The global market for digital rehab is clearly on the rise. According to Grand View Research, it is expected to grow from USD 16.96 billion in 2024 to USD 27.29 billion by 2030, with a CAGR of 8.3%. This is closely tied to demographic factors, especially the aging population, and the rising number of people with chronic diseases, including stroke, arthritis, and heart disease.
Not only is technology changing how treatment is given, but it also affects the outcomes. Telerehabilitation is becoming a key part of post-acute care plans all around the world. This includes robotic-assisted exoskeletons and AI-enhanced wearable sensors. Penumbra’s full-body VR rehabilitation suite and Hyundai’s “X-ble MEX” wearable robot show that virtual rehabilitation is a real thing that can be employed by more and more people because it’s so easy to use.
These changes are not unique; they are part of a broader trend toward decentralizing rehabilitation and bringing therapy into homes and communities, particularly in areas with inadequate physical infrastructure.
This article goes into great detail about the technology that will change rehabilitation in 2025-2026. We’ll start by looking at the main new technologies that are making this change happen, such as rehabilitation software, robotics, and AI-powered tools.
Then we’ll look at how these technologies are being used in both inpatient and outpatient settings. This guide offers an in-depth look at where rehab technology is headed—and how to prepare for what’s next.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

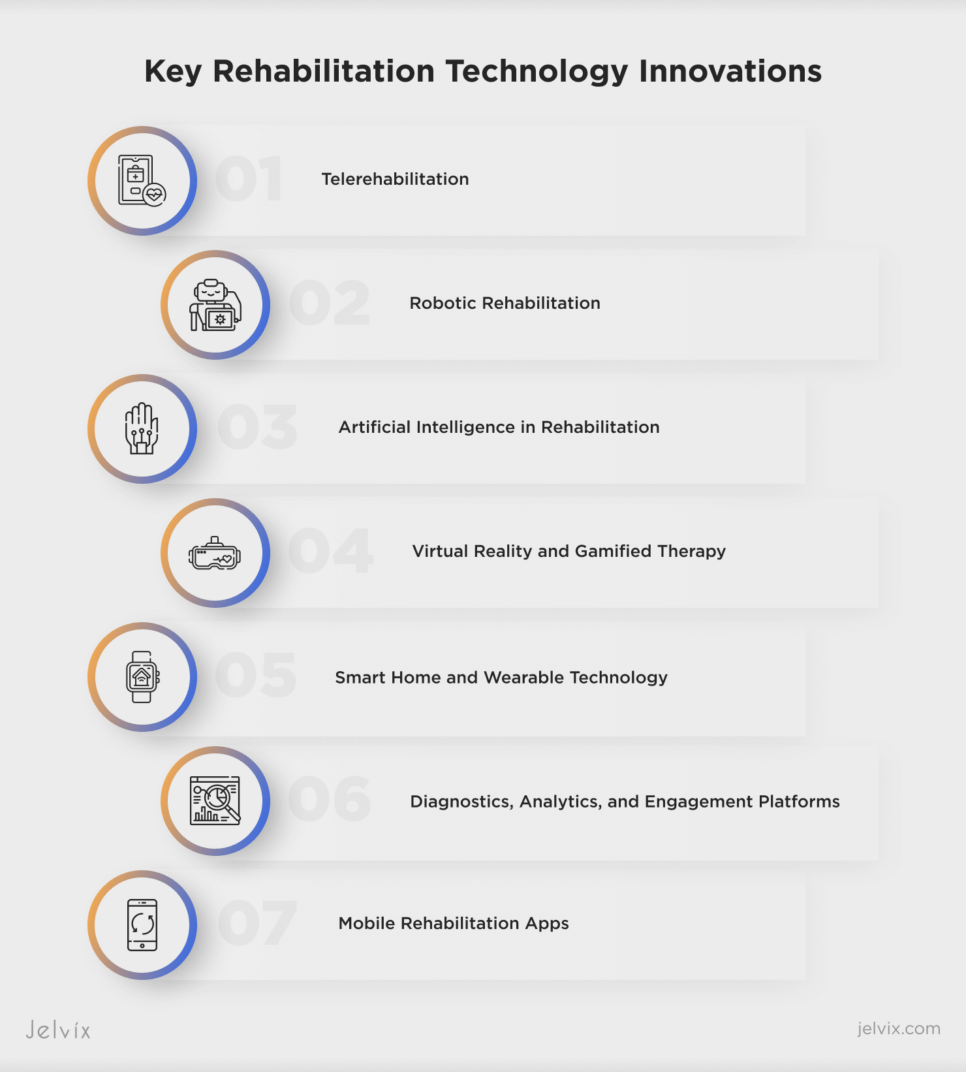
Rehabilitation Technology: Core Innovations
In 2025, rehabilitation technology will be defined by seamless integration, smart automation, and clinical accuracy. The field is moving away from fragmented tools and toward systems that work together to provide care that is always adapting.
