EHR use has grown significantly across medical practices in the U.S. After COVID-19, for instance, the adoption rates increased from 6.6% to 81.2%, confirming the necessity of modern tech solutions in healthcare.
However, EHR implementation is pretty costly and may require a significant initial investment. Add expenses for annual system maintenance, educating staff, and adding vital upgrades, and you’ll get a price that can hardly be called loyal.
If you want to adopt a modern EHR system, avoid the hidden costs related to implementation and maintenance, and justify ROI, read this article. You’ll find out how much EHR software really costs and how to set a realistic budget for successful adoption.
Why Budgeting for EHR Is Critical for Clinics in 2025
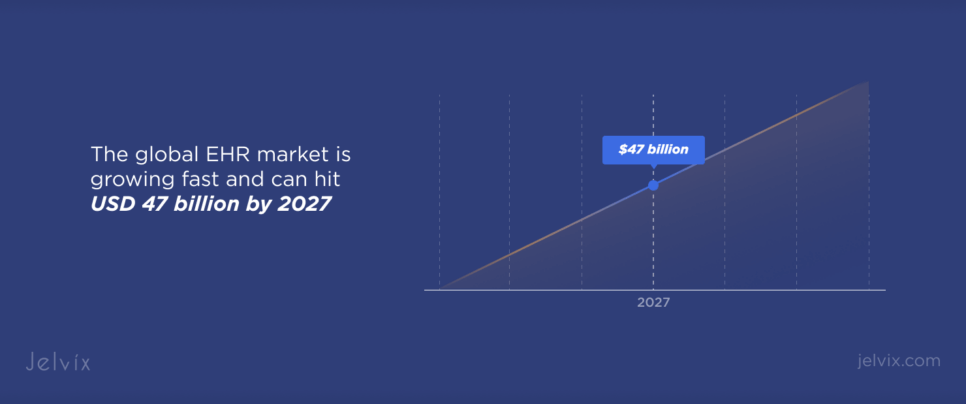
The global EHR market is growing fast and can hit USD 47 billion by 2027. However, the more clinics adopt these systems, the more complex they get, and this drives up the cost of implementation and support.
If you seek medical software development services and plan to adopt an EHR in 2025, get prepared for the costly setup, training, and data migration. You need to plan your budget accordingly to ensure financial stability and efficiency at your clinic.
