Claim processing is an integral but extremely challenging part of healthcare. Private insurers deny about 15% of all claims (even pre-approved ones) which ultimately costs almost USD 20 billion to health facilities.
If your clinic suffers from time-consuming activities like processing claims that can be denied for numerous reasons, this article is for you. You’ll find out key reasons for denying claims, ways to optimize the adjudication process, and details on choosing medical software that can help improve claim processing.
What Is Claim Adjudication in Medical Billing?
Adjudication in healthcare is the process of reviewing an insurance claim submitted by a medical facility. It involves insurance companies checking the received claims for coverage eligibility and compliance with payer policies.
Based on cases covered by a patient’s insurance and types of provided medical services, insurers decide whether to approve or decline a claim. This helps insurance companies and hospitals maintain their financial health and detect and mitigate fraudulent claim activities.
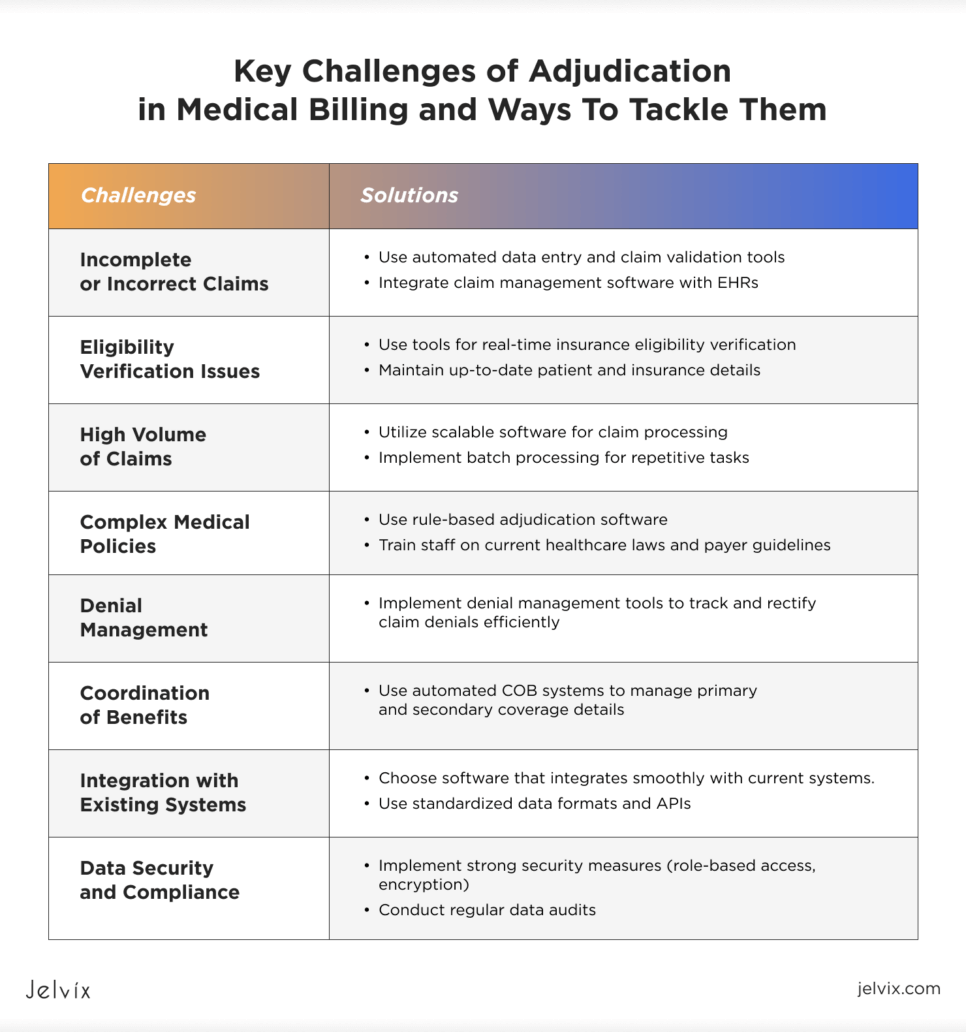
Key Challenges of Adjudication in Medical Billing and Ways To Tackle Them
Medical claim adjudication is a pretty complex process associated with numerous challenges. Clinics need to address them if they want their claim processing to be fast and accurate.
