As healthcare data volume grows, medical entities face challenges in managing this information efficiently, primarily due to a lack of interoperability. To tackle this issue, 73% of healthcare companies turn to standard-based APIs to expand the functionality of their existing EHR systems.
If you’re looking to facilitate seamless data integration, improve system interoperability, and benefit from the full potential of your healthcare data with the help of an API, read this article. You’ll find out what types of APIs exist, their benefits, challenges, and steps to choose a solution that suits your entity’s needs best.
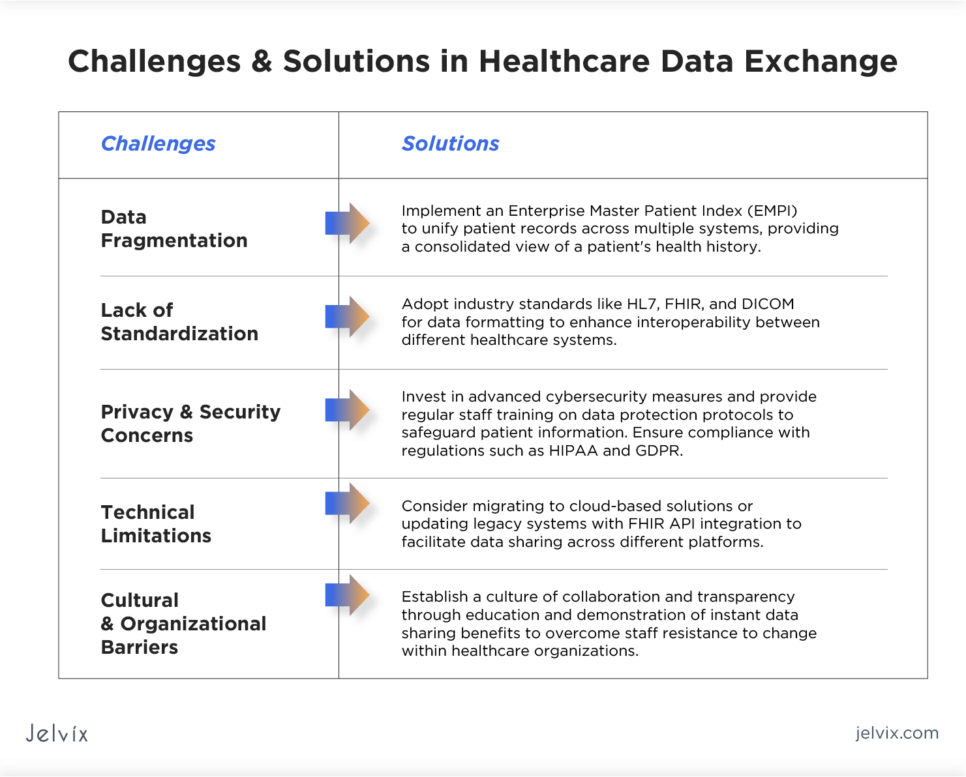
Common Challenges in Healthcare Data Exchange
Healthcare data exchange is full of obstacles that limit seamless data sharing and integration. Addressing these challenges requires a multi-faceted approach that includes the adoption of data exchange standards like HL7 and FHIR, investing in modernizing IT infrastructure, and ensuring data security measures.
Data Fragmentation
Healthcare data is often scattered across various systems and repositories, such as EHRs, lab information systems, and pharmacy management systems. This fragmentation makes it difficult to view a full patient’s health history, leading to incomplete information that can affect treatment decisions. Implementing an Enterprise Master Patient Index (EMPI) can help unify patient records across multiple systems, providing a consolidated view of a patient’s health history.
Lack of Standardization
The absence of universally adopted standards for data exchange limits the possibilities of medical teams to interpret and use data from different sources effectively. Adopting industry standards like HL7, FHIR, and DICOM for data formatting can enhance interoperability between different healthcare systems.
