Healthcare is drowning in tech noise — too many disconnected apps, too many integrations, too much architectural debt. As digital tools multiply, most organizations now struggle with healthcare integration, broken data flows, and fragmented systems that were never designed to scale. What should enable clinicians instead slows them down. The problem isn’t innovation, but the absence of sustainable interoperability in healthcare.
Real-world evidence shows how quickly this fragmentation collapses. In our diabetes app failure study, even well-funded products failed to scale because their healthcare data integration relied on brittle, point-to-point connectors that degraded over time. Onboarding new devices, EHRs, or pharmacies required rewriting entire workflows, creating architectural debt that blocked growth and compromised patient safety.
These failures reveal a structural truth: point solutions do not survive at scale. They collapse under real load, introduce compliance risk, slow product delivery, and make AI software development nearly impossible. Without unified health system interoperability, every downstream workflow becomes unpredictable.
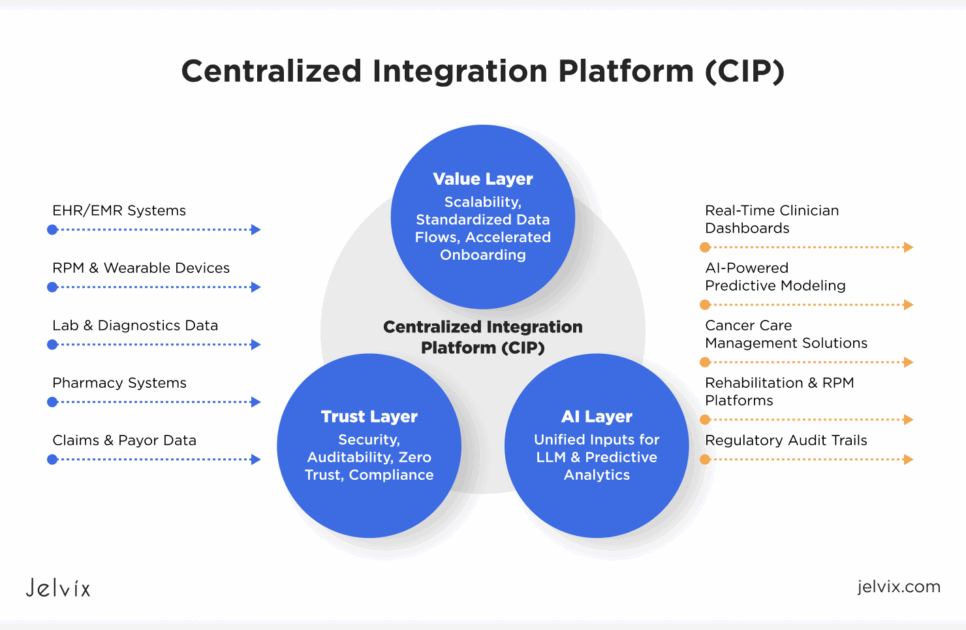
The Strategic Shift for 2026: Centralized Integration Platforms (CIP)
In 2026, leadership in digital health will belong to organizations that make a decisive architectural shift, from isolated integrations to a Centralized Integration Platform.
A CIP becomes the operating system for HealthTech, unifying trust, standardizing data flows, powering real-time connectivity, and creating the foundation needed for ethical AI and analytics. CIP consolidates:
- Trust — security, auditability, compliance, Zero Trust
- Value — scalability, event-driven data, accelerated onboarding
- AI enablement — unified inputs for predictive, prescriptive, and LLM-driven systems
This is no longer optional. Every major digital-health business model, from RPM and cancer care management solutions to rehabilitation platforms and payor-provider analytics, depends on the ability to integrate reliably and scale predictably.
Dealing with rising diabetes risks and delayed interventions? Explore how RPM transforms care with real-time tracking, timely alerts, and improved patient engagement.
Over the past year, we executed large-scale integration projects in cancer care, RPM, rehab, and hypertension management. In this research, we aim to demonstrate how a CIP can transform fragmented ecosystems into interoperable, compliant, and AI-ready platforms.
