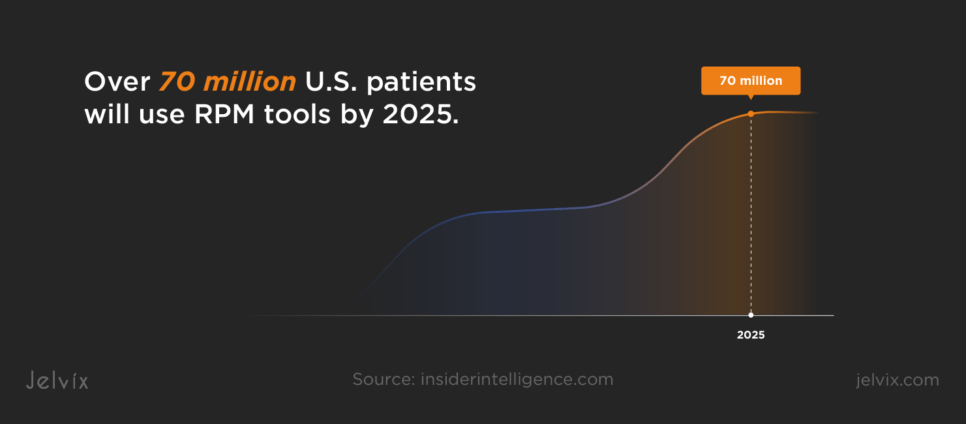
The integration of telemedicine and remote patient monitoring solutions into healthcare has changed the way medical services are delivered. Insider Intelligence estimates that over 70 million U.S. patients will use RPM tools by 2025.
Telemedicine and RPM can become life-savers for patients who require immediate access to care or face challenges in obtaining it due to geographical distances or disabilities. Yet, the complexities involved in developing and integrating remote monitoring solutions into existing systems can pose significant challenges.
If you’re a healthcare provider or a vendor struggling to overcome technological, regulatory, and patient engagement barriers in your remote monitoring solutions, this article is for you. You will reveal key challenges that RPM faces so far and ways to overcome them, look through common use cases, and analyze the effectiveness of real-world solutions implemented by other companies.
What Is Remote Patient Monitoring and Telemedicine?
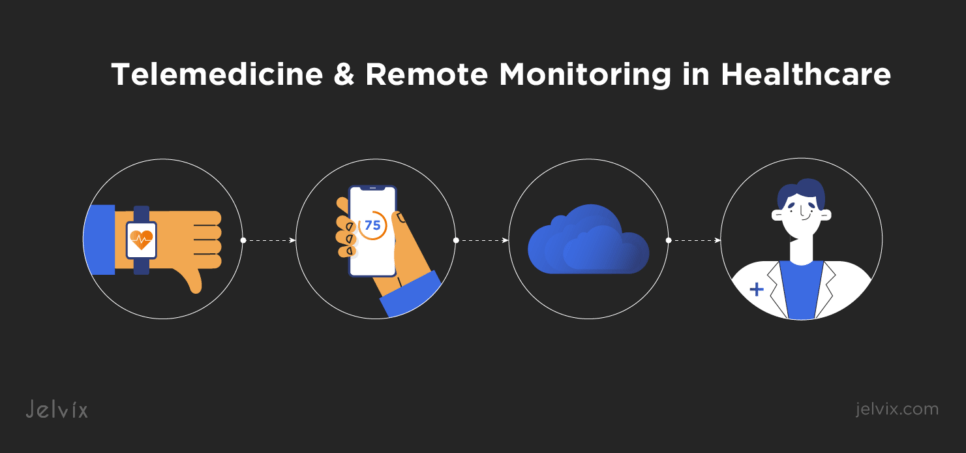
Telemedicine facilitates direct communication between patients and physicians through digital platforms, allowing for consultations, diagnoses, and treatment advice remotely. RPM solutions involve the use of digital technologies to collect health data from patients in one location and electronically transmit that information to healthcare professionals in different locations for assessment and tailored recommendations.
Together, RPM and telehealth expand access to care, improve the efficiency of healthcare delivery, and enable personalized patient management.
Telemedicine and Remote Monitoring in Healthcare: Evolution and Current Trends
The COVID-19 pandemic significantly accelerated the adoption of telemedicine and RPM solutions, breaking regulatory barriers and shifting patient and physician attitudes towards favoring remote care. A survey by APA revealed that 92% of physicians provided services using telehealth in 2020. 76% of them used telemedicine compared to only 20% using it before the pandemic.