Privacy and Security Concerns
Compliance with regulations such as HIPAA in the U.S. and GDPR in the EU adds a layer of complexity to the data exchange process. Healthcare organizations must strictly follow these regulations to protect sensitive patient information against breaches and cyber-attacks. Investing in advanced cybersecurity measures and regular staff training on data protection protocols will help safeguard patient information, too.
Technical Limitations
Many healthcare entities keep using legacy systems that were not designed with interoperability in mind. Upgrading or replacing these systems can be costly and time-consuming. Migrating to cloud-based solutions or updating legacy systems with FHIR API integration can be a good idea to facilitate data sharing across different platforms.
Cultural and Organizational Barriers
Resistance to change within healthcare organizations can compromise the adoption of new technologies and processes required for effective data exchange. Establishing a culture of collaboration and transparency through education and demonstration of instant data sharing benefits can help overcome staff resistance.
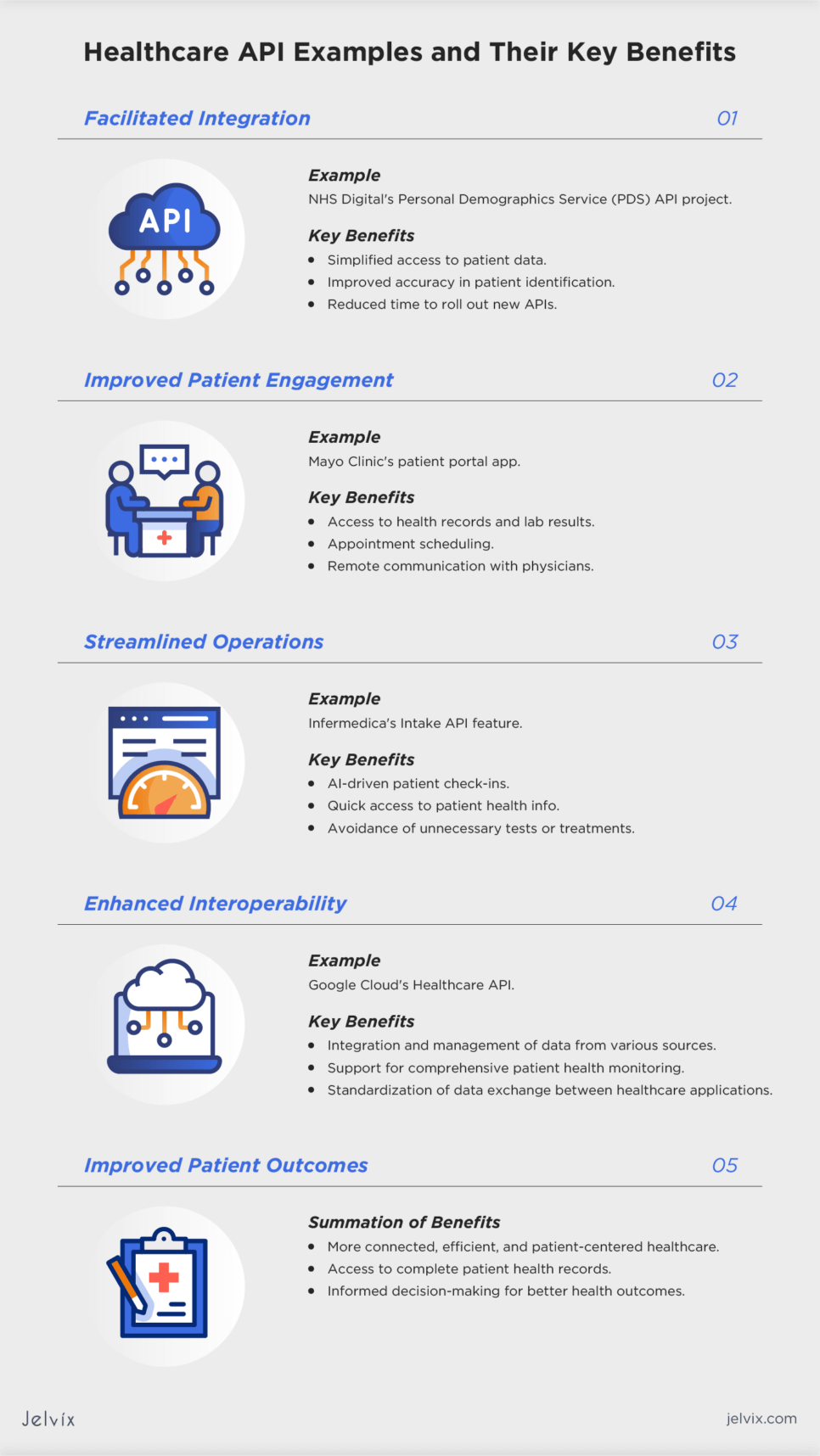
Healthcare API Examples and Their Key Benefits
As mentioned earlier, about two-thirds of healthcare companies use APIs to expand their system’s capabilities. It’s no wonder, as API integration brings in several benefits that help streamline operations, enhance patient care, and move toward innovation.