TRUST in Healthcare Integration Is Built Through Security and Compliance
As healthcare organizations expand their digital ecosystems, trust becomes the defining requirement of modern healthcare integration. Security, compliance, identity, auditability, and data lineage must all be engineered into the platform. Much of today’s risk comes from legacy point-to-point integration patterns, where each new connection increases complexity and vulnerability. A CIP reverses this trend by embedding trust into the core of the architecture.
Zero Trust Architecture: Mandatory Security for Distributed MedTech Systems
Traditional perimeter-based security was never designed for RPM devices, distributed sensors, or multi-cloud environments. As soon as data moves beyond the hospital firewall, the old model fails. RPM ecosystems, diabetes management software, and hypertension kits all operate outside controlled environments, which is why zero trust healthcare has become the industry’s new security baseline.
Zero trust model ensures that every device, user, and API request is continuously authenticated and authorized. This is essential when working with diverse ecosystems such as RPM solutions, where hardware and software vendors change frequently, and risk exposure increases with every connection.
Industry research shows the same pattern: distributed medical device networks require identity-first verification, encrypted communication, and continuous trust evaluation.
Our integration architectures use OAuth 2.0, OpenID Connect, and token-based access control to secure every interaction across the clinical ecosystem.
In a CIP, Zero Trust is the foundation. That’s why we extend the security perimeter with two-factor and multi-factor authentication, apply federated identity through SSO (using standards such as SAML for secure authentication), and enable SMART on FHIR–based app authorization so applications inside the health system follow the same identity-first rules as external partners. Together, these controls ensure that every request is verified, contextual, and compliant with modern security expectations.
Auditability and Data Lineage Are Essential for Safe Healthcare Integration
Regulators now expect complete traceability of PHI across every system involved in healthcare architecture. ONC, TEFCA, and FDA SaMD guidance all require organizations to prove how data moves, who accessed it, and how downstream workflows are informed by it.
This is nearly impossible with fragmented integrations. When logs are spread across outdated connectors or custom scripts, compliance teams cannot reconstruct the full picture. Many EHR integration challenges stem from exactly this problem: inconsistent data flows, non-standard logs, and untraceable PHI transformations.
In cancer platforms, RPM ecosystems, and rehab apps, the lack of end-to-end lineage creates patient safety risk and exposes organizations to legal liability.
Compliance in Healthcare Integration Must Be Engineered, Not Applied Later
Compliance can no longer be treated as a post-launch checklist. HIPAA and GDPR penalties for incorrect PHI handling continue to rise, and several diabetes app and RPM vendors have already faced public scrutiny due to inconsistent data flows and inadequate governance.
Real-world failures, from non-compliant RPM pipelines to misconfigured hypertension solutions, demonstrate that compliance-by-documentation is not enough. Compliance must be a structural property of the integration platform.
A CIP achieves this by enforcing standardized data flows, secure authentication, and consistent schema governance across devices, EHRs, and third-party tools. This also minimizes data fragmentation, one of the most significant risk factors in clinical systems.
We design integration platforms where compliance is built directly into the architecture. Instead of relying on after-the-fact checks, we implement HIPAA- and GDPR-aligned controls at every layer of the system. This includes role- and policy-based access to ensure that only authorized users interact with PHI, automated redaction pipelines that consistently remove or mask sensitive fields, and strict schema governance that keeps data structures stable across all vendors and devices.
Value Now Lies in Healthcare API Integration as the Driver of Efficiency
Healthcare organizations cannot scale on fragmented systems. Efficiency now depends not on adding more tools, but on integrating them through a unified, reliable architecture. A CIP turns integration from a bottleneck into a growth engine, enabling faster onboarding, stable data flows, and a foundation strong enough to support AI.