The integration of wearable and IoT devices into remote monitoring has expanded, too. Patients can use smartwatches, glucometers, and blood pressure monitors to track their vital signs and health metrics from home. There is an increased emphasis on designing telemedicine and RPM platforms that are user-friendly, accessible, and tailored to meet diverse patient needs.
Telehealth Consultations and Diagnostics Use Cases
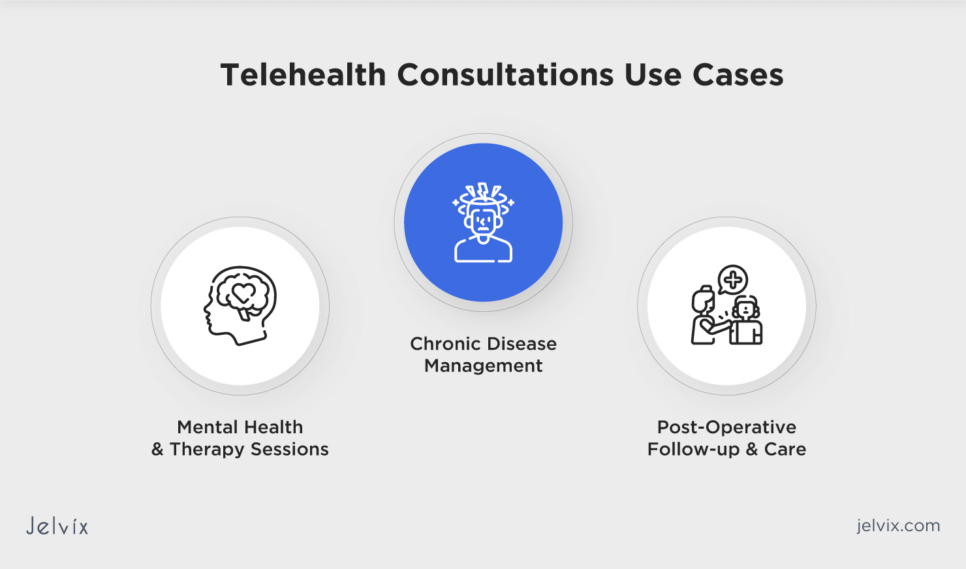
Telehealth consultations and diagnostics have become integral components of modern healthcare, providing remote patient monitoring services across various medical fields. Common use cases show why remote patient monitoring is important and highlight the versatility and effectiveness of telehealth in addressing a wide range of healthcare needs.
Mental Health and Therapy Sessions
Telehealth has changed mental health care by offering therapy sessions, psychiatric evaluations, and ongoing support through online platforms. Mental health was ranked highest among the specialties using telehealth. As reported by Epic Research, 37% of mental health visits occurred virtually in 2023.
The remote approach has made mental health services more accessible to individuals who face barriers to traditional in-person therapy, such as stigma, geographical limitations, or physical disabilities.
Chronic Disease Management
Managing chronic diseases such as diabetes, hypertension, and heart disease through telehealth allows for regular monitoring and adjustments to treatment plans without the need for frequent in-person visits. This includes medication management, lifestyle counseling, and monitoring of vital signs through connected devices.
Post-Operative Follow-up and Care
Telehealth provides an efficient way to conduct post-operative follow-ups, allowing physicians to assess recovery, manage wound care, and adjust pain management plans remotely. This can reduce the need for patients to travel, which is beneficial during the early recovery phase when mobility might be limited.
Remote Patient Monitoring System Use Cases
RPM solutions enhance patient care across different healthcare needs and populations. By leveraging RPM technologies, physicians can offer personalized, proactive, and efficient care, significantly improving patient outcomes.
Monitoring for Chronic Conditions
The WHO warns that chronic diseases like cancer, diabetes, heart and respiratory conditions might be the cause of 86% of the 90 million deaths annually by 2050. RPM systems can help reduce this trend by enabling the continuous monitoring of patients with chronic conditions. Devices like glucose monitors and blood pressure cuffs can transmit data directly to physicians, allowing for real-time adjustments to treatment plans.
Elderly Care and Monitoring
RPM technologies support the elderly by monitoring vital signs, detecting falls, and tracking medication adherence, all from the comfort of their homes. Wearable devices and home sensors can alert caregivers to potential health issues or emergencies.