Incomplete or Incorrect Claims
Claims that contain missed or incorrect info, such as coding errors or wrong patient data, can lead to denials. Automated data entry in healthcare and claim validation tools can help tackle this issue. Another good idea is to iterate claim management software with your EHR to process claims faster.
Eligibility Verification Issues
Verifying if a patient is eligible for services can be slow and full of mistakes, causing rejected claims. To fix this, use tools that check insurance databases right away to see if a patient is eligible. Keep patient and insurance details up to date to avoid mix-ups and make sure the verification process goes smoothly.
High Volume of Claims
Dealing with a bunch of claims can stress out your team, causing delays and errors. To avoid this, use scalable software to process claims. By using batch processing to take care of repetitive tasks, you can make things easier for your team and cut down on manual work.
Complex Medical Policies
Dealing with insurance rules can be overwhelming, leading to non-compliance and claim denials. To stay updated, use rule-based adjudication software and train your staff on current healthcare laws and payer guidelines.
Denial Management
Dealing with denied claims is time-consuming. You have to figure out why they were denied, fix the errors, and then send them in again. It’s a good idea to use denial management tools to keep track of why claims are getting denied and to make the whole process easier.
Coordination of Benefits
Sorting out who pays for what is often a complicated task, especially when a patient has two or more insurance plans. Using automated coordination of benefits (COB) systems can help you check your primary and secondary coverage details and process claims more accurately.
Integration with Existing Systems
Integrating new software into existing workflows is always challenging and can lead to data silos and inefficiencies. Ensure that the software you choose can smoothly integrate with your current systems to ease data exchange. Use standardized data formats and APIs to support FHIR Interoperability and seamless integration.
Data Security and Compliance
It can be challenging to ensure the security and privacy of patient data while processing claims. What you can do is implement strong security measures, such as role-based access controls and advanced encryption protocols, and conduct regular audits to protect patient data.
Explore how FHIR standards are improving healthcare interoperability and learn about benefits and implementation strategies.
Common Reasons for Denying Medical Claims
There are numerous reasons why claims can be denied in healthcare. Clinics need to recognize these reasons to prevent denials effectively.
Missing Documentation
Claims can be denied if they lack the necessary documentation to confirm the provided services. Including all required documents with the claim can help prevent this issue.
Eligibility Issues
Sometimes claims are denied because the patient’s insurance coverage is inactive or medical services aren’t covered by their plan. Always check the patient’s insurance details before providing services.
Lack of Preauthorization or Referral
Some procedures need preauthorization or a referral from a primary care doctor. If these aren’t obtained in advance, the claim might be denied.
Medical Necessity
Insurance companies may deny claims if they think the service wasn’t medically necessary. Providing clear documentation and justification for the services can help reduce these denials.
Service Not Covered
Each insurance plan has specific services that it covers. If a claim for a service goes outside of this coverage, it will be denied.
Coding Errors
Incorrect or mismatched codes, such as CPT, ICD-10, or HCPCS, can result in claim denials. Accurate coding is critical because these codes communicate the services and their necessity to the insurance company.
Duplicate Claims
Sometimes, you can submit more than one claim for the same service by mistake or the billing system can do so because of an error. In this case, you will likely face a claim denial.
Timely Filing
Insurance companies have strict deadlines for submitting claims. Patients who submit them after the set deadlines typically face denials.