The True Cost of Implementing EHR Solutions
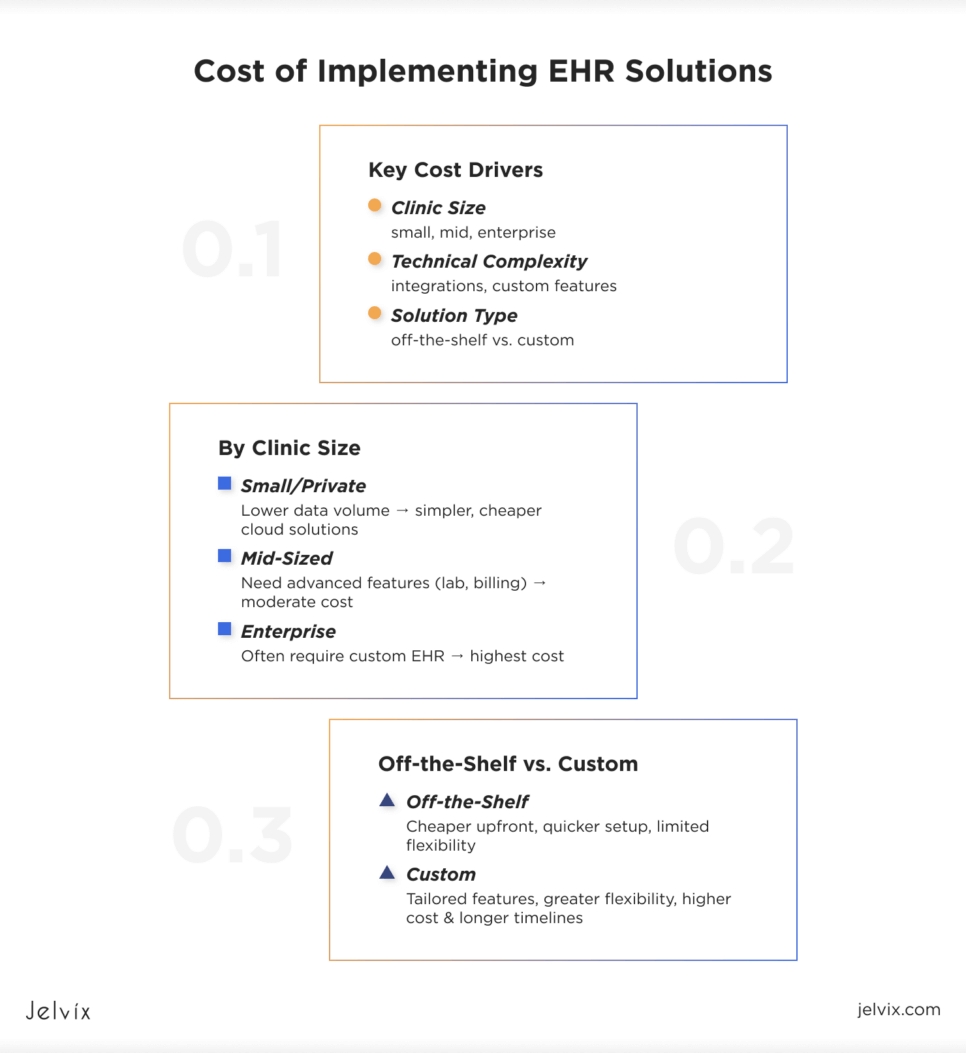
Switching to a new medical solution like EHR is a complex decision that requires a clear budgeting strategy. The cost can vary depending on your clinic’s size, its technical necessities, and the type of solution itself.
An EHR Cost for Small, Mid-Sized, and Enterprise-Level Healthcare Providers
Smaller and private practices need to process less data and have lower patient flows, so the price of EHR implementation will be much lower for them compared to more prominent clinics. Usually, it’s enough for them to use simple cloud solutions with basic functionality that offer a subscription-based model.
Mid-sized providers may require more advanced features like integration with labs, billing systems, and scheduling software. At the same time, enterprises often need a custom solution with tailored functions, which skyrockets the price of EHR tools.
Off-the-Shelf vs Custom Solutions: EHR Cost Overview
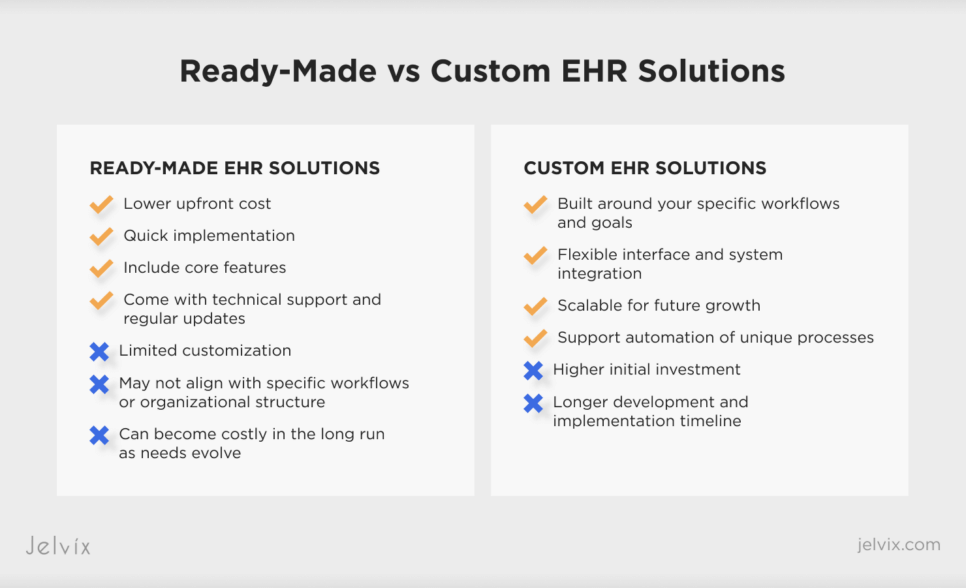
Depending on your needs, you can choose custom software vs off-the- shelf EHR solution.