Rehabilitation and Physical Therapy
For patients undergoing rehabilitation or physical therapy, RPM devices can track progress, mobility, and activity levels. This data helps therapists tailor recovery programs to the patient’s specific needs and adjust them based on real-time feedback.
Medication Adherence and Management
RPM systems can remind patients when it’s time to take their medication and monitor their adherence to treatment plans. These systems can alert physicians if a patient misses a dose, allowing for immediate follow-up.
Explore how Jelvix created a telehealth solution for RPM, enabling the tracking of vital signs, instant data transmission to doctors, and enhancing medical access with user-friendly integration and wearables.
Integrating Telemedicine and RPM into Healthcare Systems
Integrating telemedicine and RPM solutions into healthcare systems involves careful consideration of technical infrastructure, seamless integration with Electronic Health Records (EHRs), and adherence to industry regulations.
Technical Infrastructure Requirements
Technical infrastructure requirements for telemedicine and RPM include reliable Internet for seamless communication, secure data handling to protect patient privacy and comply with regulations, and compatible hardware and software for ease of use. Scalability is vital to accommodate future growth. Addressing these requirements will help ensure effective, secure, and sustainable digital health services.
Integration with Electronic Health Records
A remote healthcare monitoring system should seamlessly integrate with EHRs to streamline data flow and enhance care quality. This integration allows real-time health data from RPM tools to be directly accessible within a patient’s EHR, supporting informed decision-making and personalized care. Key to this process is adhering to interoperability standards to ensure that different systems communicate effectively and securely, overcoming interoperability challenges, and maintaining data security.
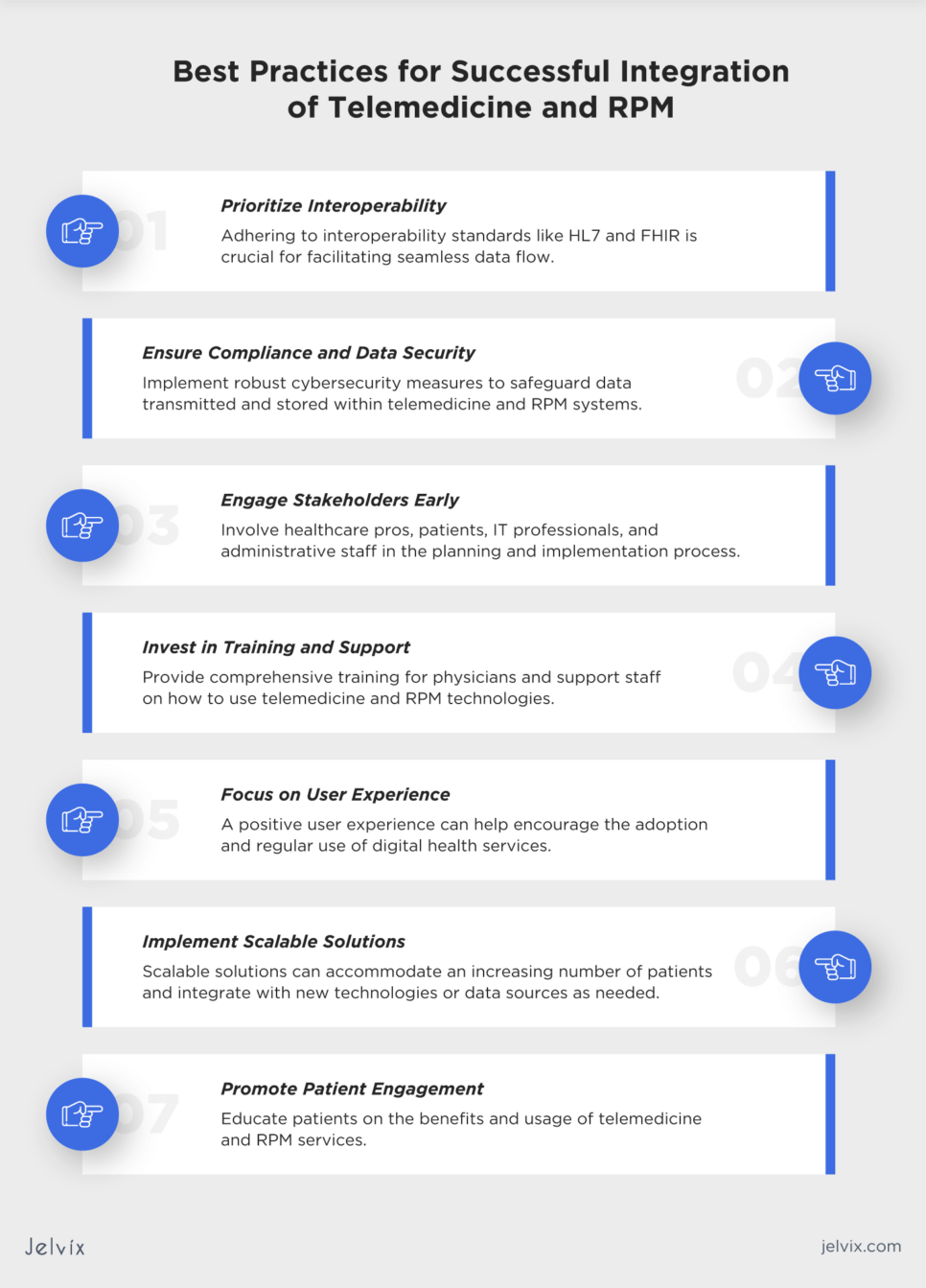
Best Practices for Successful Integration of Telemedicine and RPM
Integrating telemedicine and RPM into healthcare settings requires thoughtful planning, execution, and management. The Jelvix team recommends that you consider the best practices listed below for a successful integration.