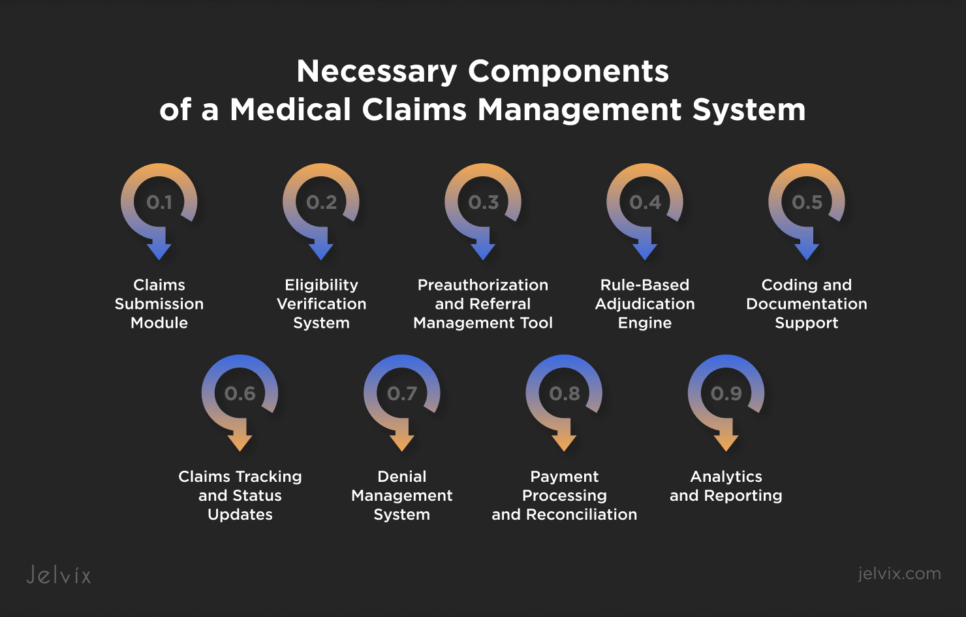
Necessary Components of a Medical Claims Management System
Although clinics face claim denials pretty often, modern tech like claims adjudication software can help prevent about 90% of them. But to do so, this software should include several key components aimed at making claim processing painless and fast.
Claims Submission Module
This component allows clinics to submit claims electronically. It ensures that all necessary information, such as patient details, service codes, and provider information, is included in the claim.
How it helps:
- Reduces paperwork and manual entry errors;
- Ensures claims are submitted on time;
- Eases the electronic transfer of claims to insurance payers.
Eligibility Verification System
This module verifies the patient’s insurance coverage in real time, ensuring that the provided services are covered under the patient’s policy.
How it helps:
- Prevents denials due to ineligible coverage;
- Saves time by automating the verification process;
- Reduces the risk of providing uncovered services.
Preauthorization and Referral Management Tool
This component tracks and manages the preauthorization and referral requirements for specific procedures or treatments.
How it helps:
- Ensures that required approvals are obtained before services are rendered;
- Reduces claim denials related to missing preauthorizations or referrals;
- Optimizes communication between providers and payers.
Rule-Based Adjudication Engine
A rule-based engine applies predefined rules and guidelines to evaluate the claims. It checks for compliance with payer policies, coding accuracy, and other important criteria.
How it helps:
- Automates the evaluation of claims against payer-specific rules;
- Identifies errors or discrepancies in claims submissions;
- Ensures consistent and accurate adjudication.
Coding and Documentation Support
This module provides support for accurate medical coding and ensures that all necessary documentation is included with the claim.
How it helps:
- Reduces coding errors that lead to claim denials;
- Ensures complete and accurate documentation is submitted;
- Supports compliance with coding standards and regulations.
Claims Tracking and Status Updates
This component tracks the status of each claim from submission to final adjudication, providing real-time updates to healthcare facilities.
How it helps:
- Enables providers to monitor the progress of their claims;
- Provides visibility into claim status and potential issues;
- Eases timely follow-up on pending or denied claims.
Denial Management System
This module identifies and categorizes denied claims, provides reasons for denials, and suggests corrective actions.
How it helps:
- Optimizes the process of addressing denied claims;
- Provides insights into common reasons for denials;
- Improves future claim submissions by identifying patterns and issues.
Payment Processing and Reconciliation
This component handles the payment process and ensures that reimbursements are correctly calculated and issued. It also reconciles payments with submitted claims.
How it helps:
- Ensures accurate and timely payments to providers;
- Simplifies the reconciliation of payments and claims;
- Reduces administrative burden and errors in payment processing.
Analytics and Reporting
This module provides detailed reports and analytics on claim performance, denial rates, and other key metrics.
How it helps:
- Provides insights into the efficiency of the claims process;
- Identifies trends and areas for improvement;
- Supports decision-making for optimizing revenue cycle management.