Pre-made EHR systems are easy to set up with no need to build anything from scratch. They’re cheaper upfront and a good fit for smaller clinics that need something fast. But they usually don’t offer much flexibility, and that can be a problem if your workflows are more complex.
Custom EHRs are built to match the specific needs of your healthcare organization. They allow for flexible interface design, automation of unique workflows, and improvement in overall efficiency. However, these solutions usually cost more and take longer to implement.
EHR Implementation Cost Breakdown: What You Really Pay for
The cost of implementing an EHR system consists of several spending categories. You need to understand and evaluate them all to avoid unexpected expenses.
Initial Investments
Before you even start adopting an EHR tool, you’ll need to pay for software licenses, servers, computers, and other devices. Also, don’t forget about infrastructure expenses if you need to update your local network or purchase additional hardware.
Implementation and Training
You need to pay to adapt your EHR to your specific workflows and clinical processes, migrate data, create templates, and train staff. Doctors and nurses need to understand how to use the new system. Otherwise, it will become underused, and you’ll simply waste money.
Direct and Indirect Expenses
Direct expenses include the cost of the EHR system itself, as well as training, consulting, and technical support. Indirect costs mean reduced staff productivity during the adaptation period, a temporary increase in patient processing time, and changes in existing EHR workflow.
Recurring and Maintenance Fees
These expenses usually include annual or monthly fees for technical support and system updates, as well as cloud data storage, backup, and protection. You also need to consider costs related to staying compliant with industry regulations.
Hidden Costs
Business owners often overlook costs related to LIS, RIS, and CRM integration with EHR systems. Hidden expenses may also include long downtimes during the transition and the time staff spends learning the new system.
Custom vs Ready-Made EHR Solutions: Cost and Flexibility
Both ready-made and custom EHR solutions have benefits to offer. The choice usually depends on the size of your entity, staffing needs, and available budget.
Advantages and Drawbacks of Ready-Made Solutions
Ready-made EHRs are quicker to implement and cost less upfront. They typically include core features, technical support, and regular updates. However, they may not fully align with the unique workflows or structure of your healthcare organization.
Benefits and Disadvantages of Custom Development
Custom EHRs are built around your internal processes, staff structure, patient types, and specific goals. They allow flexible interface design, integration with other systems, automation of unique workflows, and future scalability. On the downside, they usually take longer to build and require a higher initial investment.
Long-Term ROI
From a long-term perspective, custom EHRs often provide more value. They improve efficiency, reduce administrative workload, and adapt to new needs without requiring a platform switch. Off-the-shelf solutions, while cheaper at first, may lead to extra costs later as your organization grows or requires more flexibility.
When You Need To Opt for a Custom EHR
A custom solution makes more sense for healthcare providers with complex internal processes, high security requirements, or the need for deep integration with other systems, such as telemedicine platforms, lab services, or CRM tools.
