Imagine walking into a doctor’s office with your whole medical history instantly available. You will save yourself the hassle of having to fill out endless forms, take tests repeatedly, and risk dropping off all critical details. Electronic health records (EHR) and medical records (EMR) are huge conveniences.
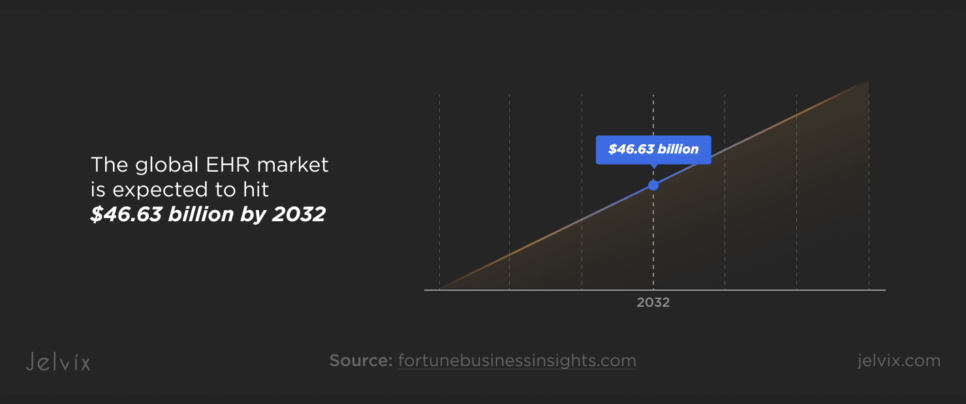
Though EHR and EMR adoption has soared, there have been difficulties along the way. High costs, security risks, and integration headaches are still slowing the progress down. Yet, the numbers show it better than anything—the global EHR market is expected to hit $46.63 billion by 2032, with a steady 5.2% annual growth rate. Governments and tech giants are backing this transformation, integrating AI, cloud computing, and real-time analytics to push healthcare into a new digital era.
Technology advances are also boosting the market. EHR systems with integrated Artificial Intelligence (AI) and machine learning can also help produce better patient outcomes. Furthermore, cloud-based EHR solutions are becoming increasingly popular because they are scalable, cost-efficient, and, most importantly, allow healthcare practitioners to easily handle patient data.
However, what is driving this rapid advance? Why are hospitals and clinics fervently digitizing their files? Let’s talk about the latest industry insights, adoption trends, and the key forces shaping the future of healthcare data management.
What is an Electronic Medical Record (EMR)?
An EMR is the digital version of a patient’s medical chart in a single healthcare facility. It is a complete record of the patient’s medical history at that clinic or hospital, with which doctors can track treatments and monitor progress. Unlike EHRs, designed for interoperability across multiple institutions, EMR systems are confined to one organization and primarily used for internal patient management.
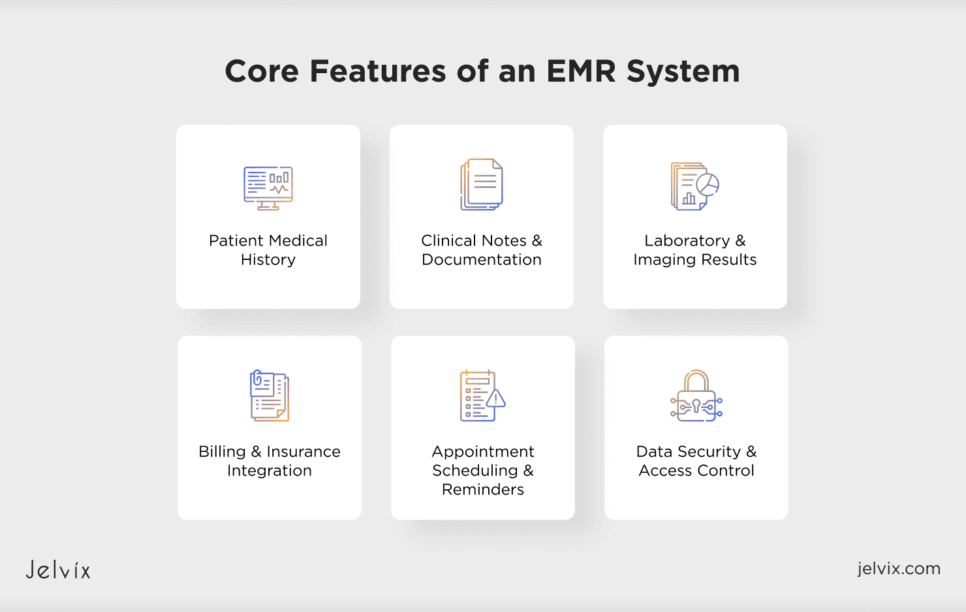
Core Features of an EMR System
EMR systems in healthcare promote productivity and efficiency in patient management and clinical workflow. Here’s what makes them critical to modern healthcare:
- Patient Medical History: Stores comprehensive health records.