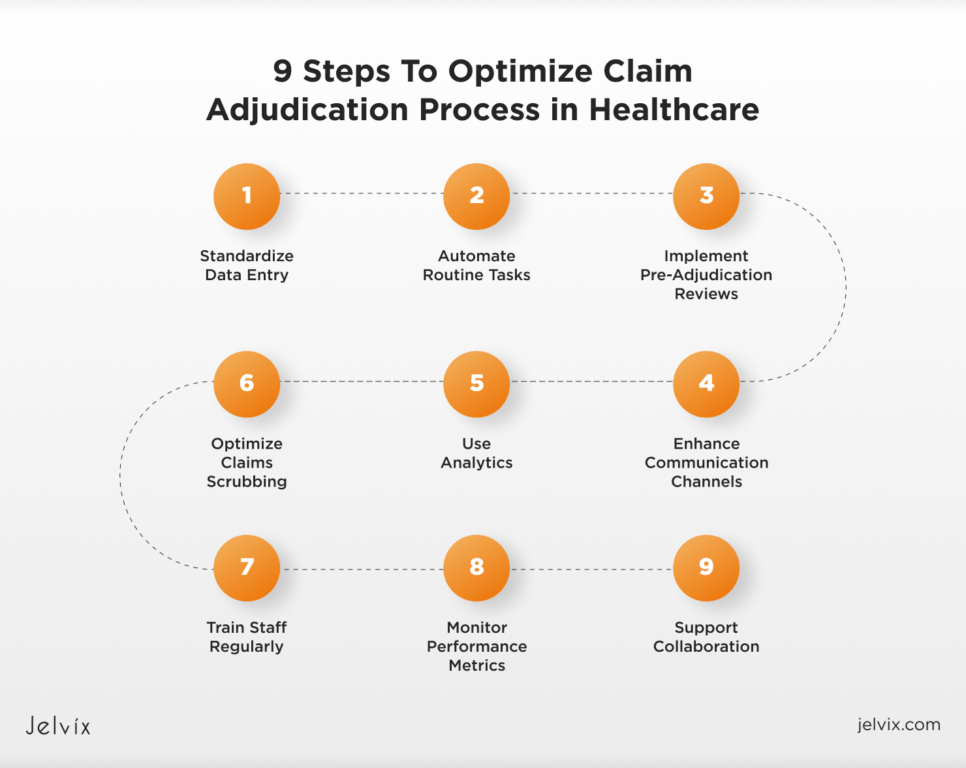
Claim Adjudication Process in Healthcare: 9 Steps To Optimize It
Companies need to optimize their claim adjudication process to make things run smoothly, reduce errors, and get reimbursements faster. The Jelvix team suggests that you follow several steps that will help you optimize claim adjudication at your clinic.
1. Standardize Data Entry
Make sure all the data entered into your system is consistent and standardized. This way, you’ll minimize errors and make it easier to process claims. Implementing standardized data formats and protocols can greatly improve data accuracy.
2. Automate Routine Tasks
Automate as many routine tasks, such as data entry, eligibility checks, and initial claim evaluations, as possible. Automation helps speed up the process and reduce the risk of human errors.
3. Implement Pre-Adjudication Reviews
Conduct pre-adjudication reviews to spot and correct errors before claims are submitted. This step can include checking for missing information, verifying coding accuracy, and ensuring all required documentation is attached.
4. Enhance Communication Channels
Improve communication channels between healthcare providers, insurance payers, and patients. When communication is clear, it’s easier to resolve issues quickly and keep everyone informed about the status of claims.
5. Use Analytics
Use predictive analytics to identify potential issues before they become problems. Predictive tools can help foresee claim denials, allowing you to take preventive measures and reduce the likelihood of rejections.
6. Optimize Claims Scrubbing
Use claims scrubbing tools to clean and validate claims before submission. These tools check for errors and inconsistencies, ensuring that claims meet payer requirements and reducing the risk of denials.
7. Train Staff Regularly
Ensure your medical teams receive proper training and are up to date with the latest coding standards, insurance policies, and regulatory requirements. Continuous education helps maintain high accuracy and efficiency.
8. Monitor Performance Metrics
Regularly track and analyze performance metrics related to the claim processing. Key metrics can include claim denial rates, processing times, and reimbursement rates. Analyzing them helps identify areas for improvement.