Discover the most trusted EHR systems to support clinical workflows, enhance patient care, and ensure regulatory compliance for growing healthcare organizations.
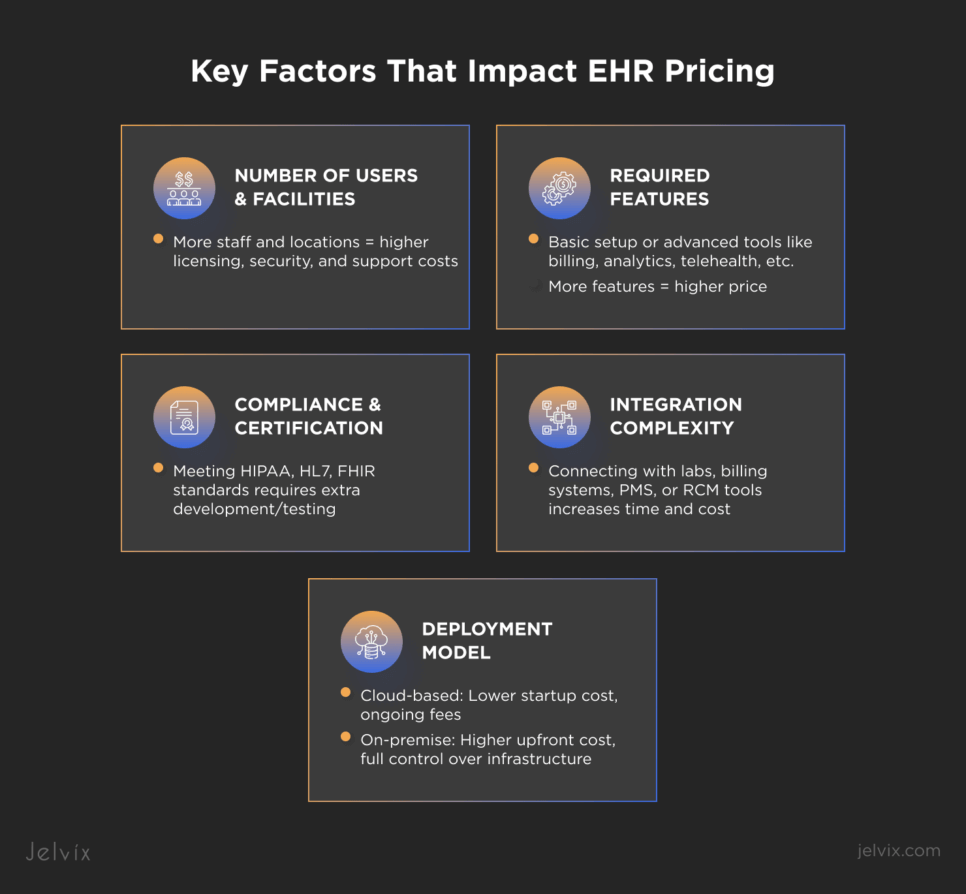
Key Factors That Impact EHR Pricing
The cost of implementing an EHR system primarily depends on the type of chosen platform. However, additional technical and business factors can push the price up.
Number of Users and Facilities
The more staff and locations that need access, the higher the licensing, scalability, security, and support requirements, leading to higher overall costs.
Required Features
Before implementing an EHR, you need to asses what functionality you need. This can be just a basic clinical setup, or also billing, analytics, telehealth, and patient engagement tools. The broader the feature set, the higher the price.
Compliance and Certification Needs
As noted earlier, you need to meet standards like HIPAA, HL7, and FHIR. This requires additional development and testing time, especially for systems handling loads of sensitive data.
Integration Complexity
If your system needs to connect with labs, PMS, billing tools, or RCM platforms, expect more time and cost for custom integration work.
Deployment Model
Cloud-based systems are typically quicker and cheaper to launch, but they come with ongoing subscription fees. On-premise solutions have higher upfront costs but give you complete control over infrastructure.
Cloud vs On-Premise EMR Cost: What’s Better for Your Budget?
It’s true that the choice between cloud and on-premise EHR depends on implementation costs. It also impacts long-term expenses, and you need to be ready for that.
Infrastructure and Security
Cloud solutions don’t require investing in hardware updates or server costs, because it’s your provider’s responsibility to take care of EHR safety, data backup, and system upgrades.
Local systems require their own server hardware, security settings, and dedicated specialists to work correctly.
Scalability and Maintenance
Cloud models are easy to scale, as you only add new users and features without disrupting your workflows. On-premise systems, on the other hand, are more complicated to expand. You’ll need frequent system updates and more maintenance resources.
Long-Term Cost Impact
Cloud EHRs usually cost less to start, but subscription fees add up over time. After a few years, you might end up paying more than you would for a one-time on-premise setup. With local systems, the big costs come up front, but you own the system and have more control over long-term spending. The best option depends on your budget and how fast your clinic is growing.
How Medical Entities Can Pay for EHR Systems
The financial model of EHR implementation can greatly impact the overall expenses and return on investment. You need to choose a format that perfectly suits your budget and growth plan.
Ownership vs Subscription
Ownership model means you buy the entire system, paying just once for licensing, servers, deployment, and maintenance. The initial investments are more considerable, but can be more profitable in the long run.
In a subscription-based mode, you pay monthly or annually to access the EHR as a service. This reduces startup costs, but over time, the costs can be comparable to purchasing a complete system.
Government Incentives or Compliance Penalties
Some countries offer government programs that support healthcare digitalization by partially covering EHR implementation costs. On the other hand, failing to meet requirements like security standards or reporting rules can lead to financial penalties or limitations in working with public healthcare programs.
