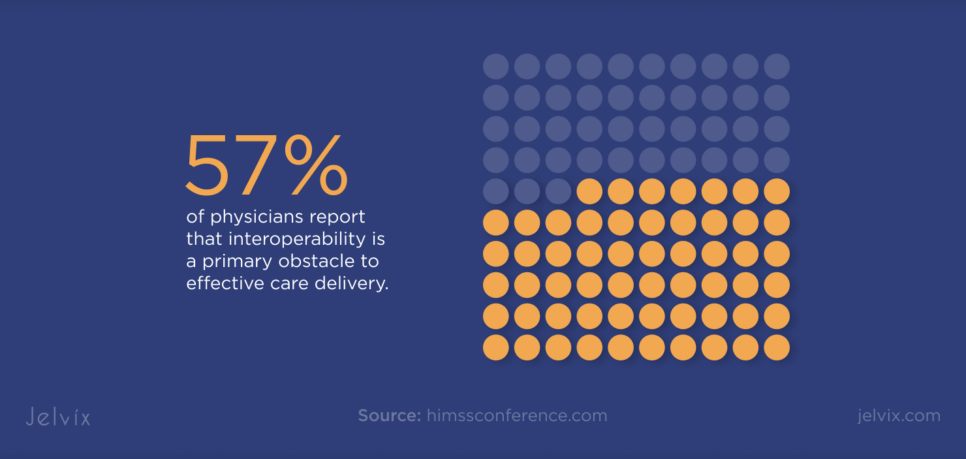
Healthcare providers face mounting pressure to deliver connected and compliant care via telehealth platforms. At the same time, integrating different tools remains a critical challenge, and 57% of physicians report that interoperability is a primary obstacle to effective care delivery.
However, using data within a unified telehealth solution takes more than just APIs in healthcare. It demands a strategic patient data integration plan that meets compliance standards and enhances user experience.
If you aim to scale your healthcare business through seamless and secure medical data integration, read this guide. It will walk you through the telehealth and EHR integration best practices, helping you set everything up step by step.
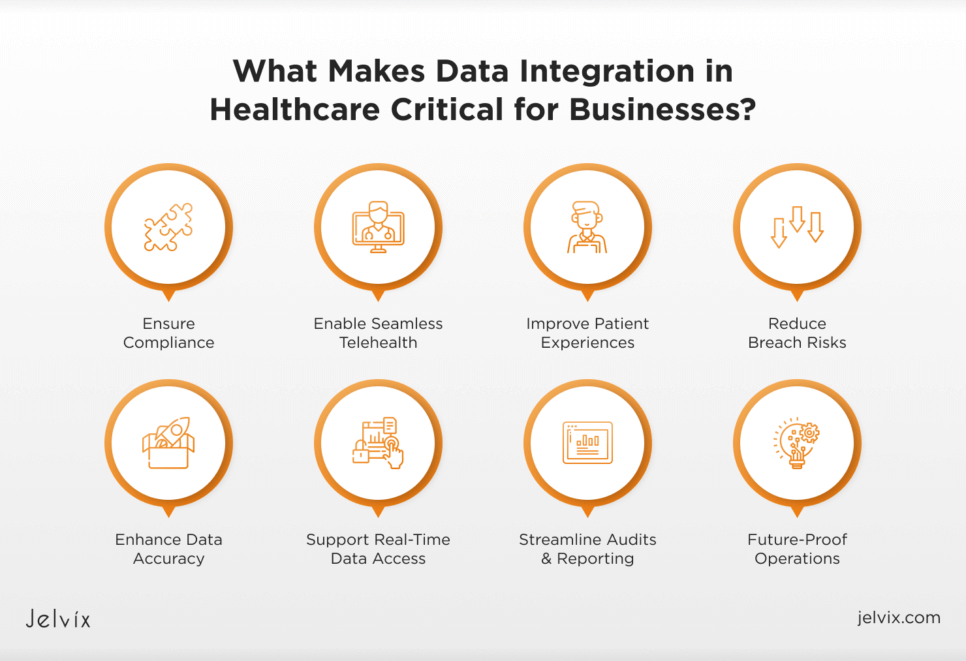
What Makes Data Integration in Healthcare Critical for Businesses?