FHIR-First Architecture Replaces Point-to-Point Integration at Scale
For years, digital health platforms tried to scale by stitching together point-to-point integration patterns — one connector for each EHR, one connector for each device, one connector for each external API. This worked when a startup needed two or three integrations. It collapses when an organization needs twenty. And it becomes unmanageable when it needs hundreds. Each new connector increases cost, latency, risk, and operational overhead. Worse, point-to-point systems amplify data fragmentation because every connection transforms data slightly differently, leading to inconsistencies that clinicians immediately feel.
This is why modern digital health platforms are abandoning ad-hoc connectors and moving toward FHIR API architecture – a standardized, reusable, schema-driven approach that eliminates the need to rebuild integrations from scratch. With FHIR as the canonical model, new systems plug into a shared structure rather than into each other, greatly reducing complexity and enabling scalable healthcare data integration.
In our recent hypertension project, the team unified multiple devices, EHRs, and analytical tools through a centralized FHIR layer, enabling real-time, bi-directional clinical data flow without sacrificing compliance. By replacing dozens of inconsistent workflows with one interoperable pipeline, the platform could onboard new partners in days, not months. That is a critical competitive advantage in hypertension solutions, RPM ecosystems, and chronic care management software.
Our custom FHIR integration and HL7–based connectors enabled secure bi-directional sync between devices, EHRs, and analytics. Instead of writing custom mappings for each integration, we create a unified clinical model that every system uses as its source of truth. This reduces redundancy, prevents version drift, and ensures reliable bi-directional synchronization at scale. By adopting a FHIR-first approach, our clients eliminate the architectural limitations of legacy integrations and gain a platform foundation that can support growth, regulatory readiness, and advanced AI workflows.
Reusable Integration Frameworks Are Now a Core Competitive Advantage
In a market where digital health companies must integrate with dozens of EHRs, devices, pharmacies, labs, payors, and third-party vendors, onboarding speed has become a key competitive differentiator. It no longer matters how advanced a product is if connecting it to real clinical environments takes six months. In RPM tools, rehabilitation platforms, and cancer care management solutions, delayed integrations directly translate into lost contracts and stalled growth.
This is where reusable integration frameworks outperform traditional connector-based approaches. Instead of building each connection repeatedly (a common cause of EHR integration challenges), a CIP defines standard pipelines for identity, authorization, data normalization, validation, event handling, and error management. Every new vendor, device, or health system plugs into the same modular framework, dramatically reducing engineering effort and eliminating the maintenance burden of one-off custom integrations.
The result is not only faster onboarding but also predictable scaling. Multi-vendor ecosystems typically break because each partner introduces a new schema, transport method, or data quality issue. Without a centralized framework, these variations accumulate into a fragile web of adapters and transformations. With a CIP, however, every integration, whether for rehab solutions, RPM devices, or hypertension management software monitoring apps, follows consistent architectural rules. This creates a stable environment in which systems interoperate reliably rather than competing for control of the data flow.
In practice, organizations that adopt reusable frameworks can expand their networks exponentially faster than those that rely on point-to-point approaches. They become easier partners for hospitals, more attractive to investors, and significantly more resilient in real-world clinical deployments.
Event-Driven Infrastructure Powers Real-Time Clinical Care
Chronic-care management now depends on real-time data, not delayed uploads. Conditions like hypertension, diabetes, oncology, and post-acute rehabilitation require immediate visibility into what is happening with the patient at any moment. A blood-pressure spike, a critical lab value, or a sudden symptom change cannot wait for the next batch file to process. When updates arrive hours late, clinical windows close, risk increases, and workflows become reactive instead of proactive.
This is why batch-based healthcare architecture is becoming obsolete. In ecosystems built around RPM devices, continuous vitals, streaming wearables, and dynamic EHR updates, batch uploads create blind spots that undermine both safety and clinician trust. For organizations deploying large-scale RPM solutions or advanced hypertension solutions, these blind spots translate into missed alerts, delayed interventions, and reduced effectiveness of care models.