Prioritize Interoperability
Ensure that telemedicine and RPM platforms can seamlessly exchange data with EHRs and other healthcare systems. Adhering to interoperability standards like HL7 and FHIR is crucial for facilitating the seamless data flow.
Ensure Compliance and Data Security
Adhere to healthcare regulations such as HIPAA in the U.S. or GDPR in Europe to protect patient privacy. Implement robust cybersecurity measures to safeguard data transmitted and stored within telemedicine and RPM systems.
Engage Stakeholders Early
Involve healthcare pros, patients, IT professionals, and administrative staff in the planning and implementation process. Their input can provide valuable insights into user needs and system requirements.
Invest in Training and Support
Provide comprehensive training for physicians and support staff on how to use telemedicine and RPM technologies. Offer ongoing technical support to address any issues promptly, ensuring minimal disruption to healthcare processes.
Focus on User Experience
Design telemedicine and RPM interfaces to be intuitive for both patients and physicians. A positive user experience can help encourage the adoption and regular use of digital health services.
Implement Scalable Solutions
Choose tools that can grow with a healthcare organization. Scalable solutions can accommodate an increasing number of patients and integrate with new technologies or data sources as needed.
Promote Patient Engagement
Educate patients on the benefits and usage of telemedicine and RPM services. Clear communication and easy access can significantly enhance patient engagement and satisfaction.
Ensuring Patient Privacy and Data Security
Prioritizing patient privacy and data security is essential for fostering trust, ensuring regulatory compliance, preventing breaches, and facilitating the effective and ethical delivery of digital healthcare services. Make sure your remote monitoring solution takes the following security measures:
- Adhere to legal and regulatory standards: comply with laws like HIPAA and GDPR by implementing protective policies for patient information use;
- Encrypt data transmission and storage: protect all data in transit and at rest with strong encryption algorithms, such as AES and RSA, to prevent unauthorized access;
- Implement access controls: use multi-factor authentication and role-based permissions to ensure only authorized personnel access patient data;
- Regular security audits: conduct assessments and audits to identify vulnerabilities, reviewing security measures regularly;
- Secure patient authentication: employ secure and user-friendly methods for patient access to safeguard their privacy and data;
- Educate patients and staff: provide training on data privacy and secure practices to prevent phishing and other security threats;
- Develop an incident response plan: have a plan to quickly address data breaches;
- Patient consent and transparency: obtain informed consent and be transparent about how patient data is used and managed.
Compliance with Healthcare Regulations
As noted earlier in this article, compliance with healthcare regulations, such as HIPAA and GDPR, is critical for the smooth work of telemedicine and RPM services. This compliance ensures the protection of patient privacy and the security of health data, which are fundamental to maintaining patient trust and the integrity of healthcare services.
If you plan to empower your healthcare solutions with AI, make sure you are aware of the new EU AI Act aimed at ensuring that AI tech is used safely and doesn’t compromise patient privacy.