Disconnected systems create risks for both compliance and patient experience. As regulations tighten and virtual care becomes the new norm, seamless integration and interoperability in healthcare are no longer optional.
Compliance Comes First
Data privacy laws like HIPAA and GDPR require secure and auditable handling of patient information. In the U.S., over 167 million healthcare records were compromised by cyberattacks in 2023, a 264% increase in ransomware incidents. Connected systems help ensure data accuracy and simplify audits, reducing the risk of costly breaches.
Patients Expect More
Telehealth remains widely accepted, with 94% of patients who used virtual care in 2024 saying they would use it again. When systems do not communicate, patients face repeated questions and inconsistent care. On the other hand, healthcare data interoperability gives providers a real-time view of patient history, enabling smoother and more personalized experiences.
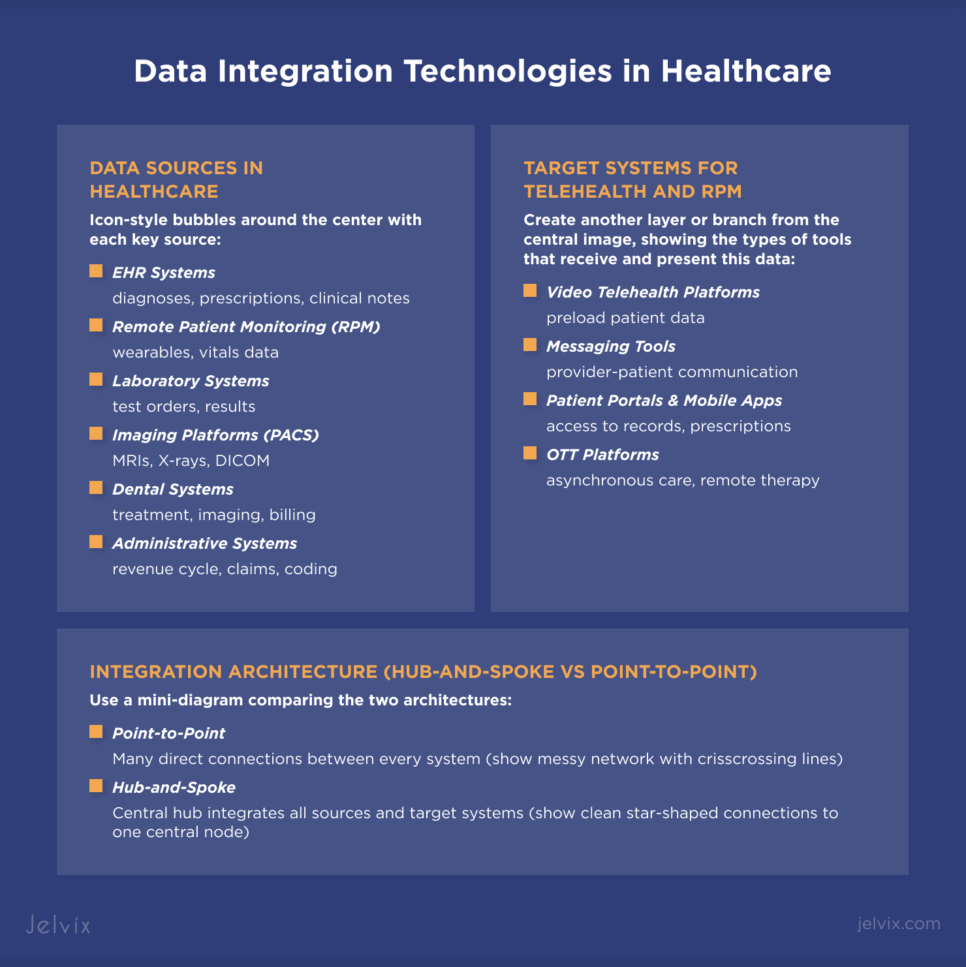
Data Integration Technologies: An Overview of Key-Systems and Architecture
Healthcare platforms often rely on numerous disconnected tools, each with distinct formats, rules, and workflows. Choosing the right architecture will help you simplify the process of healthcare data migration and reduce the likelihood of disconnected care.