Financing and ROI Calculation
Many medical practices consider phased financing, leasing, or partnerships with tech vendors to avoid budget strain. However, you need to evaluate not just the direct costs, but also the expected return, such as time saved, reduced administrative load, and increased revenue from better patient service.
Understanding Maintenance and Support Cost of EMR Software
If you decide to implement an EHR system, don’t expect that expenses end here. You need to invest in upgrading and supporting it, otherwise it won’t be able to comply with changing regulations and work without disruptions.
The Cost of Updates, Compliance, and Technical Support
EHR support and maintenance usually include security and functional updates, compliance with regulations, data backup, error correction, tech support for staff, and integration with other systems. Cloud solutions usually add all these as a part of their subscription, while on-premise EHRs require additional budgeting.
Cost Control Strategies
It’s easy to exceed your budget if you don’t know all the aspects of EHR implementation. To prevent this from happening, ensure to have a transparent agreement with the provider, which clearly states what is included in the service and how much it costs.
It is also worth choosing solutions that support automatic updates and have documentation for self-solving typical issues. Regular audits of EHR usage will help to identify unnecessary bottlenecks that need optimization.
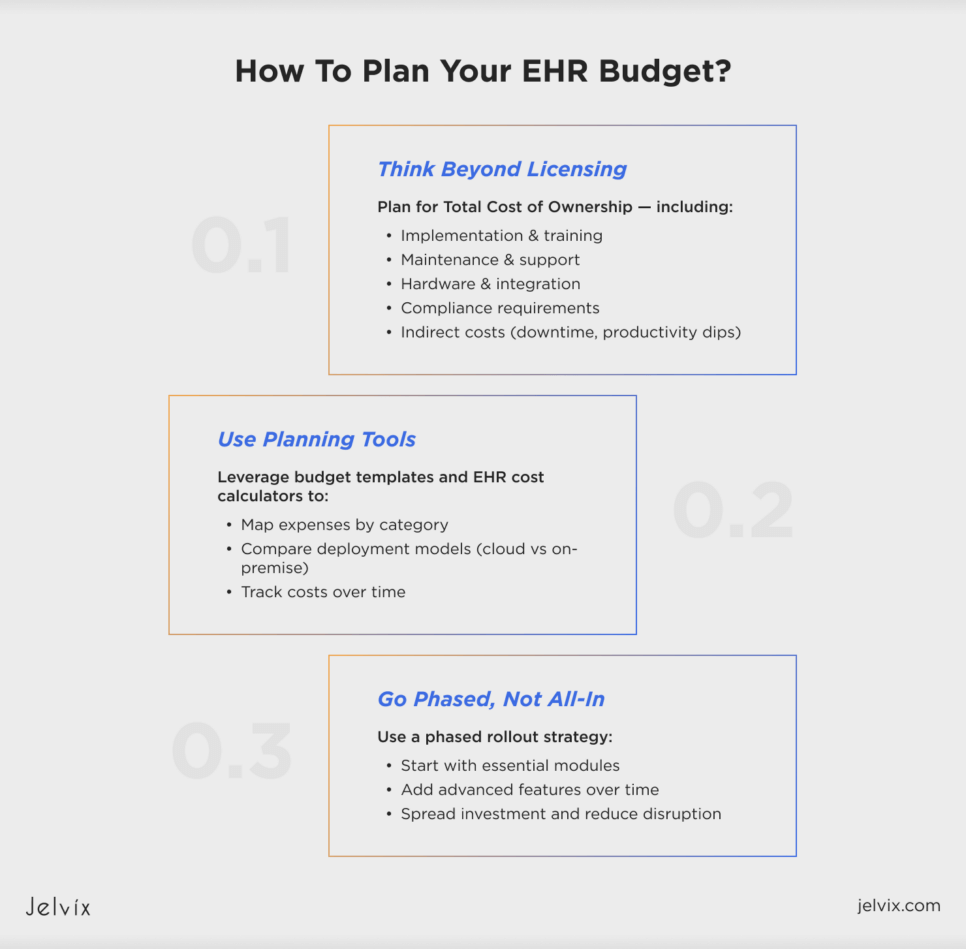
Electronic Medical Records Software Cost: Planning a Realistic Budget
Planning your EHR budget isn’t just about the initial software price, but about understanding the full picture and making long-term decisions.