- Clinical Notes & Documentation: This feature allows healthcare providers to input and track patient encounters, treatment plans, and observations.
- Laboratory & Imaging Results: Integrates lab reports, X-rays, MRIs, and other diagnostic results for better decision-making.
- Appointment Scheduling & Reminders: Helps with patient appointment management, reducing no-shows.
- Billing & Insurance Integration: Supports medical coding, billing, and claims processing.
- Data Security & Access Control: Ensures that only authorized personnel can access sensitive patient data.
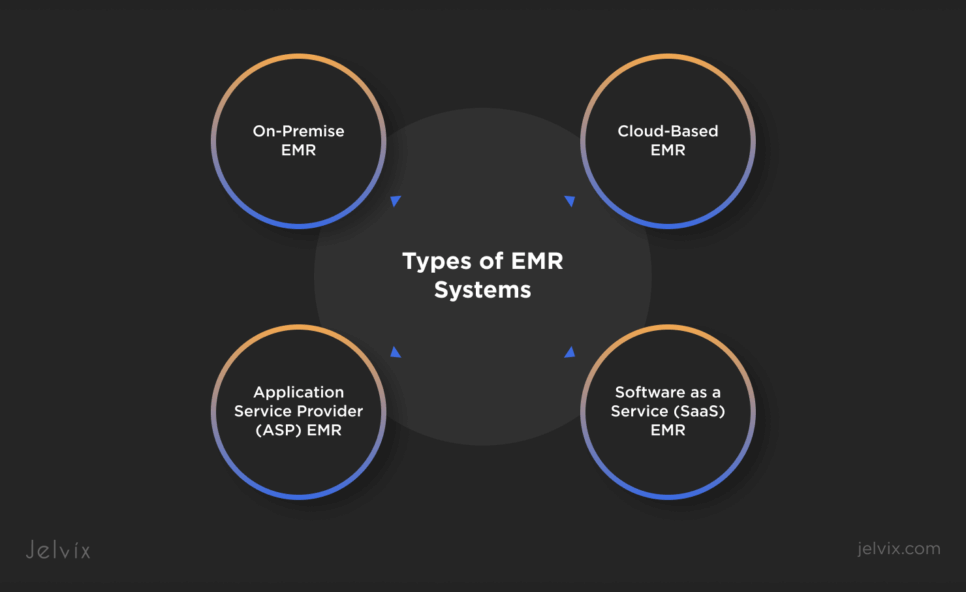
Types of EMR Systems
Not every EMR system is the same. Healthcare establishments need varying degrees of control, access, and security. Therefore, there are four main types of EMRs:
- On-Premise EMR: An EMR set up on a hospital or clinic’s private servers. It offers good security but requires extensive IT upkeep.
- Application Service Provider (ASP) EMR: Software hosted by a third party, accessed via the internet, generally more affordable for small practices.
- Software as a Service (SaaS) EMR: Cloud-based with automatic updates and minimal hardware requirements. Common among mid-sized healthcare providers.
- Cloud-Based EMR: This type of EMR is hosted entirely online and can be accessed with an Internet connection anywhere (even on phones and tablets). However, it can pose security challenges compared to on-premise solutions.
How EMRs Are Used in Healthcare
Electronic medical records make things easier for doctors, providing instant access to a patient’s medical history to make more informed treatment decisions. They also reduce the amount of paperwork required, using technology to help with scheduling, billing, and documentation, meaning more time spent treating patients. Finally, they prevent prescription errors by monitoring medications and awarding potential adverse drug interactions, making the effectiveness of the treatment safer and more reliable.