9. Support Collaboration
Encourage collaboration among all stakeholders involved in the process. This includes healthcare providers, billing staff, and insurance payers. Partnership can lead to better problem-solving and more efficient processing of claims.
Key Benefits of Automating Healthcare Claims Adjudication
Automating the claims adjudication process brings several benefits to healthcare providers and insurers.
Increased Efficiency and Speed
Automation speeds up claims processing by eliminating manual tasks. This allows for quicker handling of large volumes of claims, leading to faster reimbursements and more efficient operations.
Reduced Errors and Denials
Automated systems ensure accurate data entry and coding, reducing errors that lead to claim denials. This minimizes the need for reworking claims and improves the overall revenue cycle.
Cost Savings
By cutting down on manual labor and errors, automation reduces administrative costs. Faster processing also means quicker reimbursements, which improves revenue flow for healthcare entities.
Improved Compliance and Security
Automated systems comply with industry standards and regulations, reducing the risk of non-compliance penalties. They also enhance data security with robust encryption and access controls, protecting sensitive patient information.
Discover the key security risks in cloud computing and learn strategies to protect your data.
Enhanced Reporting
Automation provides detailed reports and analytics on claim performance, denial rates, and processing times. These insights help clinics optimize their claim processing and make informed decisions.
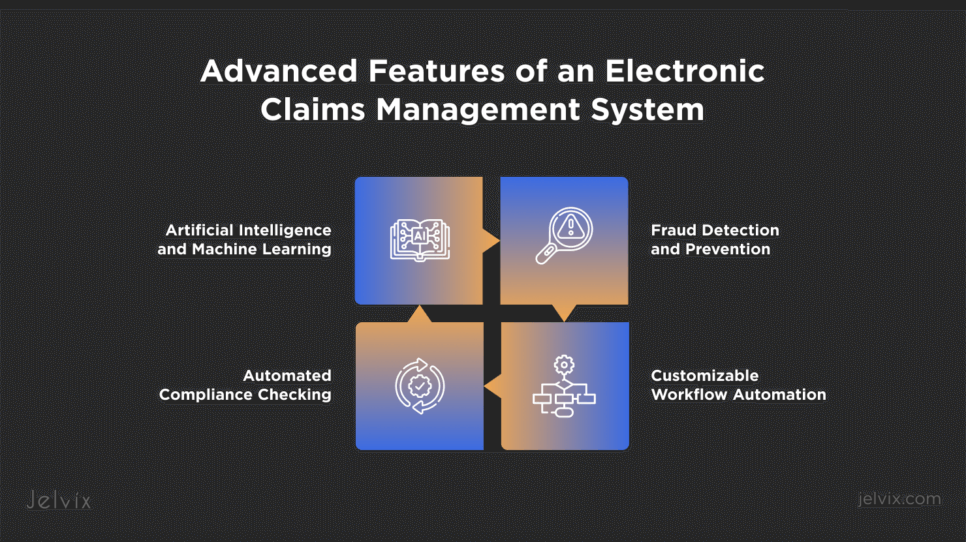
Advanced Features of an Electronic Claims Management System
Depending on your needs, medical claims adjudication software may come with a variety of advanced features that help enhance claim processing efficiency and accuracy.
Artificial Intelligence and Machine Learning
AI and ML algorithms can analyze vast amounts of data to predict claim outcomes, detect fraud, and identify patterns that indicate inconsistencies. These technologies help make informed decisions and improve the accuracy of claim adjudication.
Automated Compliance Checking
This feature ensures that all claims meet regulatory requirements and payer-specific guidelines. It helps avoid legal fines and ensures that claims are processed correctly.
Fraud Detection and Prevention
Advanced fraud detection algorithms analyze claims data to identify suspicious patterns and potential fraudulent activities. This feature helps protect healthcare providers and payers from financial losses due to fraudulent claims.