In 2025, physical therapy uses AI not only to speed things up but also to provide care that is more precise and thorough. Therapists can use motion analysis software that employs deep learning to compare a patient’s movements to large clinical datasets.
This lets them make exercise plans that reduce the risk and accelerate their progress. These algorithms can now make changes in real time during a session, spot patterns that show strain before symptoms reveal themselves, and give outcome forecasts based on each patient’s biometrics.
Documentation, which used to take a lot of time, has also been transformed. AI-enabled ambient systems automatically record clinical conversations, turning therapist observations and verbal signals into arranged notes. This cuts down on manual entry by almost half, makes it easier to follow the regulations, and lets clinicians focus completely on their patients.
Immersive technologies are currently the second pillar of sophisticated rehab tech, next to AI. Virtual reality creates adaptive environments that change the level of difficulty depending on how well a patient is doing. This establishes a dynamic, engaging feedback loop that encourages consistency and motivation.
Augmented reality places a layer of instructional help directly in the patient’s physical area, providing real-time corrections and visualizations that assist them in learning and improving their motor skills.
It’s evident that these platforms do more than just entertain; they also collect extensive movement data, quantify improvement with clinical accuracy, and make therapy more accessible without decreasing quality. They are changing not only how treatment is given but also how progress is measured.
The Rise of Telerehabilitation
Telerehabilitation has gone from being a temporary fix for emergencies to a long-term clinical solution. It involves offering rehabilitation services from a distance, utilizing telecommunications technology. This can include physiotherapy, occupational therapy, and cognitive care, among other fields.
It supports full-spectrum care, such as evaluation, monitoring, guided intervention, and reporting on outcomes. In practice, telerehab connects professionals to patients who are far away, removing geographic barriers and keeping care going.
The technology is already performing duties. Telerehabilitation can be just as beneficial as in-person therapy, especially for musculoskeletal, cardiovascular, and neurological problems, according to randomized clinical research. After arthroplasty, during stroke recovery, and for shoulder rehabilitation, it has been utilized successfully with measurable improvements in motion, strength, and patient-reported satisfaction.
Physiotherapists may now change programs without being physically close thanks to video calls, interactive home exercise platforms, and sensor-based telemonitoring. The World Federation of Occupational Therapists backs telerehab as an acceptable method when in-person care isn’t possible or isn’t as effective.
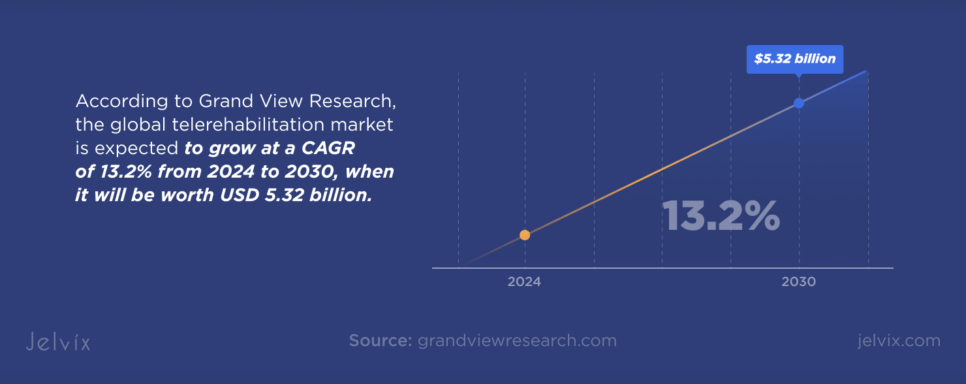
This change is shown by the rise of the market. According to Grand View Research, the global telerehabilitation market is expected to grow at a CAGR of 13.2% from 2024 to 2030, when it will be worth USD 5.32 billion. The increase is due to the growing number of people with chronic and neurological conditions, especially children and the elderly.
