerts and Automated Workflows via APIs
When thresholds for glucose variation are breached, APIs act as event triggers, sending actionable alerts to clinicians, updating patient dashboards, and initiating scheduling workflows in care management platforms. Event-driven architectures can connect these alerts to serverless functions, enabling automated dosing adjustments or patient outreach without running persistent backend jobs.
Scaling RPM Solutions Without Losing Performance
As endpoints scale into the thousands, APIs need to remain responsive, even under heavy load. Kubernetes, which is used to manage containerized applications, automatically distributes workloads across the available nodes, whereas load balancers distribute incoming user requests equally among the nodes so that no single node becomes a bottleneck.
Similarly, caching layers (such as Redis) eliminate redundant data calls, and smart rate-limiting maintains serviceability when the infrastructure is shared among other tenants (e.g., major diabetes telehealth companies).
Such APIs in turn enable enriching CGM data with fitness tracker metrics to deliver adaptive dosing recommendations, while insulin pumps are updated through predictive analytics-informed configuration pushes.
Glucometers connected to their systems continuously stream readings right into EHRs, eliminating the need for manual entry and improving consistent continuity across clinical and telehealth environments. These features transform APIs from mere integration mechanisms to the driving forces behind scalable, future-proof RPM networks.
See how we improved chronic care management solution by unifying EHR, IoMT, and lab data through seamless integrations in this healthcare case study.
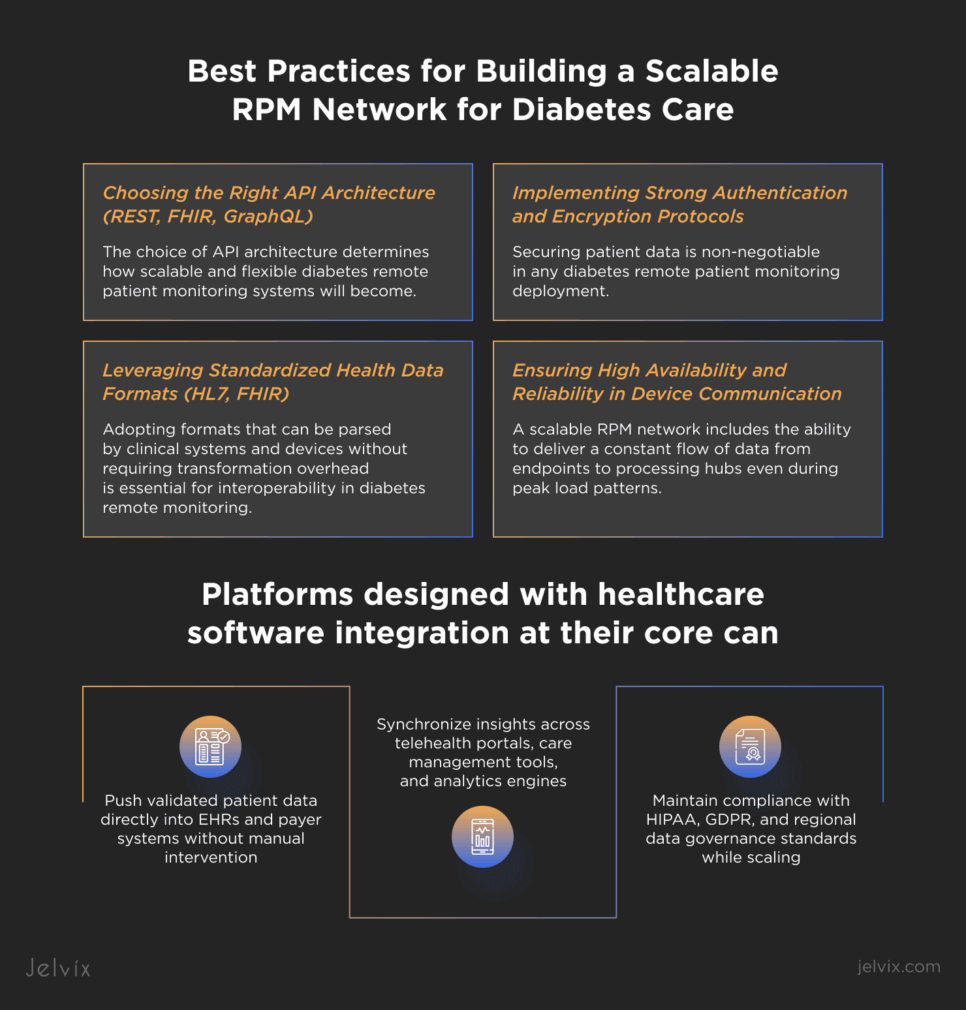
Best Practices for Building a Scalable RPM Network for Diabetes Care
Choosing the Right API Architecture (REST, FHIR, GraphQL)
The choice of API architecture determines how scalable and flexible diabetes remote patient monitoring systems will become. For device-to-cloud communication, REST continues to be the most popular because of its ease and robust platform tooling.
FHIR-based APIs offer native interoperability with healthcare systems and EHRs, which is why they are a smart choice when creating a remote patient monitoring app to seamlessly integrate with clinical workflows in place.
In mobile applications, GraphQL can optimize queries, which ultimately helps to use bandwidth and speed up responses, something that is crucial in cases where every millisecond of latency impacts patient data freshness.
Leveraging Standardized Health Data Formats (HL7, FHIR)
Adopting formats that can be parsed by clinical systems and devices without requiring transformation overhead is essential for interoperability in diabetes remote monitoring. FHIR offers up-to-date, web-friendly resource models to support RESTful interactions, while HL7 offers a strong messaging standard for the interchange of structured health data.
Following these guidelines reduces integration issues and speeds up the onboarding of new device manufacturers.