Customizable Workflow Automation
Workflow automation allows medical facilities to set up specific rules and processes for claim adjudication. This flexibility ensures that the software can adapt to the unique needs of different healthcare organizations, optimizing operations and improving efficiency.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

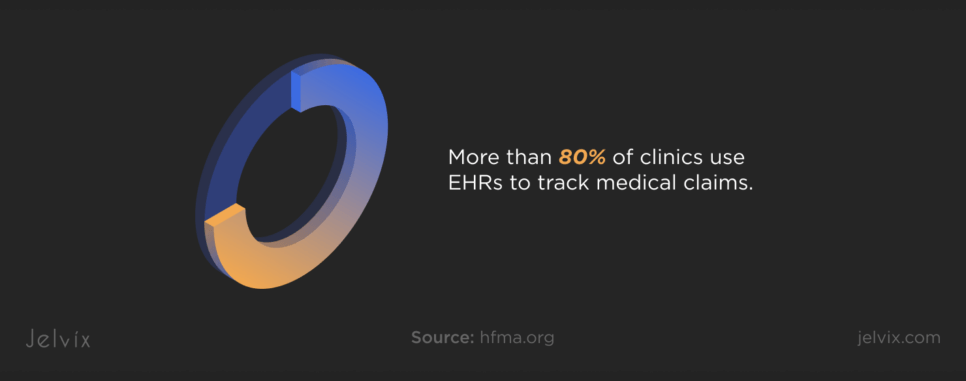
Advanced Features of EHRs for Claims Management Software
More than 80% of clinics use EHRs to track medical claims. If you’re one of them consider integrating your EHR with claim management software and upgrading it to offer advanced features for maximum efficiency.
Comprehensive Reporting and Analytics
Advanced EHR systems can offer robust reporting and analytics tools that provide insights into claim performance and revenue cycle metrics. These tools help clinics identify trends, monitor key performance indicators, and make data-driven decisions to improve claims management.
Patient Portal Integration
Integrating a patient portal with your EHR system allows patients to access their claim status, payment details, and other relevant information. This transparency improves patient satisfaction and reduces the administrative burden on healthcare teams.
Preauthorization Management
Managing preauthorizations within your EHR system can improve the approval process for services that require prior authorization. This feature ensures that necessary approvals are obtained before services are provided, reducing the risk of claim denials.
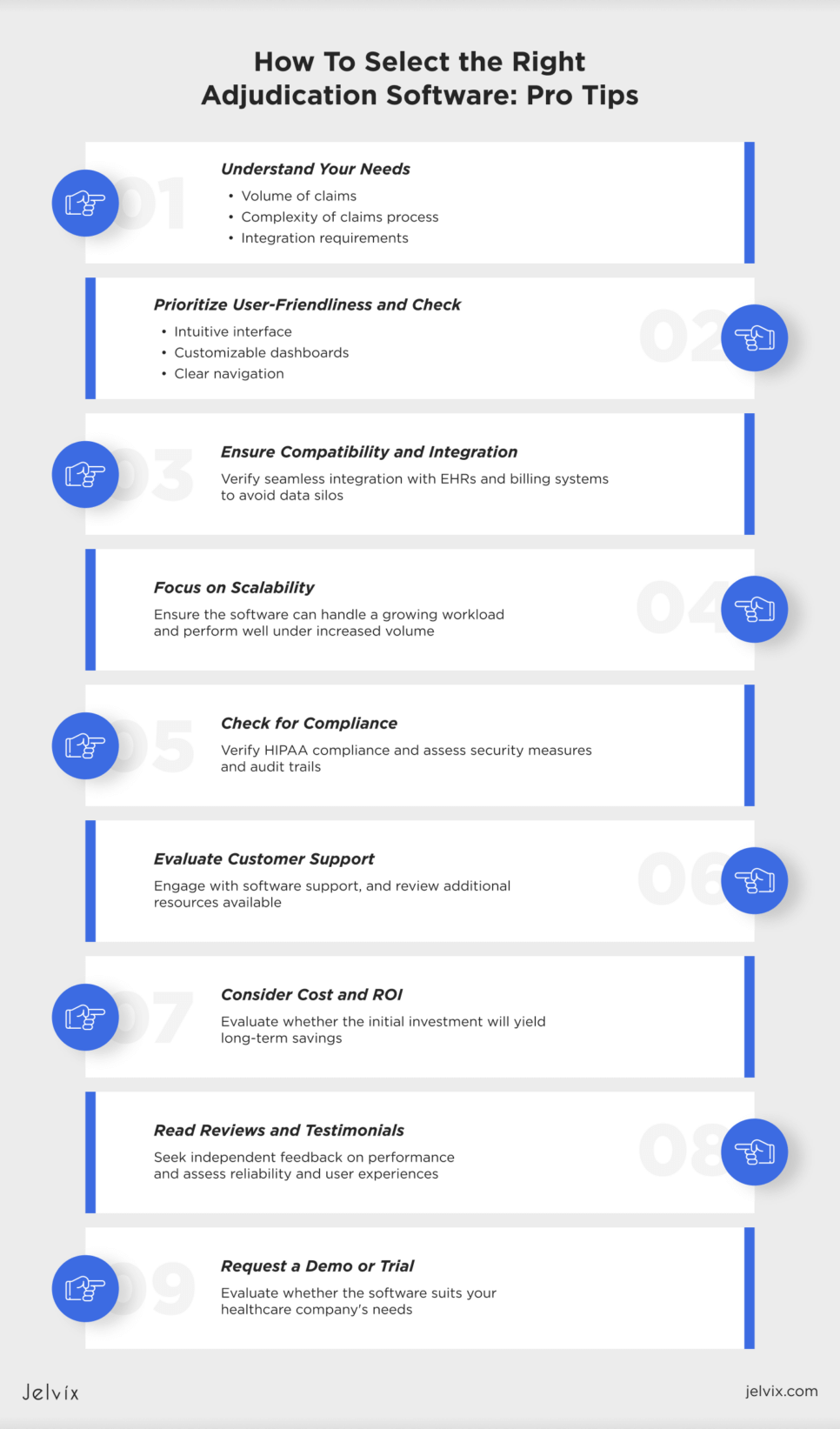
How To Select the Right Adjudication Software: Pro Tips
Choosing the right adjudication software can help optimize the claims process, reduce errors, and ensure timely reimbursements. Consider following the tips listed below to choose the software that best suits your business goals.
Understand Your Needs
Before you start looking at different software options, understand your specific needs. Consider the volume of claims you handle, the complexity of your claims process, and the specific features you need (e.g., integration with existing systems, real-time data processing, and comprehensive reporting tools).
Prioritize User-Friendliness
The software should have an intuitive interface and be easy for your staff to use. User-friendly systems reduce the learning curve and minimize errors during claims processing. Look for solutions that offer customizable dashboards, easy navigation, and clear instructions.
Ensure Compatibility and Integration