It is also due to the fact that there are now more use cases, such as behavioral health, pain management, and follow-up monitoring. Clinical therapy is still the most popular service area, but there is a growing need for integrated platforms that offer virtual consultations and remote progress tracking. These systems also use AI development to automate tests, make diagnoses more accurate, and customize therapy plans for a lot of people.
Challenges of Telerehab
But there are still certain challenges with adoption. Full-scale integration is still held back by a lack of ICT skills, an absence of clarity about reimbursement, and insufficient infrastructure. Technical problems, including software fragmentation, weak security standards, or non-interoperable platforms, might also make clinical utility go down. But it’s evident that the long-term value is there.
Telerehab makes scheduling easier, helps people stick to their plans by giving them real-time feedback, and reaches out to those who don’t get enough services. It helps physiotherapists and health organizations. When combined with innovative rehab software and robotic rehabilitation instruments, it is the foundation of modern, distributed care.
Robotic Rehabilitation: Expanding the Boundaries
Robotic rehabilitation therapy uses smart, motorized gadgets to help or guide patients as they move during therapy sessions. These devices can mimic complicated motor patterns, change resistance based on feedback in real time, and keep track of development with clinical accuracy. Robotic systems are different from passive tools because they are dynamic.
Rehabilitation robotics is based on a wide range of systems that are made to meet unique demands. For example, exoskeletons are robots that you can wear that help you walk, move your arms and legs, and keep your joints stable. Active models like Ekso Bionics and HAL can pick up neural signals and turn them into supported motion. This makes them good at helping paralyzed limbs move again.
Passive solutions like NEUROExos and WREX can help with load balancing and joint alignment without requiring power to work. In upper limb therapy, gadgets like ARMin and IntelliArm enable therapists to make exact modifications to their treatments by guiding complicated joint movements and keeping track of performance data.
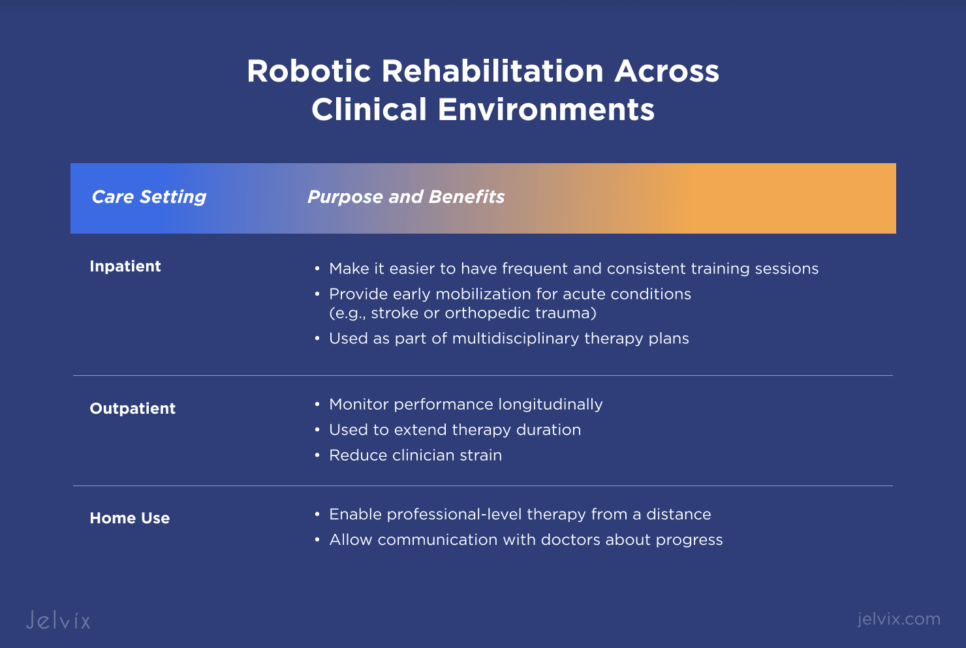
Robotic rehabilitation devices are often used in multidisciplinary therapy plans for patients who are staying in a hospital. They provide early mobilization for acute conditions such as stroke or orthopedic trauma. These technologies make it easier to have training sessions that happen often and don’t change much, which is important for getting back to baseline function.