Facilitated Integration
The Personal Demographics Service (PDS) API project at NHS Digital transformed how healthcare teams accessed and used patient data. By switching from a SOAP to a modern API management platform, the team made it simpler for developers to integrate NHS services, improving the accuracy of patient identification and communication. This change slashed the time to roll out new APIs from a year to just a few months.
Improved Patient Engagement
APIs enable the development of mHealth apps and patient portals that offer access to health records, appointment scheduling, and remote communication with physicians. The Mayo Clinic used an API to develop an app that provides patients access to their medical records, lab results, and other health-related info, enhancing overall patient engagement.
Streamlined Operations
Infermedica made visiting a doctor easier by expanding its API with Intake – a new feature that uses AI to make patient check-ins smooth and quick. Thanks to this API enhancement, physicians can see a patient’s health info right away and avoid unnecessary tests or treatments.
Enhanced Interoperability
APIs help standardize data exchange between healthcare applications and solutions. In particular, Google Cloud’s Healthcare API, which is in use by Mayo Clinic, enables healthcare organizations to integrate and manage data from a variety of sources, including EHRs, Google Fit, and other IoT devices, supporting a comprehensive approach to patient health.
Improved Patient Outcomes
Summing up the benefits listed above, APIs can significantly improve patient outcomes by supporting a more connected, efficient, and patient-centered healthcare ecosystem. Better interoperability between various medical systems ensures that physicians have access to a patient’s complete health record, allowing for informed decision-making. At the same time, APIs allow physicians to analyze vast amounts of patient data, enabling them to derive actionable insights to guide interventions that improve health outcomes.
APIs and Microservices
In healthcare, the concepts of APIs and microservices often intersect, yet they serve distinct roles in how applications are built, deployed, and integrated. Understanding the differences between both is needed for using medical technology effectively.
The Concept of APIs
APIs act as the communication layer that allows different software applications to interact with each other. They define the rules and protocols for how software components share data and functionalities. APIs enable EHRs, patient management platforms, and diagnostic tools to exchange data seamlessly and securely over a network, allowing remote access to medical services.
The Concept of Microservices
Microservices represent an architectural style that structures an application as a set of coupled services. Each service in this architecture is built around a specific business function and can be developed, deployed, and scaled independently. This approach offers flexibility, scalability, and the ability to use different technologies for different services.
For instance, a healthcare app built using microservices might have a microservice for handling lab results. This microservice would expose an API that other parts of the application can use to access and display a patient’s lab results.
Together, APIs and microservices enable healthcare organizations to create sophisticated and patient-centered applications that can adapt to changes in the medical industry.