What is an Electronic Health Record (EHR)?
An EHR is a digital version of a patient’s complete medical history, which includes diagnoses and medications, lab results, imaging reports, allergies, immunizations, and treatment plans. But, unlike EMRs, which are specific to a single healthcare provider or organization, EHRs are designed for broader use. EHRs, with their pervasiveness across multiple providers and organizations, constitute a vital tool in delivering coordinated, patient-centered care.
EHRs allow data flow between hospitals, clinics, pharmacies, and partner organizations. This means that all medical professionals, wherever care is offered, can have access to today’s patient records.
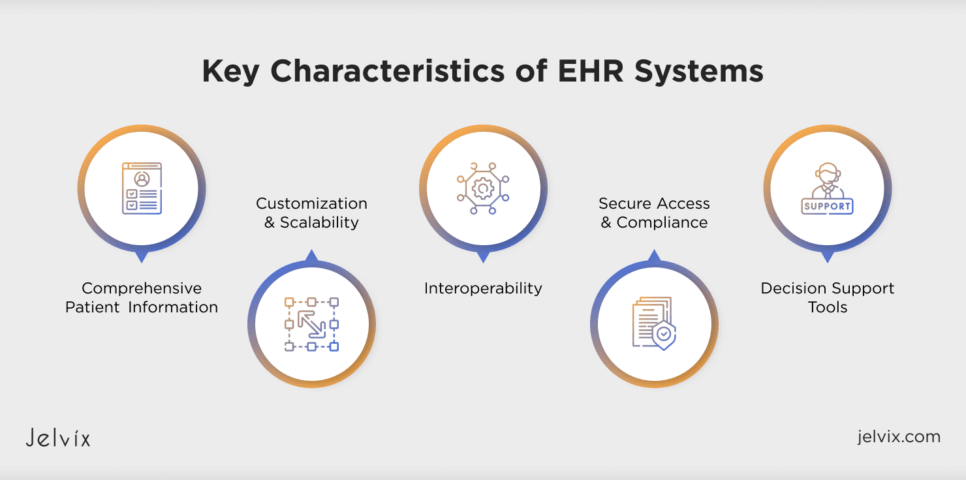
Key Characteristics of EHR Systems
EHR is not just a platform for saving patient data. It leads to real-time integration, analysis, and facilitation of healthcare-related workflows. These are the defining features of EHR systems:
- Comprehensive Patient Information: Organizes the structured digital recording of medical history, diagnostic test results, allergies, immunizations, and treatment plans.
- Interoperability: EHRs are designed to share patient data across various healthcare systems, enhancing communication between providers and helping avoid unnecessary tests and duplicate care.
- Decision Support Tools: Clinical decision support features, such as alerts to possible medication interactions and reminders for preventive treatment, are commonly built into EHRs.
- Customization and Scalability: Several EHR systems serve different healthcare requirements, ranging from huge hospital networks to individual private practices.
- Secure Access & Compliance: EHRs meet HIPAA and other regulatory standards for the secure exchange of patient data.
Are All EHRs Certified Electronic Health Record Technologies (CEHRT)?
As we mentioned, compliance is one of the key features of EHRs. However, not all EHR systems meet the same regulatory and security standards. Certified Electronic Health Record Technology (CEHRT) refers to EHR solutions that comply with government-mandated security, privacy, and interoperability standards. Such certifications, which are required in the US through the HITECH Act and Meaningful Use programs, provide assurance that EHRs:
- Meet Data Security & Privacy Standards: Patient information protection against breaches.
- Enable Interoperability: Seamless data exchange between healthcare providers.
- Support Meaningful Use Initiatives: Allowing hospitals and clinics to qualify for financial incentives by adopting EHR systems that improve patient care.
Although numerous healthcare providers have transitioned to certified EHR systems, some organizations opt for non-certified solutions, which tend to be utilized for internal record-keeping instead of extensive data exchange. However, as the EHR landscape and existing interoperability and compliance requirements advance, systems implemented as CEHRT will eventually serve as the baseline standard.