A Centralized Integration Platform replaces these fragile workflows with event-driven architecture — systems that listen for clinical events as they happen and trigger downstream actions automatically. Each incoming measurement, medication update, or EHR change becomes an event that can generate:
- real-time alerts to clinical teams,
- updated predictive-risk scores,
- automated care pathways,
- or enriched patient context for LLM-driven summaries.
This is the architecture required for modern chronic care management, oncology programs, and high-acuity patient management.
A strong example comes from our work in hypertension management, where an event-driven CIP unified devices, EHRs, and analytical workflows into a real-time ingestion pipeline. This approach worked well because hypertension care depends on rapid response: a single elevated reading can indicate the need for dose adjustment, escalation, or immediate outreach.
By streaming each measurement the moment it occurred, the platform eliminated the delays common in batch-based systems and gave clinicians visibility into patient status in near real time. As a result, care teams were able to intervene earlier, reduce unnecessary escalations, and maintain full compliance while still operating at scale.
AI in Healthcare: Progresses From Analytics to Autonomous Decision Support
Healthcare organizations want AI that actually works in clinical practice, and not isolated demos, not lab-grade prototypes, and not pilots that never scale. But AI can only deliver real clinical and financial impact when the underlying data foundation is unified, reliable, and consistently integrated. A CIP transforms AI from a one-off experiment into a production-ready capability.
Struggling with fragmented oncology data and manual workflows? Exlpore how Jelvix built a unified AI-powered data management platform that streamlines oncology operations and unlocks actionable insights.
Without Integration, AI Is Just a Pilot Project
Across the industry, AI is often presented as the “future of healthcare,” yet most AI initiatives never progress beyond isolated pilots. The reason is rarely the model itself – it is the absence of unified, high-quality input data. AI thrives only when it receives clean, consistent, and complete information. In fragmented ecosystems, it gets the opposite: duplicated fields, conflicting values, missing context, outdated measurements, and inconsistent timestamps. This is one of the core EHR integration challenges that continues to block real-world deployment.
This problem is especially visible in oncology, RPM, and chronic-care environments, where patient data comes from dozens of sources, creating severe data fragmentation that AI cannot resolve on its own.
Oncology workflows require structured pathology reports, imaging summaries, lab values, genomic markers, and treatment histories, none of which follow the same format across health systems. RPM platforms stream vitals from heterogeneous devices, often using proprietary data structures. Chronic-care programs rely on EHRs, claims, pharmacy systems, and remote sensors, each contributing partial information.
Without a unified ETL layer inside the CIP to normalize, validate, enrich, and reconcile data, these inputs become incompatible. The model sees fragments, not the full clinical picture, and its predictions fail as a result – a common failure mode in poorly implemented healthcare data integration efforts.
A clear demonstration of this challenge comes from our work in oncology analytics, where the initial datasets were too inconsistent to support reliable modeling. Only after building a centralized ingestion and transformation layer and standardizing inputs from multiple clinical systems did the predictive models produce clinically usable results.
Our ML oncology model succeeded because we unified data sources before modeling. By integrating EHR data, lab results, imaging metadata, and treatment records into a consistent schema, we eliminated the variability that typically undermines model performance. This allowed clinicians to trust the output and enabled the AI system to operate as part of a real clinical workflow, not just a research experiment.