Make sure the adjudication software can seamlessly integrate with your existing systems, such as EHRs, practice management software, and billing systems. Compatibility and integration are critical for maintaining a smooth workflow and avoiding data silos.
Focus on Scalability
Choose software that can grow with your hospital. As your practice expands and the volume of claims increases, the software should be able to handle the additional workload without compromising performance.
Check for Compliance
Ensure the software complies with all relevant healthcare regulations like HIPAA. Compliance features are vital for protecting patient data and avoiding legal issues. The software should include robust security measures, regular updates, and audit trails.
Evaluate Customer Support
Good customer support is essential for resolving issues quickly and efficiently. Make sure your vendor offers assistance options, such as email responses or live chat support. Also, check for additional resources like user manuals, tutorials, and community forums.
Consider Cost and ROI
While cost is a significant factor, it shouldn’t be the only consideration. Evaluate the return on investment the software offers by improving efficiency, reducing errors, and speeding up the claims process. A bigger investment at the beginning can lead to greater savings in the long run.
Read Reviews and Testimonials
Check reviews and testimonials from other clinics that have used the software. Their experiences can provide insights into the software’s performance and reliability. Look for reviews on independent platforms to get an unbiased perspective.
Request a Demo or Trial
Before making a final decision, request a demo or trial of the software. This allows you to test the features, assess usability, and determine if it meets your needs. A hands-on experience is the best way to ensure the software is a good fit for your medical company.
How Custom Adjudication Software Can Improve Your Claims Processing
Sometimes, the solutions offered on the market may not completely suit your current needs and future goals. In this case, opting for a custom claim processing software can be a good idea.
If you need help developing tailored claims adjudication software for your clinic, the Jelvix team can help. As a seasoned software development partner, we can create a system that will help you manage the needed volume of claims efficiently and accurately. Reach out to our specialists for a consultation based on your business needs.
Looking for a skilled team?
Boost your development capacity with our dedicated professionals.