How EHRs Are Used in Healthcare
EHRs are a central hub for all patient information in day-to-day medical care. Doctors can pull up a patient’s complete medical history, including how they were diagnosed, what medications they were prescribed, and test results from just seconds ago. Specialists can also construct and continually update therapy plans. Medication tracking is central to EHRs: clinicians can immediately look over a patient’s prescriptions or make any needed adjustments during their appointments. Even scheduling is streamlined, with EMRs helping clinics manage appointments, minimize scheduling conflicts, and send automated reminders to patients.
EHRs offer significant advantages beyond general healthcare for specialized fields. For example, in dentistry, digital records track treatment histories, X-rays, and routine cleanings, giving dentists a clear picture of a patient’s oral health. Mental health professionals use EHRs to document therapy sessions, medication plans, and psychiatric evaluations, ensuring continuity of care.
EHRs are also increasingly integrated into medical research and data analysis. By accumulating troves of patient data, they aid researchers in tracking health trends, scrutinizing disease outbreaks, and analyzing treatment results. Data-driven insights that guide policy decisions and resource deployment become very effective. EHRs support outcome analysis in the clinic and hospital, enabling providers to determine the best treatments.
EHRs are customizable to suit different healthcare settings. In hospitals, inpatient EHRs handle complex care plans, track vitals, and record surgeries, enabling doctors and nurses to render care collaboratively. In outpatient clinics, they help track treatments, plan follow-ups, and ensure specialists can access the same patient history. EHRs are used in long-term care facilities to record when residents have received medications and treatments and even log their general well-being.
EHR vs. EMR: What’s the Main Difference?
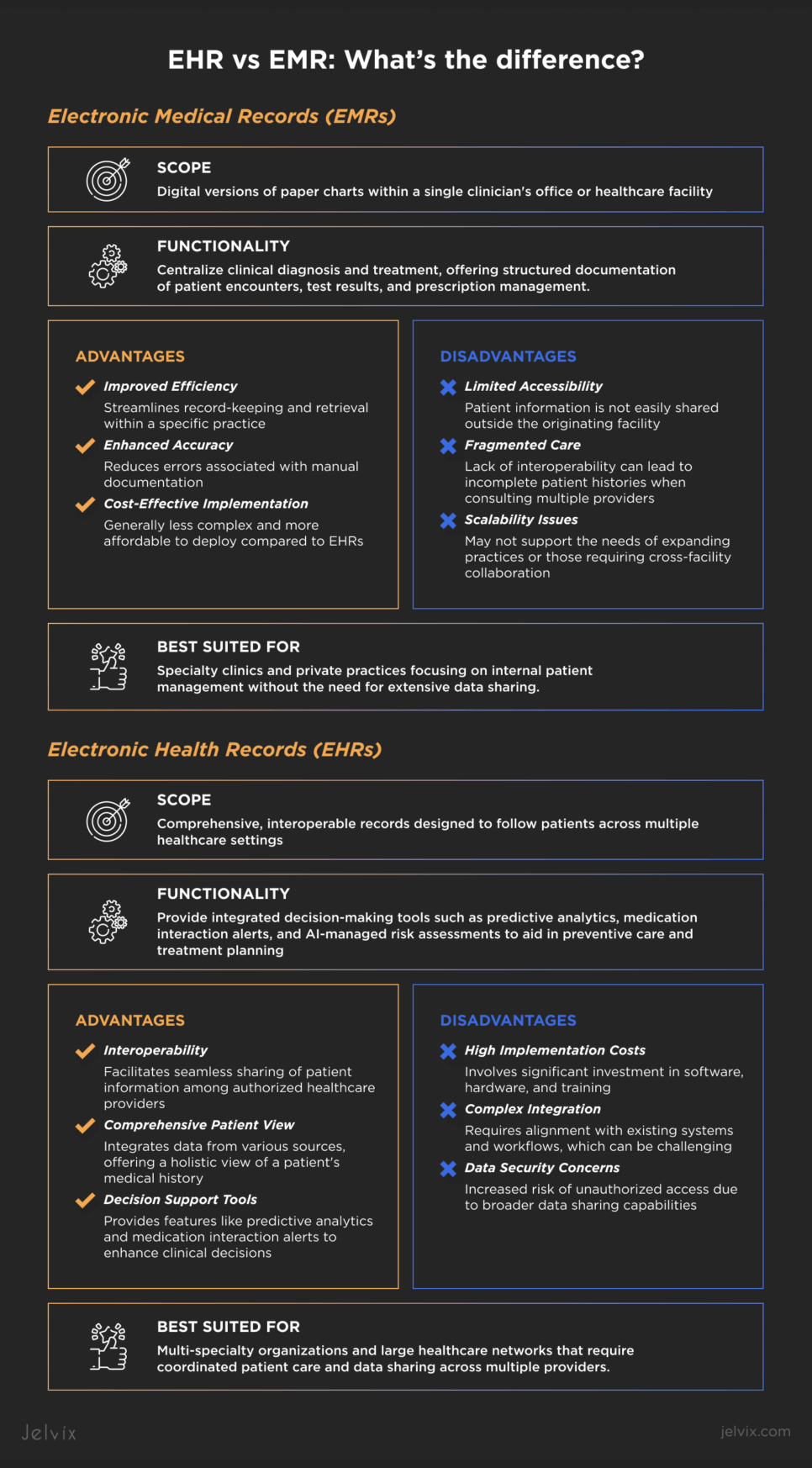
EHR and EMR may seem like interchangeable terms, but they serve different purposes in healthcare. EMRs are digital medical charts that store patient data within a single clinic or hospital. They make record-keeping more efficient but don’t allow access outside that facility. EHRs, in contrast, are engineered to be interoperable so that a patient’s complete medical record travels with them from provider to provider—from primary care to a specialist to the hospital.
The difference between EHR and EMR is more than an access issue. EMRs centralize clinical diagnosis and treatment. They offer a relatively structured means of documenting patient encounters (with notes, vitals, and so on), tracking test results, and managing prescriptions. EHRs, on the other hand, provide integrated decision-making tools such as predictive analytics, alerts for medication interactions, and AI-managed assessments of future risks that help doctors plan preventive care and treatment. EHRs have become a record-keeping system and a dynamic tool for improving patient outcomes.