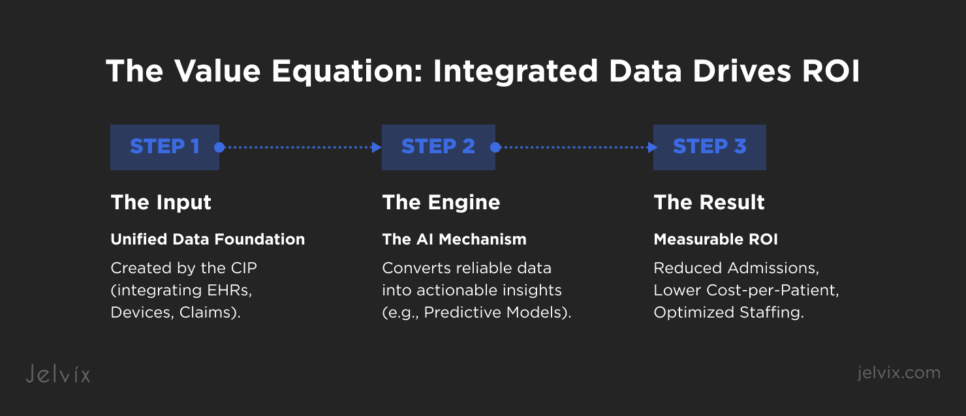
Measuring Value, Not Features: AI Becomes the New Health System ROI
As digital health matures, executives increasingly demand measurable ROI rather than theoretical innovation. Health systems and payors want to see concrete financial outcomes: reduced admissions, fewer escalations, shorter time-to-diagnosis, optimized staffing, and lower cost-per-patient. Vendors are held to the same standard, where platform adoption must translate into revenue expansion and operational efficiency.
AI becomes the mechanism for proving that ROI, but only when it operates on integrated, reliable data. When a CIP eliminates fragmentation and unifies data across devices, EHRs, labs, pharmacies, claims, and monitoring systems, AI can finally produce insights that align with business outcomes. Predictive models identify patients at risk before deterioration occurs, reducing costly emergency visits. Automated care pathways streamline clinical workflows, lowering the burden on overstretched staff. Real-time analytics reveal which interventions are effective and which are not, enabling health systems to invest resources where they matter most.
In other words, AI converts interoperability in healthcare into value. A fragmented environment creates inconsistent metrics and unreliable outcomes. A fully integrated platform provides longitudinal patient visibility, enabling quantification of impact across clinical, operational, and financial dimensions. This is why organizations now view AI not as a feature, but as the ultimate validation that their healthcare integration strategy is working.
The stronger the integration layer, the stronger the ROI story, and the more defensible the business model becomes to investors, payors, and enterprise partners.
LLMs Provide the Clinical Clarity Needed to Bridge Data and Decisions
Despite the rapid expansion of digital tools, clinicians are not asking for more dashboards, more charts, or more notifications. They want simplification. Modern care environments already overwhelm them with EHR notes, vitals from RPM kits, imaging results, lab values, and patient-reported outcomes. This flood of information is one of the reasons why healthcare systems fail to scale. As data volume grows, cognitive burden grows with it, and clinicians cannot keep up without support.
LLMs offer a way forward by transforming raw, integrated data into clear, contextual summaries that fit directly into clinical decision-making. Instead of forcing clinicians to interpret dozens of fragmented metrics, an LLM can synthesize EHR entries, device readings, and historical patterns into a single meaningful narrative. A well-designed model might produce an update like: “Blood pressure has risen steadily over the past 48 hours, with decreased medication adherence and new symptoms suggesting early risk. Consider intervention within the next 24 hours.”
These summaries reduce chart-review time, highlight critical changes earlier, and ensure that subtle patterns are not lost inside documentation noise. When supported by strong health system interoperability, LLMs can access a complete and accurate patient picture rather than fragmented data silos. This is particularly valuable in oncology, hypertension management, and chronic-care coordination, where timely action can prevent deterioration.
LLMs become even more powerful when supported by a Centralized Integration Platform. A CIP provides unified, high-quality inputs, eliminating the data inconsistencies that often undermine AI tools. This creates a practical roadmap for modernizing a legacy healthcare system: clean integrations at the bottom, intelligent summarization at the top.
Rather than adding complexity, LLMs provide the clinical clarity required to operate safely and efficiently in a data-heavy environment. They bridge the gap between integrated data and clinician-ready insight – the missing link in many digital-health architectures.