Outpatient clinics, on the other hand, are using robotic tools to extend therapy duration, reduce clinician strain, and monitor performance longitudinally. Robotic solutions that can be used at home are starting to work with telerehabilitation platforms. This lets patients get professional-level therapy from a distance while still being able to talk to their doctors about their progress.
Real-world research backs up the clinical benefits of robotic rehabilitation. Patients who have had a stroke and are getting robot-assisted therapy see big improvements in their upper limb mobility and their ability to get back to normal movement patterns. Lower limb exoskeletons have made it easier for people with spinal cord injuries to walk, reducing their dependence on caregivers.
Clinical trials have shown that robotic therapy often works just as well as or better than traditional methods, especially when combined with AI-driven progress tracking and individualized programming. The real strength of these systems is not just that they can automate movement, but also that they can make human-led care more successful, making therapy more accurate, scalable, and measurable.
Artificial Intelligence in Rehabilitation
AI is changing rehabilitation by adding a level of flexibility and foresight that wasn’t feasible before. AI systems don’t only follow set therapeutic plans or subjective observations. They learn directly from how each patient moves, reacts, and progresses.
They use data from prior instances and current situations to change exercises in real time, gently noticing delays, symptoms of weariness, or strange movement patterns that would have gone unreported otherwise.
These days, smart rehab software seems more like a helpful partner than a way to keep track of things. The software makes a digital mirror of the patient’s progress using wearable sensors or camera-based motion tracking. It records every small change and adjustment, figures out the underlying metrics, and makes adjustments without stopping the therapy.
That kind of quiet accuracy implies greater feedback for both the patient and the physician, and it also cuts down on the time wasted on methods that don’t work.
The ability to predict is what makes AI unique. The algorithm can guess what will happen next based on how the patient reacts in the first few weeks. It can tell who is likely to plateau, who would do better with robotics, and who needs a change before progress stops. This spares doctors from having to try things out and lets them make better, quicker decisions without burning out.
Virtual Reality and Gamified Therapy
Virtual reality is no longer a new thing in rehab; it’s a toolset that is influencing how patients interact with therapy itself. Patients no longer do the same exercises over and over again in sterile clinical settings. Instead, they join immersive, task-based worlds that mimic actual challenges or abstract environments that help them get better.
These VR systems make rehab more personal through modifying the intensity and difficulty of the exercises based on each patient’s present skills and performance metrics. They do this through motion capture, real-time feedback, and adaptable difficulty.
More and more hospitals and outpatient clinics are using virtual therapy modules that work with their current rehabilitation software platforms. These aren’t just game consoles that seem like treatment; they’re FDA-approved devices that have been set up to boost therapeutic outcomes.
For example, stroke survivors who use virtual reality rehabilitation systems to retrain their limbs generally have increased cortical activation compared to those who go through traditional rehab.
You can see the results in fMRI data and kinematic telemetry. Patients with issues with balance do dynamic weight-shifting exercises in simulated urban landscapes. People who are recovering from orthopedic surgery learn fine motor skills again through virtual reality physical therapy activities that are based on goals and test their range, dexterity, and reaction time.
The benefits get better over time. Patients say they feel more involved and less self-conscious. Therapists keep track of progress by using session-based statistics to compare joint angles, motion smoothness, and completion times on easy-to-use dashboards.
Virtual reality for rehabilitation gives a significant number of situations to work with, including crossing virtual bridges, reaching for groceries, or moving around familiar home spaces. These scenarios make people move more naturally and think more deeply. These qualities make it one of the most influential physical therapy trends currently redefining the field.
Some systems now combine immersive therapy with telerehab, which lets patients do supervised sessions from home using headsets and motion-tracking technology. When corporations look into this new area, they often partner with AR/VR development companies to create or modify solutions that fit with their existing processes.