Types of Data Sources in Healthcare
In any healthcare environment, patient data is scattered across multiple systems. An integrated EHR is typically the central hub, containing diagnoses, prescriptions, and clinical notes.
Remote patient monitoring telehealth tools collect real-time vitals from devices like wearables and glucose meters, providing insight into the patient’s condition between visits. Laboratory systems manage test orders and results, which must be synchronized with the patient record for timely review.
Imaging platforms, such as PACS, store and deliver high-resolution scans, including MRIs and X-rays, often using specialized formats like DICOM. Dental clinics use similar tools to manage treatment charts, imaging, and billing workflows.
On the administrative side, revenue cycle systems process claims and coding and must stay in sync with clinical data to avoid billing errors.
Target Systems in Telehealth and Remote Patient Monitoring
The goal of telehealth EHR integration is to bring this data into the tools used during virtual care. Live video platforms must preload relevant patient data to facilitate smooth and informed consultations.
Messaging tools rely on access to history and test results, enabling providers to respond accurately, even outside scheduled visits.
Patient portals and mobile apps provide users with access to their medical records, prescriptions, and follow-up instructions. For the experience to feel seamless, data must be updated in real-time and be available across devices.
Finally, OTT platforms take it a step further, offering asynchronous care, remote therapy, and personalized health content, all of which rely on accurate and timely data.
Designing the Right Architecture: Hub-and-Spoke vs Point-to-Point
Point-to-point architecture connects each system directly to every other system it needs to communicate with. This method can work in small-scale environments with only a few tools. However, adding a new system requires creating new connections, which can quickly become unmanageable.
Hub-and-spoke architecture introduces a central integration layer that connects to each system individually, handling translation, security, and data routing. Systems only need to communicate with the hub, making the hub-and-spoke architecture ideal for healthcare entities that are building scalable digital infrastructure and investing in medical software development.