Estimating Your Total Cost of Ownership
To budget effectively, you need to look beyond licensing costs. Factor in implementation, training, maintenance, support, hardware, integration, and compliance. Don’t forget about indirect costs like productivity dips during onboarding or system downtime.
Tools and Templates for Cost Planning
Budgeting doesn’t have to be guesswork. You can use cost planning templates or EHR budget calculators to map out expected expenses by category. These tools help compare deployment models and track costs over time.
Budgeting for Phased Implementation
Rolling out your EHR in phases, starting with essential modules and adding more later, helps control costs and reduce disruption. This approach also gives your team time to adapt while spreading investment over a more extended period.
EHR Cost-Benefit Analysis
Investing in an EHR system can feel like a significant financial commitment, but when implemented thoughtfully, the return often outweighs the cost.
EHRs improve how practices manage patient data, reduce paperwork, and help providers make more informed decisions. With better documentation and automation, clinics can streamline billing, reduce administrative errors, and cut down on operational costs.
A well-designed EHR improves workflow efficiency by making records easier to access, reducing duplication, and speeding up routine tasks. This leads to better patient outcomes, faster diagnosis, and more coordinated care, which all translate to long-term value for both providers and patients.
Top EMR Pricing: Epic, Cerner, and Athenahealth
Choosing the right EHR system starts with knowing what’s out there and what it might cost you. While many providers go with market leaders, price and limitations often push others toward custom solutions.
Market Leaders and Their Price Ranges
Epic, Cerner, and Athenahealth are some of the most popular EHR systems on the market.
Epic and Cerner are often used by larger hospitals. They offer advanced features but can be expensive. For instance, Cerner can cost around USD 1 million to smaller hospitals, over USD 60 million to larger clinics. The final cost depends on factors like hospital size, existing infrastructure, and project scope.
Athenahealth is more common in small and mid-sized clinics. It’s cloud-based and more affordable, and can be offered as a stand-alone product for about USD 140 per month per provider. Other systems like NextGen and eClinicalWorks can fall into this price range, depending on the features you need.
Why Choose Custom Solutions
Off-the-shelf systems don’t always fit every clinic’s workflow. Some providers find the user experience clunky, the features too broad or too limited, or integration too difficult. When that happens, they turn to custom EHRs built around their specific needs, although the upfront costs can be higher.
Check how Jelvix developed a scalable, user-friendly EHR platform to streamline clinical workflows, improve patient data access, and support decision-making in healthcare.
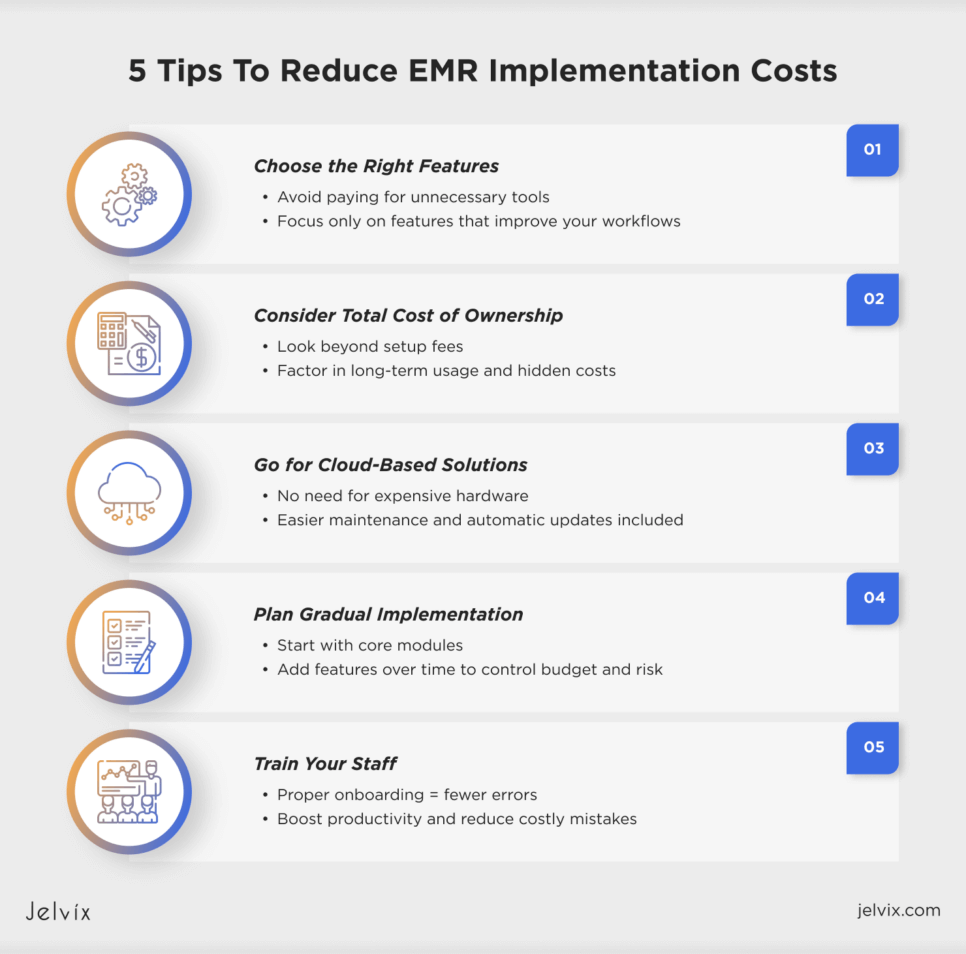
5 Tips To Reduce EMR Implementation Costs Without Compromising Quality
EHR implementation is a costly process. However, you can reduce associated expenses without compromising quality or safety.