Summing Up
AI can only succeed when the underlying data foundation is unified. Integrated data is the prerequisite for every form of clinical intelligence, from early-warning scores to predictive modeling to decision-support automation. Once a CIP consolidates data across devices, EHRs, labs, and care workflows, it enables the interoperability in healthcare that allows AI to move beyond isolated pilots and deliver measurable outcomes. And as healthcare systems adopt more complex data sources, LLMs play a critical role in translating that complexity into clinical clarity, enabling clinicians to act quickly, confidently, and at scale.
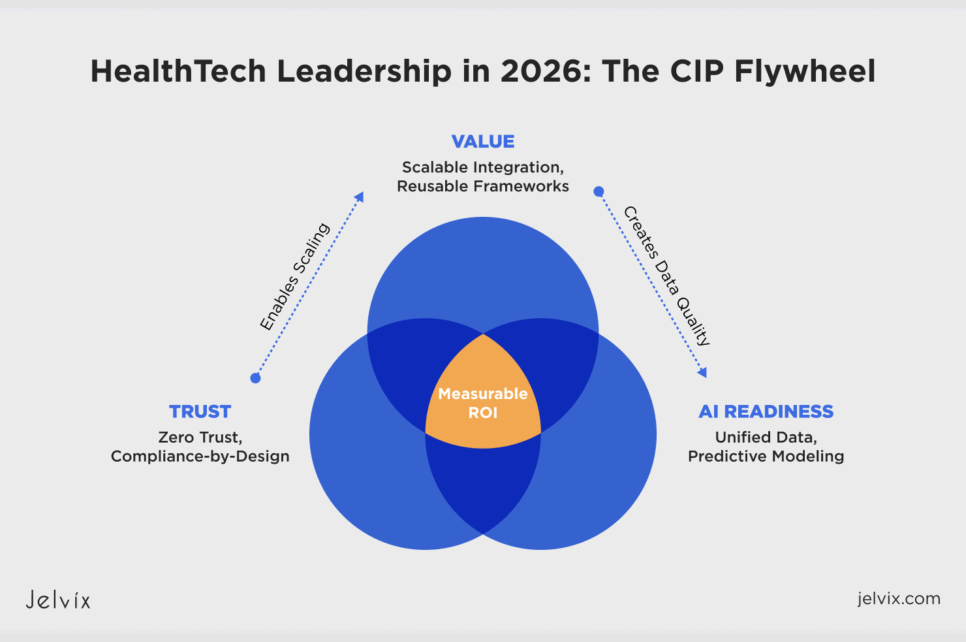
Why CIP Is the Strategic Asset That Will Define HealthTech Leadership in 2026
Healthcare entered the past decade believing that more apps, more devices, and more integrations would bring progress. Instead, fragmentation grew, architectural debt multiplied, and AI remained trapped in isolated pilots. The organizations that will lead in 2026 are those that break this cycle – not by adding more tools, but by unifying them through a Centralized Integration Platform.
A CIP brings together everything modern HealthTech requires:
- Trust, through Zero Trust security, auditability, and compliance-by-design.
- Value, through scalable healthcare API integration, event-driven data flows, and reusable frameworks that eliminate bottlenecks.
- AI readiness, through unified inputs that enable real predictive modeling, real-time analytics, and LLM-driven clinical clarity.
Trust, Value, and AI do not live in separate silos – they reinforce one another. A secure and compliant foundation allows integrations to scale. Scalable integrations create the data quality AI needs. And AI becomes the mechanism for delivering measurable ROI back to health systems, payors, and investors.
This is the architecture Jelvix has been building across cancer care, hypertension platforms, RPM ecosystems, and rehabilitation solutions. And it is the architecture that will determine which digital-health companies break through the noise in 2026 and which fall behind.
Ready to build your 2026 CIP strategy? If your organization is preparing to scale, modernize, or bring AI into clinical production, now is the time to lay the right foundation. We invite you to discuss your integration roadmap with Jelvix experts to design a CIP strategy built for reliability, compliance, and long-term growth.
Tired of integrations that break every time you grow?
Build a stable, future-proof healthcare integration ecosystem with Jelvix.