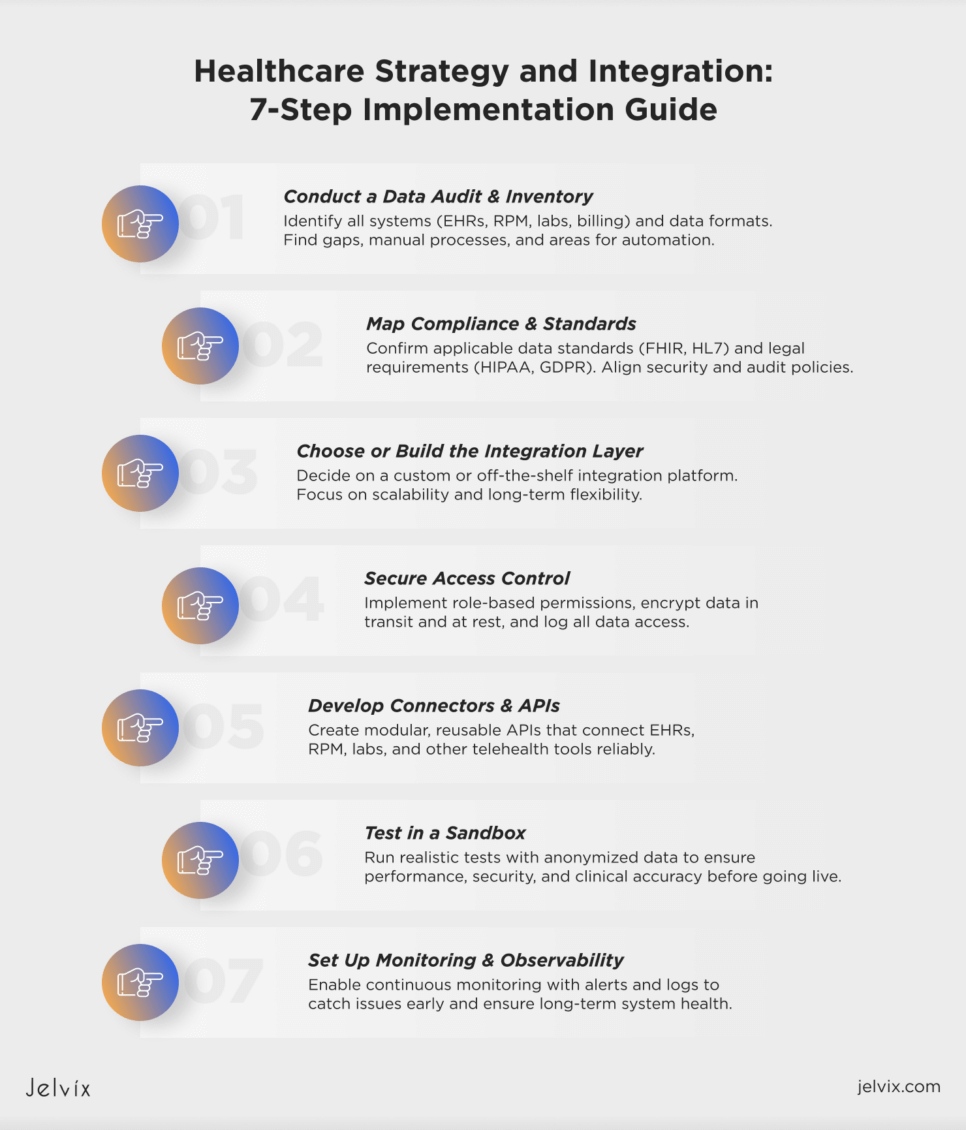
Healthcare Strategy and Integration Planning: A Step-by-Step Implementation Guide
Integrating healthcare data into a telehealth platform requires a structured, phased approach. The following steps outline the process of transitioning from disconnected systems to a reliable, secure, and compliant integration environment.
Step 1. Conduct a Data Audit and Inventory
Start by identifying all systems that produce or store patient data, including EHRs, remote patient monitoring telehealth tools, lab systems, and billing tools. List each system, note the type of data it holds, and document the format, such as HL7 v2, FHIR data model, or proprietary CSV files.
Also, assess how data flows between platforms and identify gaps, redundancies, and areas where manual workarounds are in place to clarify what needs to be automated.
Learn how FHIR standards improve interoperability, streamline data exchange, and support scalable digital health solutions.
Step 2. Map Compliance Requirements and Data Exchange Standards in Healthcare
Determine which healthcare data standards and laws apply based on your location and services. Most clinical integrations will involve the use of FHIR or HL7 standards. Map out your HIPAA, GDPR, or regional compliance obligations to guide access rules, audit logging, and retention policies.
Step 3. Choose or Build Your Integration Layer
Decide whether to use an off-the-shelf integration platform or build custom enterprise solutions. Consider cost, timeline, system complexity, and long-term scalability. The right solution should support your healthcare-specific needs and be flexible enough to adapt as your tech stack evolves.
Step 4. Secure Access Control
Set up role-based access so that users only see the data they are authorized to view. Don’t forget about encryption at rest and in transit, and implement authentication at the API level. Make sure all access is logged and auditable to meet compliance standards.
Step 5. Develop Connectors and APIs in Healthcare
Build the APIs and connectors that link your systems. Common examples include syncing EHRs with telehealth platforms or feeding RPM data into care dashboards.