Smart Home and Wearable Technology
Wearable IoT is quietly transforming the landscape of physical therapy with the precision of continuous insight. In today’s rehab environments, these devices become data-rich companions that record, interpret, and transmit a patient’s every action. As outpatient rehab software evolves, these wearables sync effortlessly with digital systems, creating a feedback loop that supports clinicians while empowering patients.
Sensors built into wristbands, shoes, or clothing can detect minute shifts in movement or vitals. It’s no longer theory—an off-kilter gait post-hip surgery now triggers real-time feedback; a spike in temperature during home therapy prompts infection alerts. With each repetition, biomechanical monitors capture joint mechanics, muscle activation, and endurance patterns, then deliver those metrics straight to a provider’s dashboard.
Meanwhile, smart textiles make the process feel less clinical. Shirts and leggings embedded with micro-sensors collect mobility data while offering comfort and familiarity. For someone navigating recovery from a spinal injury or Parkinson’s diagnosis, the ability to move freely while generating data that shapes tomorrow’s therapy is crucial. These garments offer precision without restriction and real-time coaching without constant intervention.
At-Home Rehab Monitoring Through IoT
Back at home, IoT’s impact doesn’t taper off. Bluetooth-enabled spirometers, pulse oximeters, and motion sensors turn everyday spaces into responsive rehab zones. Subtle changes in movement or respiratory function trigger alerts, while AI-driven platforms offer reminders or adjustments tailored to that moment’s context.
These capabilities represent current trends in physical therapy that prioritize adaptability and transparency. Patients no longer have to guess whether they’re improving. Real-time visualizations make the invisible visible: progress charts, movement symmetry diagrams, cardio trends over weeks.
As clinics look ahead, the horizon is filled with rehabilitation software that listens, learns, and evolves. From smart floors that detect fall risk to digital twins that simulate recovery paths, new technology in physical therapy is about removing barriers—geographical, cognitive, and emotional.
It’s about giving patients agency and giving therapists better tools to guide recovery. Jelvix, through its custom solutions like the Physical Therapy Exercise App, is at the center of that change, helping rehab providers build connected ecosystems that feel personal and perform like clockwork.
Diagnostics, Analytics, and Engagement Platforms
Today’s rehabilitation environments rely on more than patient observation—they run on real-time diagnostics and intelligent analytics. Clinics are adopting motion capture systems and EMG (electromyography) sensors that map muscle activation across therapy sessions. These tools offer a more granular view of performance than visual assessments alone.
For example, small improvements in coordination after stroke therapy, previously imperceptible, can now be identified by comparing 3D motion data across sessions.
Layered on top is business intelligence that turns this raw data into a clinical advantage. Rehab centers now employ AI-powered dashboards that aggregate outcomes across patient groups, revealing which protocols yield faster recovery, lower readmission, or higher patient compliance.
This type of analytics supports individual care and informs institutional strategy. Decisions on staffing, equipment allocation, and treatment pathways are now grounded in real performance metrics, rather than assumptions.
Diagnostic imaging is also gaining contextual intelligence. Integrated software can now link MRI and ultrasound results to rehab planning tools. By embedding these diagnostics into the workflow, rehab teams reduce the lag between test results and treatment changes, keeping care proactive, not reactive.
Meanwhile, digital engagement platforms add another layer of value. Daily prompts are adjusted based on biometric data. Motivational messages, progress charts, and goal suggestions adapt to each user’s therapy journey. As these platforms sync with wearable devices and outpatient rehabilitation software, they create a loop that keeps the patient informed and emotionally invested in their recovery.
Mobile Rehabilitation Apps
Rehab mobile apps are transforming therapy into a personal and accessible experience. No more messy printouts or uncertainty—patients can follow guided workouts, receive real-time feedback, and enjoy daily check-ins right from their phones. Features like AI motion tracking and haptic feedback help keep them motivated without the need to visit a clinic.
Clinics are embracing these innovative tools to keep track of progress from afar. The data automatically syncs with outpatient rehab software, enabling therapists to customize routines based on real movement data.
These apps cater to a wide range of needs, from neuro rehab and orthopedic recovery to gait analysis and breathing exercises. The most effective ones support post-acute interoperability and promote continuity of care after patients leave the facility. As physical therapy continues to evolve in the digital age, these applications are paving the way for a future where therapy is not just effective, but also personalized and always within reach.