Another key distinction comes down to who benefits from each system. EMRs are more suited for specialty clinics and private practices, where patient data is kept in a contained environment. A dermatologist, for example, might use an EMR to maintain patient records but has no reason to disperse them beyond the clinic. However, EHRs are built for multi-specialty organizations and large healthcare networks that depend on sharing patient data across multiple providers. If someone has surgery in a hospital and then sees a primary care doctor, an EHR helps both providers access the same critical health information.
The benefits of EHRs are becoming more widely recognized as healthcare moves towards interoperability and data-centric decisions. While EMR systems are well-suited for managing single-practice networks, their ability to interconnect healthcare systems, improve collaboration among specialists, and increase patient safety makes them ideal solutions for today’s medical establishment.
Benefits of EMRs and EHRs
Integrating EMRs and EHRs has significantly transformed healthcare delivery. One primary benefit is improving patient care and safety. By providing professionals with immediate access to comprehensive patient histories, EMRs and EHRs reduce the likelihood of medical errors. A study noted that using EHRs has resulted in more legible, accessible, and secure patient information, which has improved patient management and reduced the need for multiple appointments.
Additionally, these digital records provide a much easier way to access the data, thus facilitating easy coordination between healthcare providers. With EHRs, physicians can quickly access a patient’s medical history, lab results, and other relevant information, which aids in effective collaboration and shared decision-making. This plays a crucial role in maintaining consistent information flow to keep all patient care team members in the loop for better coordination propelled by more efficient care.
EMRs and EHRs improve the quality of care, increase efficiency, and reduce costs in healthcare environments. Digital systems facilitate automation and information sharing, streamline administrative tasks, reduce the time spent on documentation, and minimize the risk of lost or misplaced records.
From a financial perspective, EHRs contribute to significant cost reductions. They help healthcare providers save on labor costs and time by decreasing paperwork through digitized administrative processes. According to a McKinsey & Company report, purposeful utilization of EHR data can result in an overall supply cost reduction of 3.5% to 6.5%. Collectively, these benefits underscore the value of EHRs in promoting safer, more efficient, and cost-effective healthcare delivery.