Keep connectors modular and reusable to support long-term maintainability and ensure that updates or changes in one system don’t break the entire workflow.
Step 6. Test in a Sandbox Environment
Before going live, set up a sandbox that mirrors your production environment. Use realistic but anonymized data to simulate how each integration will behave in real-world scenarios. Run tests for data syncing, access control, error handling, and performance under load, and validate that the data flows make sense clinically and operationally.
Step 7. Set Up Monitoring and Observability
Once the system is deployed, set up logging and alerts to detect failed connections, permission issues, or performance slowdowns. Use dashboards, logs, and alerts to detect issues early and track the long-term health of your system.
Telehealth EHR Integration: Real-World Use Cases
Every healthcare provider faces unique challenges when integrating data systems, depending on their size, structure, and services. Below are three examples that show how different types of organizations can apply integration strategies in practice.
Discover how API integration improves patient care, eliminates silos, and accelerates innovation across your tech stack.
Small Clinic Performing EMR Data Integration to Zoom
A small clinic offering remote visits struggled with manual workflows because their EHR didn’t support video. Staff had to copy data and send links separately.
To streamline this process, they developed a simple middleware that connects the EHR to Zoom via API. It automatically generates secure links, updates the patient record, and logs the session. As a result, remote visits became easier to manage and just as structured as in-person care.
Hospital Network Centralizing Patient Data to Feed Into Telemedicine App
A hospital group operating multiple facilities sought to integrate patient data into a unified telemedicine application. However, differences in EHRs and lab systems led to delays and inconsistencies.
They implemented a hub-and-spoke integration engine that pulls data from local systems, standardizes it using FHIR, and delivers it to the app. Now, patients experience consistency across facilities, and providers have access to complete data during virtual visits.
RPM Telehealth Vendor Integrating With Third-Party Telehealth APIs
A remote monitoring startup needed to send real-time vitals into each clinic’s telehealth system, but every partner used a different platform.
They built a flexible API gateway that routes data in the required format for each partner, whether via FHIR, webhooks, or SDKs. This enabled seamless integration with multiple systems, allowing clinics to view live patient data without altering their workflows.
Risk Minimization Framework for Your Medical Software Integration
Integrating healthcare systems brings security, technical, and legal risks. Without the proper safeguards, organizations can face data breaches, system failures, and compliance violations. This framework outlines how to minimize those risks effectively.
Data Breach Scenarios and Mitigations
Breaches often result from weak authentication, misconfigured APIs, or poor access controls. To reduce risk, organizations must use encryption, restrict access based on roles, and log all system activity. Regular audits and security testing help uncover vulnerabilities before they cause damage.
Fault Tolerance and Recovery Planning
Outages can disrupt care and erode trust. Building redundancy into key systems and automating backups is essential. Recovery plans should include clear response procedures and monitoring tools to catch issues early.
Third-Party Vendor Risk Checklist
External vendors introduce security and compliance risks. Each partner should be reviewed for certifications, data handling practices, and breach history. Ongoing monitoring and reevaluation ensure that vendor performance and security stay aligned with the standards of data governance in healthcare.
Legal Safeguards
Strong legal agreements help define responsibility and reduce liability. BAAs, DPAs, and SLAs should clearly outline how data is handled, who has access, and what happens in the event of an error or incident. These documents protect both operational integrity and compliance.