Ensuring High Availability and Reliability in Device Communication
A scalable RPM network includes the ability to deliver a constant flow of data from endpoints to processing hubs even during peak load patterns. API gateways and failover paths are made redundant so that anything read from the device must reach the central platform without any human intervention.
Pre-validation of glucose readings at the edge before transmission saves us from any corrupted data entering the pipeline and provides the accuracy of technology to use in managing a patient’s diabetes, where clinical decisions rely on instant visibility into such granular data.
Implementing Strong Authentication and Encryption Protocols
Securing patient data is non-negotiable in any diabetes remote patient monitoring deployment. Authentication layers should use OAuth 2.0 or mutual TLS to verify devices, and payload encryption with AES-256 guarantees confidentiality. Security is further enhanced with token expiration policies, key rotation schedules, and intrusion detection mechanisms.
Your encryption standard should apply to in-transit and at-rest data, thus ensuring compliance with standards like HIPAA or GDPR and other healthcare-specific protection frameworks without performance compromise.
Future of Remote Patient Monitoring in Diabetes Care
At its essence, the future of telehealth for diabetes will depend on cutting-edge AI predictive analytics, which can forecast hypoglycemia and hyperglycemia before they happen. Now, we have machine learning models that can be trained on the continuous streams of data from remote glucose monitoring devices to detect non-linear, complex patterns that would be difficult to spot by manual observation.
These systems will often provide actionable predictions hours in advance, enabling patients and clinicians to take proactive measures by taking into account factors like insulin dosing history, activity levels, meal timing, and even sleep quality. With this paradigm shift, glucose management moves from reactive cure to proactive optimization.
As value-based care becomes more prevalent in healthcare ecosystems, remote patient monitoring will inevitably be incorporated into reimbursement frameworks. These RPM-derived insights will be automatically pushed into payer and provider systems by platforms designed for smooth integration with current healthcare software, guaranteeing that interventions are recorded, results are monitored, and cost savings can be confirmed.
Combined with clinical performance, there is significant alignment to be done, especially for large provider networks looking for functional diabetes home care management models.
However, personalized medicine and digital therapeutics will make a fine-line distinction regarding how RPM occurs at the individual level. Algorithms can customize interventions based on the patient’s specific glucose response curve instead of some predefined treatment schedules. The expansion will include:
- Closed-loop insulin delivery systems that automatically adjust dosing based on predictive modeling.
- Digital coaching platforms that adapt behavioral nudges according to real-time biometric data.
- Virtual care pathways that integrate mental health, nutrition, and physical activity monitoring into a unified profile.
These features will completely change remote monitoring so that it can be used to build a fully coordinated care network where device data, clinical insights, and therapeutic interventions work together almost perfectly. This model allows for both scalability and personalization.
The entire RPM infrastructure can grow with the number of patients in a system, while still giving each patient access to personalized therapeutic strategies and health care solutions.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

Conclusion
API-based integration has become a key part of big diabetes solutions. It lets devices, platforms, and clinical systems work together as a single, high-performance network. Remote patient monitoring platforms can use well-designed APIs to bring together glucose sensors, insulin delivery systems, activity trackers, and apps for patients into one data fabric.
That might include systems that can handle load with continuous monitoring, weekly data feed updates, and other slow-fi cadences, but the point stands: every last individual data point should reach the correct system in the right format with a small amount of latency, whether it be from live telemetry or periodic measurements.
True acceleration comes when the world shifts from integration to device connectivity to full clinical interoperability. Platforms designed with healthcare software integration at their core can:
- Push validated patient data directly into EHRs and payer systems without manual intervention.
- Synchronize insights across telehealth portals, care management tools, and analytics engines.
- Maintain compliance with HIPAA, GDPR, and regional data governance standards while scaling.
By embedding these capabilities into the infrastructure, providers are better equipped to scale their RPM programs while maintaining high performance, security, and data integrity. It helps healthcare organizations prepare for the days when AI, predictive analytics, and personalized medicine become accepted as routine in diabetes management.
Get in touch with Jelvix—your global integration partner. We work with healthcare providers and vendors to design custom integration strategies to enable scalable, API-driven RPM networks. We know how to help make data flow better in multi-vendor environments and are experienced at connecting devices, optimizing flows of data, and shaping more technologically mature predictive care models. Reach out today to discuss your project and explore how we can accelerate your digital health transformation.
FAQ
What compliance certifications should be prioritized when launching RPM solutions for diabetes?
Key certifications include HIPAA (US), GDPR (EU), ISO 13485 (medical devices), and IEC 62304 (medical software). Developing APIs with built-in compliance features lowers regulatory risks during scaling.
What are the best practices for ensuring data security in API-enabled RPM networks?
Best practices encompass end-to-end encryption, token-based authentication, role-based access control, and routine penetration testing. For B2B implementations, security must be integrated at the API level to safeguard sensitive patient data both during storage and transmission.
How can clinics and health systems quickly scale RPM services without major infrastructure changes?
Using API-driven device integration allows healthcare providers to add new monitoring devices without needing to replace their existing EHR systems. Cloud-based data aggregation platforms facilitate scaling with minimal hardware costs.
What role do APIs play in partnering with insurance companies for RPM reimbursement?
APIs enable smooth sharing of RPM data with payers in standardized formats, simplifying compliance with reimbursement criteria for diabetes monitoring programs. This transparency fosters value-based care initiatives and enhances B2B collaborations.
Which interoperability standards are essential for connecting RPM devices in diabetes care?
Essential standards encompass HL7 and FHIR for health data exchange, IEEE 11073 for medical device communication, and DICOM for imaging data. Adhering to these standards guarantees smooth integration among devices, EHR systems, and third-party analytics platforms.
Need a qualified team of developers?
Scale your development capacity with top-level expertise and resources.