Navigating Reimbursement Policies and Insurance Coverage
By understanding healthcare settings, maintaining accurate documentation, and leveraging technology, providers, and vendors can maximize reimbursement opportunities, ensuring the sustainability of telemedicine and RPM services:
- Stay updated: be in the know of the latest changes in reimbursement policies and insurance coverage for telemedicine and RPM at both federal and state levels;
- Insurance partnerships: work closely with insurance companies to understand their specific requirements for telemedicine and RPM service reimbursements;
- Accurate coding: ensure accurate and up-to-date coding for telemedicine and RPM services. Use the correct billing codes that reflect the service provided, as this directly impacts reimbursement;
- Maintain records: keep detailed records of remote healthcare sessions, including patient consent, service documentation, and clinical outcomes;
- Transparent billing: communicate with patients about potential costs associated with telemedicine and RPM services and what is covered by their insurance;
- Financial assistance: for services not covered by insurance, provide information on any available financial assistance programs or payment plans to ensure patients can access necessary care.
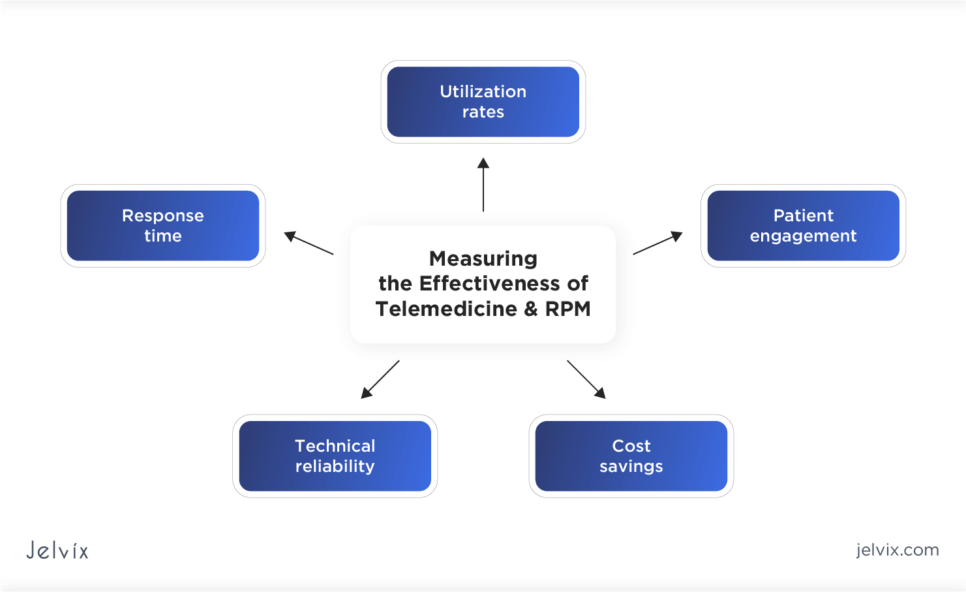
Measuring the Effectiveness of Telemedicine and RPM
Measuring the effectiveness of RPM and telemedicine solutions is essential for evaluating their impact on healthcare delivery and patient outcomes. Using Key Performance Indicators (KPIs), alongside assessing patient satisfaction and outcomes, provides a comprehensive understanding of their value:
- Utilization rates: track the frequency of use to check adoption levels among patients and physicians;
- Response time: measure the time taken to respond to patient queries or concerns via telemedicine platforms to indicate the efficiency of remote care delivery;
- Patient engagement: assess engagement levels by monitoring active users, session durations, and usage patterns of telemedicine and RPM tools;
- Technical reliability: monitor system uptime, error rates, and technical issues encountered, which affect the quality of service and user experience;
- Cost savings: analyze cost savings resulting from the use of telemedicine and RPM, such as reduced hospital readmissions, fewer emergency department visits, and decreased travel expenses for patients.
Patient Satisfaction and Outcome Measurement
Patient feedback provides valuable insights into the quality of healthcare services. By measuring patient satisfaction and outcomes, providers and vendors can identify areas that need improvement and take steps to enhance the quality of care they deliver:
- Surveys and feedback forms: implement regular surveys and feedback forms to collect patient perspectives on medical services, focusing on accessibility, ease of use, and satisfaction;
- Health outcomes: evaluate changes in patient health outcomes related to telemedicine and RPM interventions, such as improved management of chronic conditions, faster recovery times, and overall health improvements;
- Quality of life: assess the impact of your solutions on patients’ quality of life, including factors like mental health, physical activity levels, and independence;
- Adherence to treatment plans: measure patient adherence to prescribed treatment plans and medication intake;
- Patient retention and loyalty: track patient retention rates and loyalty as indicators of satisfaction and trust.