1. Choose a System That Suits Your Needs
One of the most common mistakes during EHR adoption is paying for functionality you don’t really need. Ensure to assess your clinic’s needs and select only those features that will improve your workflows before you make an investment.
2. Consider the Cost of Ownership
Paying for EHR implementation is just a part of the total expenses. Think about how much using this system will cost you in the long run, especially if your solution is pre-made.
3. Opt for Cloud Solutions
Unlike local servers, cloud EHRs don’t usually require expensive hardware to operate, and they’re much easier to maintain. Automatic updates and basic safety features are already included, so you don’t need to spend funds on IT teams.
4. Plan for a Gradual Implementation
Instead of rolling out the whole system, start with basic modules and then add the remaining functionality. This way, you can distribute expenses and minimize the risks of system disruptions.
5. Invest in Staff Training
It’s not enough just to implement a modern EHR. Your medical and administrative workers must know how to work with it. This will cut down on time and reduce the likelihood of manual errors that may cost a lot in the future.
Why Custom EHR Software Development Can Be Better for Your Business
Off-the-shelf EHR systems may work for some clinics, but they often fall short when clinics need to put flexibility, control, and long-term growth first.
Customized Workflows, Integrations, and Compliance
A custom EHR is built around your specific processes, not the other way around. It fits your clinical workflows, supports your preferred integrations (like lab systems or billing platforms), and ensures full compliance with healthcare regulations like HIPAA or GDPR.
Competitive Advantage in Specialized Care
If your clinic offers specific services, such as behavioral health, oncology, or rehabilitation, you can build tools and templates that reflect how your teams work using a custom solution. This means faster onboarding, fewer errors, and better care delivery.
Scalability and Future-Proofing
Custom systems can grow with you and allow you to expand locations, add providers, and roll out new services. A tailored EHR gives you the flexibility to scale without significant disruptions or expensive rebuilds.
Summing Up: Strategic Investment vs Short-Term Savings
Choosing the right EHR for your medical entity isn’t just a matter of initial investment, but also an important decision that will impact your flexibility and scalability. Cheaper solutions may seem a better option at first, but can limit your clinic’s ability to expand and serve more patients. Custom tools cost more, but can support your workflows and help your clinic expand without running into roadblocks.
At Jelvix, we understand the importance of building comprehensive solutions to specific clinical needs. Our software development services include creating EHR tools from scratch, implementing them into existing settings, and also customizing pre-made platforms to fit your business needs. Contact us for a customized consultation on developing an EHR that can support your long-term success.
Ready to scale?
Partner with a dedicated development team that delivers beyond expectations.