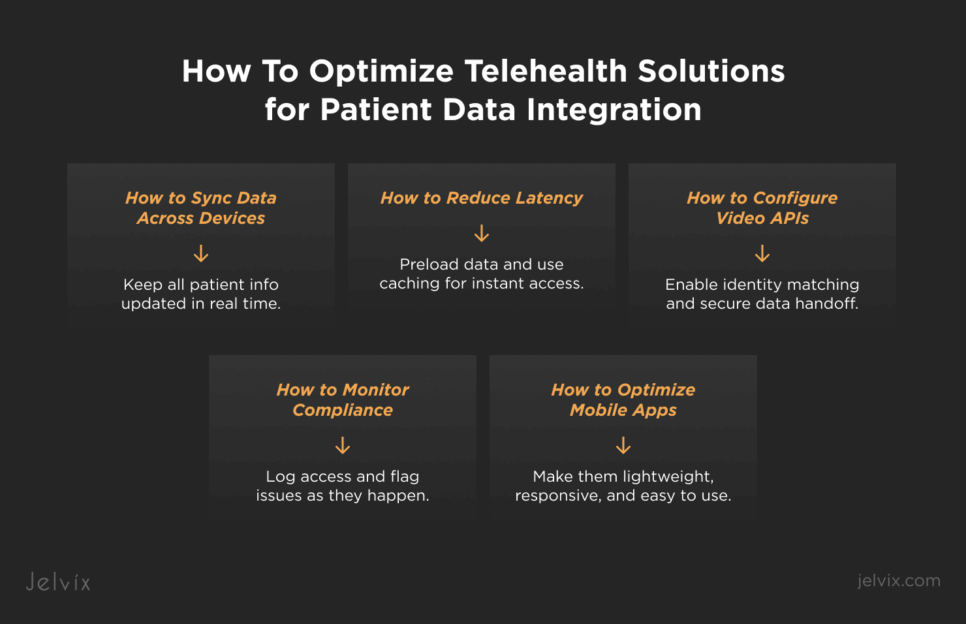
Optimizing Telehealth Solutions for Patient Data Integration Workflows
Once systems are connected, the next challenge is ensuring that the integrated data supports fast, smooth, and reliable telehealth experiences. This involves more than just syncing records; it requires tuning performance, security, and usability across all channels.
Reducing Latency in Data-Driven Video Sessions
When clinical data is shared during a live video session, delays can disrupt communication and reduce care quality. To minimize latency, patient data should be preloaded before the session begins. Caching strategies and optimized database queries can help ensure that lab results, medications, and care notes are available instantly during a visit.
Efficient Data Synchronization for Multi-Device Access
Patients and providers often switch between various devices, including laptops, tablets, and phones. Synchronization must occur in real-time, with consistent data presented across every touchpoint. Using background sync and lightweight API calls helps maintain performance without draining device resources.
Video API Configuration for EHR-Integrated Platforms
Embedding video functionality inside EHR workflows requires careful configuration. Video APIs must support identity matching, session tracking, and secure handoff of visit data to the patient record. This helps providers stay within one system while still accessing all video features and clinical data during the call.
Real-Time Compliance Monitoring
As data moves between systems, compliance cannot be an afterthought. Real-time logging and alerts should track access attempts, data transfers, and unusual patterns. When compliance is monitored continuously, issues can be flagged early and addressed before they lead to violations.
Mobile Optimization for Patient-Facing Telehealth Apps
Most patients access RPM telehealth functionality through mobile devices. Apps must be responsive, lightweight, and designed for varying connectivity levels. Streamlined login, simplified data views, and clear error handling are essential for making telehealth services usable and trustworthy on mobile devices.