By monitoring these KPIs and metrics and gathering comprehensive patient feedback, providers and vendors can gain valuable insights into the effectiveness of their telemedicine and RPM tools.
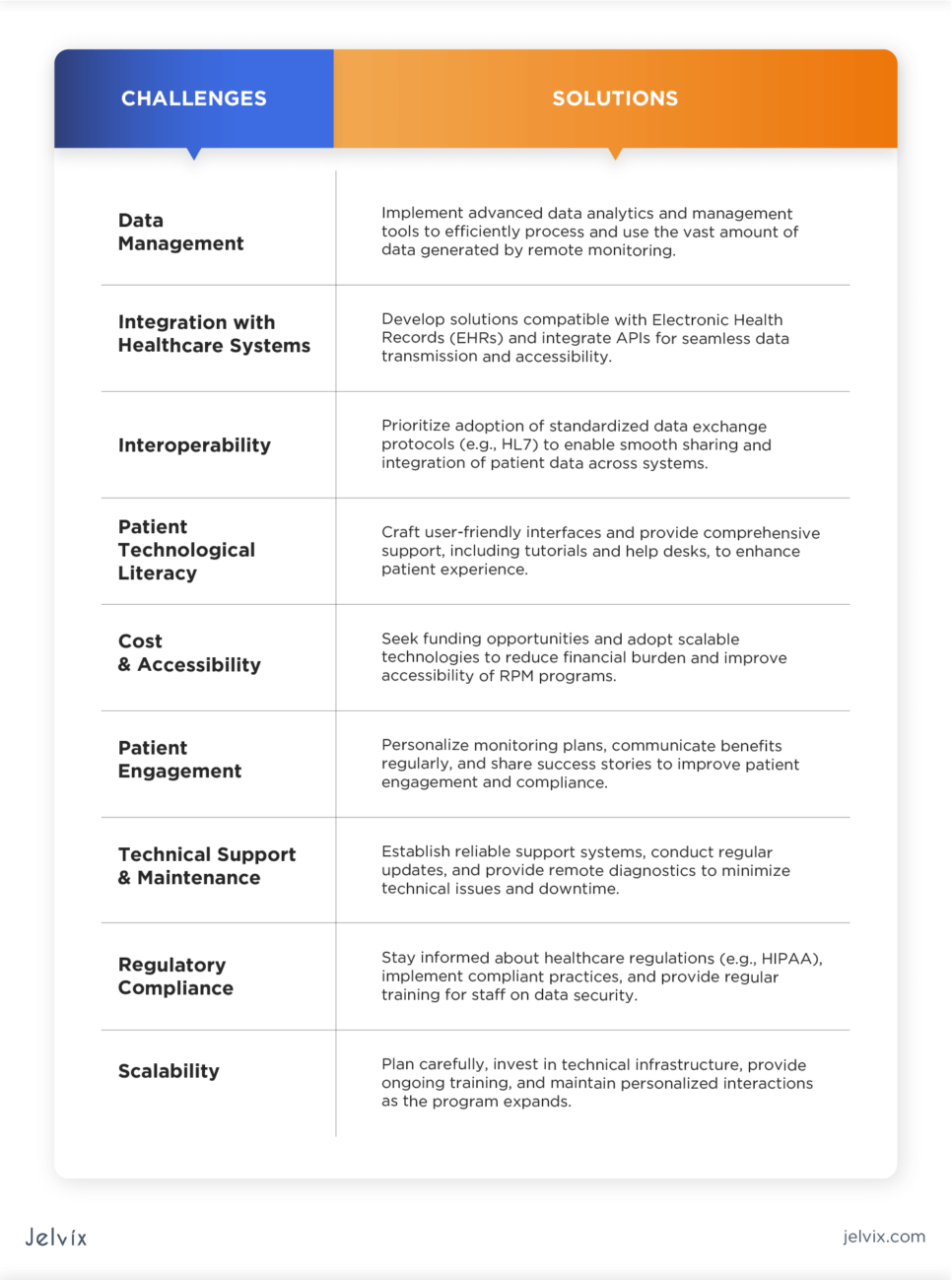
Challenges and Solutions in Telemedicine and RPM
Although integrating telemedicine and RPM solutions into healthcare settings brings numerous advantages that help streamline patient care, providers and vendors need to understand the associated challenges. Addressing them is needed to enhance the effectiveness of remote care and ensure data security and regulatory compliance.