Disadvantages of EHR and EMR Software Systems
Although using EHR or EMR systems offers many benefits, healthcare providers must also overcome some challenges.
EHR systems can be costly to implement. For example, the average cost for a five-physician practice is about $162,000, with $85,000 allocated to maintenance. These costs include purchasing software, hardware, training, and ongoing support. These types of financial requirements can be a barrier, particularly for smaller practices where budgets are by nature constrained.
With the digitization of patient records, data security, and patient privacy have become particularly concerning. In 2023, 725 data breaches were reported to the Office for Civil Rights (OCR), which shows that unauthorized access to sensitive health information is on the rise. Such breaches threaten patient confidentiality and subject healthcare organizations to legal and financial liabilities.
Transitioning to EHR systems challenges healthcare providers to adapt to new technologies. The learning curve associated with these systems is high. Training staff will understandably result in decreased productivity that may be temporarily compromised as teams learn how to navigate new workflows and interfaces. The justification for such wide-scale training at the outset is to get providers on board to use the systems in ways that actually improve patient care rather than distract from it.
Tackling these challenges is imperative for healthcare organizations to gain complete insight into using EHR and EMR systems without affecting routine operations or data security.
Do Hospitals Use an EHR or EMR System?
Hospitals and healthcare providers use digital systems for clinical records to manage patient care within facilities. Still, the correct choice between EHR and EMR systems will depend on the size and needs of the facility. We’ve mentioned this already, but let’s explore how different EMR systems and types of electronic health record systems correspond to different settings.
Large hospitals and multi-specialty healthcare networks virtually always use EHR systems because they facilitate data sharing between departments and providers and between external healthcare organizations. This need for interoperability is especially pronounced in the hospital setting, where multiple specialists and departments must collaborate to treat complex cases.
The numbers back this up. 96% of non-federal acute care hospitals in the U.S. have adopted certified EHR systems, according to the Office of the National Coordinator for Health Information Technology (ONC). EHRs are now widely used in the hospital setting due to government incentives and an effort to standardize the exchange of patient data to improve outcomes and reduce redundant procedures.
While hospitals use EHR systems, smaller clinics and private practices more often use EMR systems instead. EMRs, in contrast to EHRs, are not designed for multiple providers to access—they are meant to work within a single practice. An EMR—often used by a family doctor’s office or a specialty clinic—could track patient visits, prescriptions, and treatment history. Still, this information won’t seamlessly follow the patient if they change providers.
EMRs cost less, are easier to implement, and require less training than full-fledged EHR systems for small practices. But as care models drive connected care, many clinics have hybrid solutions that facilitate some data exchange with hospitals or outside providers. Many modern EMR solutions for smaller practices now have some referral capability and limited interoperability to help solve it.
EHR vs. EMR Usage Trends
EHR and EMR adoption has moved beyond simple digital record-keeping to becoming the foundation of modern healthcare infrastructure. As the backbone of any healthcare system, EHRs are receiving substantial investments. Moreover, the focus switches to solutions incorporating AI-driven diagnostics, predictive analytics, and patient engagement tools. This transition is not limited to a particular focus on digitizing patient records; it is about leveraging technology to enhance treatment precision and efficiency.
One key driver behind this growth is the rising demand for value-based care. As healthcare systems transition away from volume-based reimbursement towards outcome-driven models of care, providers leverage EHR data analytic tools to monitor patient trajectory, estimate the likelihood of readmissions, and enable improvements in healthcare delivery. A study conducted by Health Affairs reports a 30% decline in medical errors in hospitals utilizing complete EHR systems, solidifying EHRs’ role in bolstering patient safety and effective care.
Another significant trend is the increasing implementation of cloud-based EHR solutions. Implementing on-premise systems requires a significant infrastructure investment. Cloud-based EHRs are a better alternative for small—to mid-sized healthcare providers because they provide flexibility, scalability, and lower maintenance costs. A report from Global Market Insights in 2024 states that cloud-based EHR solutions are expected to register a CAGR of 7.5%, mainly due to their affordability and easy integration with telemedicine and remote patient monitoring systems.