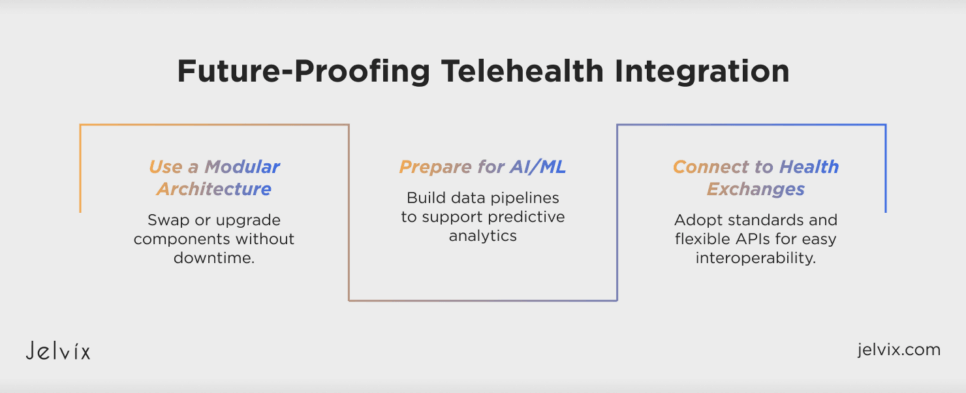
Future-Proofing Your Telehealth Integration
As healthcare technology continues to evolve, integration strategies must remain flexible. Building for today is not enough. To avoid expensive rebuilds or compliance gaps down the road, it’s important to design systems that can adapt to new tools, policies, and use cases.
Making Your Stack Modular for Upgrades
A modular architecture allows teams to replace or upgrade specific components without affecting the entire system. This is especially useful as vendors update APIs, sunset features, or change pricing models. By separating concerns, such as identity management, video services, and patient data sync, organizations can maintain data integration and interoperability with minimal disruption.
Planning for AI/ML and Predictive Analytics Integration
Healthcare organizations are increasingly adopting AI for decision support, risk scoring, and patient engagement. Future-ready systems should include clean, well-structured data pipelines that can feed into AI/ML models. Whether used for predictive diagnostics or care coordination, these tools require real-time access to diverse and accurate data sources.
Interfacing with National Health Exchanges
Regulations like TEFCA in the U.S. and similar health information exchange initiatives globally are creating new expectations around data sharing. Integrating with national exchanges allows providers to access external patient histories, referrals, and care team communications.
Clinics must develop systems with open standards, consent management, and flexible APIs to support this kind of integration and interoperability in healthcare.
Ensuring Seamless Health Data Integration with a Trusted Tech Partner
Integrating patient data into telehealth platforms is essential for delivering connected, compliant, and high-quality care. From EHRs and RPM devices to lab systems and mobile applications, each component must work together in real-time.
If you need to develop a telehealth solution or integrate an existing system, Jelvix is here to help. We design secure, scalable, and integration-ready solutions for healthcare providers worldwide. Reach out to our experts to find out how we can support your telehealth strategy.
FAQ
What is the most secure way to integrate patient data into a telehealth platform?
Use encrypted APIs, role-based access controls, and audit logging. Also, encrypt data in transit and at rest, and follow compliance frameworks like HIPAA or GDPR. Secure authentication and regular security testing are essential for minimizing breach risks.
How do I choose between building a custom integration layer and using an iPaaS solution?
Choose based on complexity, timeline, and in-house expertise. iPaaS offers faster deployment and built-in connectors, ideal for standard use cases. Custom middleware allows greater flexibility and control for specialized workflows or legacy systems but requires more resources to maintain.
Which standards of data governance in healthcare should my organization prioritize?
Prioritize FHIR for modern, API-driven applications. HL7 v2 remains prevalent in legacy EHR systems, but FHIR is better suited for mobile apps, patient portals, and real-time exchange. Your choice depends on the systems you’re integrating and future scalability needs.
What kind of architecture is best for scaling integrated telehealth systems: hub-and-spoke or point-to-point?
The hub-and-spoke architecture scales better. It centralizes data flow, reduces redundancy, and simplifies system management. Point-to-point works for small setups but can be complex to run when the number of connections grows.
How can I test and validate integration before full deployment?
The first step is to run a sandbox environment to mirror your production setup. Use simulated scenarios with anonymized data to test API performance, error handling, and data accuracy. Validate user permissions, logging, and response times under typical and high-load conditions.
Need a Reliable Tech Partner?
Team up with integration experts who turn disconnected systems into seamless digital workflows.