Take a closer look at the process behind building a physical therapy app that supports recovery at home.
Implementing New Technologies in Your Practice
Rolling out new technology in your rehab practice isn’t just about booking one solution—it’s about upgrading your workflow. Start with the basics:
- Define your goals.
- Map your existing systems.
- Run a pilot.
Whether it’s AI-driven analytics or VR rehab modules, implementation only sticks if it solves real pain points.
Choosing Between Custom vs. Off-the-Shelf Solutions
From off-the-shelf tools to custom builds, the right setup depends on how unique your workflows are and how deep the integration needs to go. Off-the-shelf software is quicker to deploy and cost-effective, but it often means adjusting your workflows to fit the software, not the other way around.
On the flip side, custom-built platforms give you full control over functionality, branding, and user experience, which is critical if you’re running complex rehab protocols or managing unique data flows. Deep integration matters here—if your EMR, EHR, scheduling, billing, and rehab software don’t sync smoothly, you’ll lose time, data accuracy, and potentially patient engagement.
Bottom line: if your workflows are straightforward and budget is tight, go off-the-shelf. If you’re building for scale or aiming for a competitive edge, go custom and integrate smart.
But it’s not all plug-and-play. Challenges pop up—data privacy, training gaps, and compliance risks need attention up front. Don’t forget about the ethics: who owns the data, who gets access, and how do you ensure the tech helps rather than replaces the human touch? Smooth onboarding means thinking beyond features: transparency, patient trust, and clinician buy-in.
That’s where smart partnerships come in. A solid healthcare software development team will help you future-proof the tech stack, streamline interoperability, and keep you agile as regulations shift. Choose vendors who speak your language—whether that’s HL7, FHIR, or just fast support when something breaks. Integration isn’t a one-time job. It’s the foundation for scale, reliability, and long-term wins.
Learn how we built a real-time risk assessment and Shadow AI control solution for rehabilitation center.
Conclusion
Rehab software today encompasses more than just the digitization of old workflows; it embodies the development of flexible platforms that are prepared for sensor integration and capable of supporting hybrid care. These systems facilitate real-time motion tracking and encourage patient-driven recovery processes.
To remain competitive in the future, clinics must move beyond merely adopting apps and dashboards. It is essential to ensure seamless device synchronization and achieve compatibility with Electronic Health Records (EHR). Moreover, the importance of creating intelligent data layers that can adjust therapy dynamically cannot be overstated.
This is precisely where Jelvix excels; we focus on co-building systems that are specifically tailored to meet the unique requirements of your specialty and seamlessly integrate with your current tech stack, thus enhancing your rehab services to meet the demands of the next generation of digital care. So, let’s have a chat.
FAQ
How secure is rehab software in terms of patient data and compliance?
Rehabilitation software is essential for keeping patient information safe and must follow strict laws like HIPAA and GDPR, as well as local regulations. At Jelvix, we focus on security by creating systems designed with safety in mind. This includes using encryption, controlling access, and performing regular audits to keep patient data protected.
How do we ensure clinical staff adoption of new digital rehab tools?
To successfully adopt new systems, we need to make the design easy to use and offer proper training. It’s important to involve clinical stakeholders from the start. By focusing on the needs of users, we want to create tools that are both useful and welcomed by our staff.
Can digital rehab platforms be scaled across multiple locations?
Modular platforms help improve operations at different sites. They provide a consistent experience for users and ensure data is managed the same way everywhere. This smooth connection between locations supports business growth and allows companies to expand without interrupting current operations.
How customizable are rehab technology solutions?
Rehab platforms can be tailored to fit specific workflows, clinical protocols, and reporting needs. At Jelvix, we focus on creating customizable interfaces and integrations that match your unique care model. Our approach ensures that the technology integrates smoothly with your operations and improves the quality of care you deliver.
What is the ROI of investing in digital rehabilitation technologies?
Digital rehabilitation tools usually pay off within 12 to 18 months by improving therapist efficiency, making scheduling more accurate, and enabling remote services. They also create new ways to earn money by helping keep patients and allowing for more growth in operations.
Need a qualified team of developers?
Reach top talent pool to handle end-to-end delivery of your project.