Government Regulations and Incentives
In fact, adopting electronic health records (EHRs) remains a key global focus for governments. The HITECH Act in the U.S. allocated many resources to motivate hospitals and clinics to adopt certified EHR systems, and today, 96% of non-federal acute care hospitals use an EHR.
However, new regulations encourage a shift from merely an adoption to interoperability and data exchange. Under the 21st Century Cures Act, all EHR vendors must enable seamless data sharing, preventing “data blocking” practices that previously restricted patient information flow between healthcare providers.
With the EU Digital Health Strategy, the European Union seeks to create a cross-border EHR network that enables patients and providers to share medical records. Different countries have implemented national policies mandating the use of EHRs and ensuring compliance with those policies to facilitate secure and standardized data exchange.
Stricter global government data security and interoperability regulations are also nudging healthcare providers to move beyond outdated EHR systems and use more innovative, higher-technology platforms for AI data integrations to support decision-making in the moment and across distances.
Custom EHR and EMR Popularity
Healthcare organizations increasingly utilize customized EHR and EMR solutions to match their unique requirements. Conventional, generic software solutions restrict hospitals and clinics from integrating specialty-specific features, automating workflows, and improving the user experience for medical staff.
For example, oncology-specific EHRs have begun incorporating genomic data analysis capabilities, enabling oncologists to tailor treatment plans according to genetic markers. In mental health, custom EHR solutions embed behavioral tracking tools and merge telehealth, making therapy and psychiatric consultation more accessible.
The demand for modular EHR platforms that healthcare providers can customize or tailor functionalities to their specialty further underpins this shift toward a personalized approach to digital health solutions. With the growing number of cloud-based and AI-based EHR technologies, this personalized system notion is becoming more attainable than ever.
Discover how we developed a personalized EHR system that optimized the clinic’s workflow while ensuring maximum privacy and security.
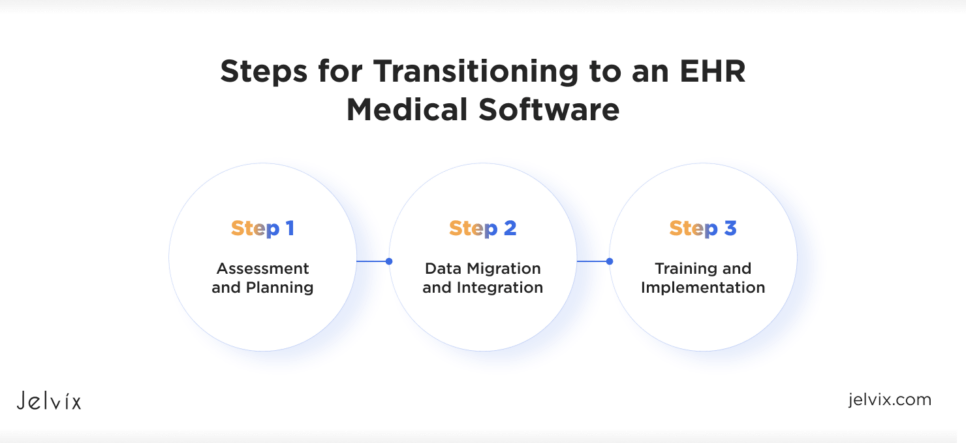
Steps for Transitioning to an EHR Medical Software
Assessment and Planning
The initial phase involves thoroughly assessing your practice’s specific needs and workflows. This involves:
- Assessing the different types of EHR systems on the market—cloud-based, on-prem, and hybrid software.
- Exploring which aligns most closely with your business needs and objectives.
Involving stakeholders across departments at this stage ensures the chosen system will meet the diverse needs of your practice. A well-defined plan should outline the implementation timeline, budget considerations, and key performance indicators to monitor progress.
Data Migration and Integration
Once a suitable EHR system is selected, the focus shifts to data migration and integration. One of the most essential parts is moving the existing patient records and ensuring interoperability with other systems, such as lab information and billing systems. Data accuracy and security during this procedure are crucial; false or lost data could threaten patient care. A well-planned data migration strategy, comprising data mapping, validation, and testing, mitigates the risk of potential issues and ensures a seamless transition.