Interoperability
Healthcare systems often use different EHR systems and devices, leading to interoperability challenges when trying to integrate data from multiple sources. Communicate the adoption of interoperability standards to facilitate seamless data exchange between RPM and EHR systems.
Data Security and Privacy
Telemedicine and RPM involve the exchange of sensitive patient information, and ensuring its security and privacy can be a significant challenge. Implement robust encryption and adhere to industry regulations to protect patient information.
Provider Workflow Integration
Implementing telemedicine and RPM into existing healthcare workflows requires changes to traditional care delivery processes. Healthcare providers and vendors can redesign workflows to incorporate telemedicine and RPM efficiently. Training and education for staff are crucial in this process.
Lack of Standardization
The lack of standardized protocols and guidelines for telemedicine and RPM can lead to lower care quality and limit the scalability of these technologies. Promote the development and adoption of standardized clinical protocols and guidelines for telemedicine and RPM to ensure consistent and evidence-based care.
Reimbursement and Regulation
Reimbursement policies and regulations for telemedicine and RPM services vary by location and can be complex, affecting the financial viability of these technologies. Advocate for policy changes that improve reimbursement for telemedicine and RPM, making them more accessible and financially viable for both patients and physicians.
Developing Solutions for Rural and Underserved Areas
Rural and underserved areas often lack sufficient healthcare facilities, including hospitals, clinics, and specialized care centers. As reported by Patient Engagement HIT, 100 million Americans lack access to primary care. Implementing telemedicine services to connect patients with physicians remotely can save the situation by bringing healthcare directly to underserved communities.
Learn how to implement remote patient monitoring in your practice.
Successful Telemedicine and RPM Programs: Case Studies
Real-world examples of remote patient monitoring tools provide practical insights into how telemedicine and RPM are implemented in healthcare settings. They showcase the actual challenges faced and solutions applied. Successful programs often reveal best practices that can be adopted by healthcare organizations.
Ochsner Health
Ochsner Health is a renowned healthcare entity in Louisiana, U.S., that effectively leveraged telemedicine to enhance patient care, especially during the COVID-19 pandemic. By expanding its telehealth services, addressing diverse patient needs, and advocating for supportive policies, Ochsner Health showed that telemedicine can be a valuable tool in delivering high-quality care to a broad patient population.
Cityblock Health
Cityblock Health leveraged complex care coordination through telehealth by implementing a comprehensive system that connects physicians and patients in underserved urban communities. They integrated virtual care solutions into their care model, enabling patients to receive timely care without the barriers of physical distance or transportation issues.
Massachusetts General Hospital
Mass General implemented telemedicine in the fields of neurology and stroke care, effectively launching their teleneurology and telestroke programs. These initiatives are aimed at providing timely and specialized medical consultations to patients who might not have immediate access to neurologists or stroke experts due to geographic limitations or time-sensitive conditions. The benefits are twofold: rapid access to expert care for patients in need and the ability to extend specialized medical services to underserved or remote areas.
Telehealth Solution With a RPM Module by Jelvix
The Jelvix team created a telehealth solution featuring remote monitoring via IoT technology so that patients could easily track their vital signs and share them with physicians. As a result, administrative tasks for the clinic’s staff were reduced by 25%, and unnecessary hospital visits for patients were cut by 30%, making healthcare more accessible.
The Future of Telemedicine and RPM
According to ReportLinker, the global RPM market size is expected to reach $175.2 billion by 2027. One of the key factors is the growing use of wearable device tech that is expected to result in telehealth and RPM tools becoming widely adopted.
What’s more, AI is seen as the global trend in RPM development. Statista reports that the market of AI in healthcare is projected to surpass $188 billion, allowing for more precise health monitoring and tailored treatment plans.
How a Tech Partner Can Leverage RPM Development
With expertise in healthcare software development, an experienced tech partner can help integrate RPM systems and telemedicine into established clinical workflows to enhance care delivery.
At Jelvix, we understand the complexities and challenges providers and vendors face in adopting new technologies. Our approach is centered on creating seamless, intuitive solutions that not only fit into existing clinical workflows but also improve them.
For more information on how Jelvix can support the development of healthcare solutions for your organization, contact our team for a consultation on your specific needs.
Looking for a technology partner?
Enhance your development capabilities with our dedicated team of seasoned professionals.