Training and Implementation
Comprehensive training will be vital to this project, empowering healthcare providers and staff to use the new EHR system effectively. Training has to be tailored to specific user roles and related functionalities within the practice. Creating a support structure to handle user queries and software issues in the early implementation phases can instill user confidence and create an atmosphere conducive to system adoption. It also enables ongoing optimization of the system and workflows through continuous monitoring and feedback mechanisms.
By carefully following these steps, healthcare practices can effectively switch to an EHR system, improving patient care and operational efficiency.
What Does Your Practice Need?
EMRs are digital versions of paper charts within a single practice focused primarily on diagnosis and treatment. They are perfect for smaller practices that need a simple internal-use system. Conversely, EHRs are intended to share patient information among multiple healthcare organizations and support comprehensive patient care. They may be more logical for larger practices or those planning expansion that will require a lot of data sharing.
Custom vs. Off-the-Shelf Solutions
Here are some factors to consider when choosing your EHR solution between custom and off-the-shelf:
- Cost: Custom solutions usually require more initial payments and time to implement, while off-the-shelf software is often ready to go with little initial setup investment. Best of all, while you pay more for a custom software development initially, it ultimately comes out cheaper by reducing the need for future modifications.
- Functionality: Pre-built systems have set features that do not always fit specific practices. Custom solutions are highly tailored to given workflows, making them more flexible and efficient.
- Implementation Time: Off-the-shelf solutions can be implemented quickly, while custom solutions require a longer development period to ensure they meet your exact requirements.
Factors To Consider for Your Healthcare Facility
Here is what to evaluate when deciding whether EMR or EHR systems, custom-built systems, or off-the-shelf solutions are needed:
- Practice Size and Specialty: Larger practices or those needing to share data widely tend to benefit more from EHRs than smaller practices, which EMRs may better serve.
- Cost Considerations: Assess the total cost of ownership, including the initial cost, ongoing maintenance, and the possibility of future revisions.
- Scalability: Ensure that the system can scale with your practice to accommodate growing patient numbers or the addition of more services.
- Integration: Should be able to integrate well with current and future technologies.
- Training and Support for Users: Determine if training services will be available for your system and if they provide ongoing support for successful operations.
Assessing these factors precisely will allow you to choose a system that suits your practice, improves patient care, and bolsters your long-term goals. Despite their differences, both options offer real advantages to contemporary healthcare. Digital records reduce medical errors, improve the accuracy of care, and create more efficient administrative workflows, giving providers time to treat patients rather than administer paperwork.
A government push for EHRs has accelerated the adoption, as have AI and cloud developments that are making the systems more powerful and affordable. Their ability to integrate decision-support tools with predictive analytics and monitor patients in real time makes EHRs a long-term investment in improved healthcare outcomes.
Conclusion
If you still need help determining which system best suits your practice’s requirements, Jelvix offers assistance. Whether you need consulting on custom vs. off-the-shelf solutions, data migration, training, or all of the above, our experts provide EHR and EMR solutions that streamline operations and drive patient outcomes. Contact Jelvix to find a solution that meets your healthcare system’s needs and provides a smooth digital transition for your practice.
FAQ
Can EHR and EMR systems be used together?
Indeed, many healthcare providers utilize both systems. EMRs are typically used for internal patient records, whereas EHRs facilitate data sharing among various healthcare organizations.
How does EHR improve patient engagement?
EHRs allow patients to view their medical history, test results, and treatment plans via patient portals, which enhances self-management and communication with healthcare providers.
What security measures are in place to protect EHR and EMR data?
EHR and EMR systems employ encryption and multi-factor authentication and adhere to HIPAA or equivalent regional regulations to safeguard data security and maintain patient privacy.
How does AI impact EHR and EMR functionality?
Artificial intelligence improves EHR and EMR systems through predictive analytics, automated documentation, and enhanced clinical decision support.
Do EHRs support telemedicine services?
Indeed, contemporary EHRs connect seamlessly with telemedicine systems, facilitating virtual consultations, remote monitoring, and electronic prescriptions.
Need high-quality professionals?
Own the dedicated development team of professionals exclusively for your project.