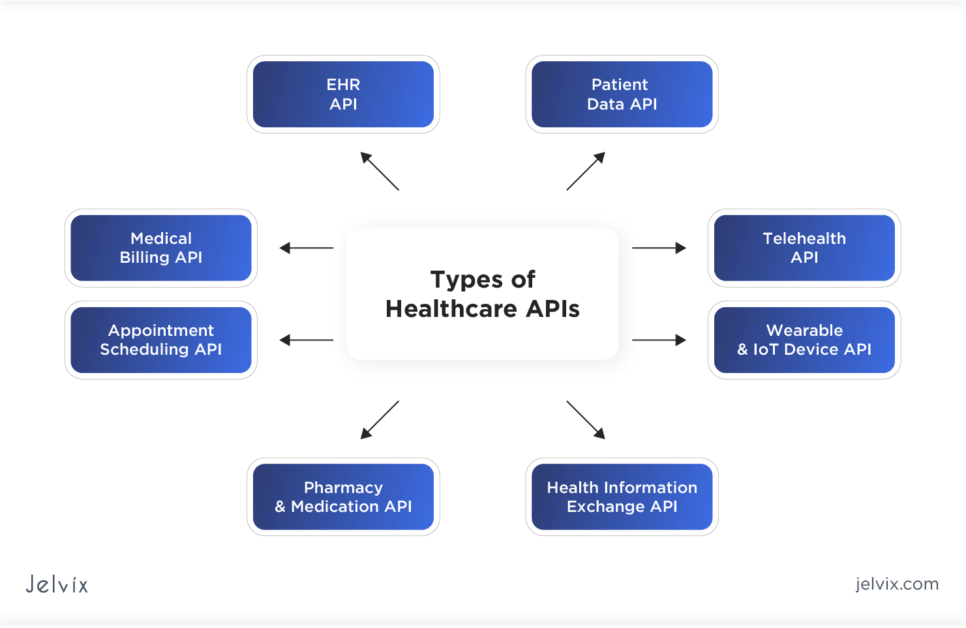
Types of Healthcare APIs
Since APIs facilitate the exchange of data in disparate healthcare settings, they find a vast amount of applications in the sector.
EHR API
EHR APIs allow for the integration of third-party applications with electronic health record systems. Physicians can access and update patient records from different EHR systems, supporting better care coordination and patient data management. For instance, Epic’s FHIR-based APIs allow developers to create apps that can access and interact with the Epic EHR system.
Patient Data API
These APIs focus on sharing patient-specific information, such as medical history, lab results, and medication lists, among healthcare providers, patients, and authorized third parties. They support patient-centered care by making personal health information accessible and manageable through patient portals and health apps.
Medical Billing API
Payment and billing APIs enhance the processing of healthcare payments and insurance claims. They can automate billing workflows, verify insurance eligibility, and facilitate secure payment transactions between patients, providers, and insurers, reducing administrative burdens on medical staff and improving financial operations.
Appointment Scheduling API
These APIs simplify the appointment booking process by integrating scheduling systems across different healthcare platforms. Patients can book, reschedule, or cancel appointments using their preferred digital channels which enhances convenience and reduces no-show rates.
Telehealth API
Telehealth APIs enable the integration of video consultations, messaging, and remote monitoring tools into healthcare applications, expanding access to care and facilitating remote patient visits.
Wearable and IoT Device API
These APIs connect wearable devices and other IoT sensors with healthcare applications. They allow for the real-time collection and analysis of patient data, such as activity levels, heart rate, and blood glucose levels, supporting proactive health management and personalized care plans.
Pharmacy and Medication API
Pharmacy and medication APIs facilitate the electronic prescribing of medications, tracking of treatment adherence, and integration of pharmacy services. They help organize medication management, improve prescription accuracy, and enhance patient safety.
Health Information Exchange API
HIE APIs support the secure exchange of healthcare information across different medical systems. They play a key role in enabling clinical interoperability, ensuring that patient data is accessible when needed for informed care decisions.
The Role of Healthcare API in Enabling Clinical Interoperability
As noted earlier, APIs facilitate the seamless exchange of data between different healthcare systems. By acting as bridges that allow diverse systems to communicate, APIs break down information silos and ensure that healthcare teams have timely access to comprehensive patient data.
This interoperability enhances patient care by enabling informed clinical decisions, streamlining workflows, and promoting patient engagement through direct access to their health information. What’s more, APIs drive innovation by enabling the development of new healthcare applications with interoperability in mind.
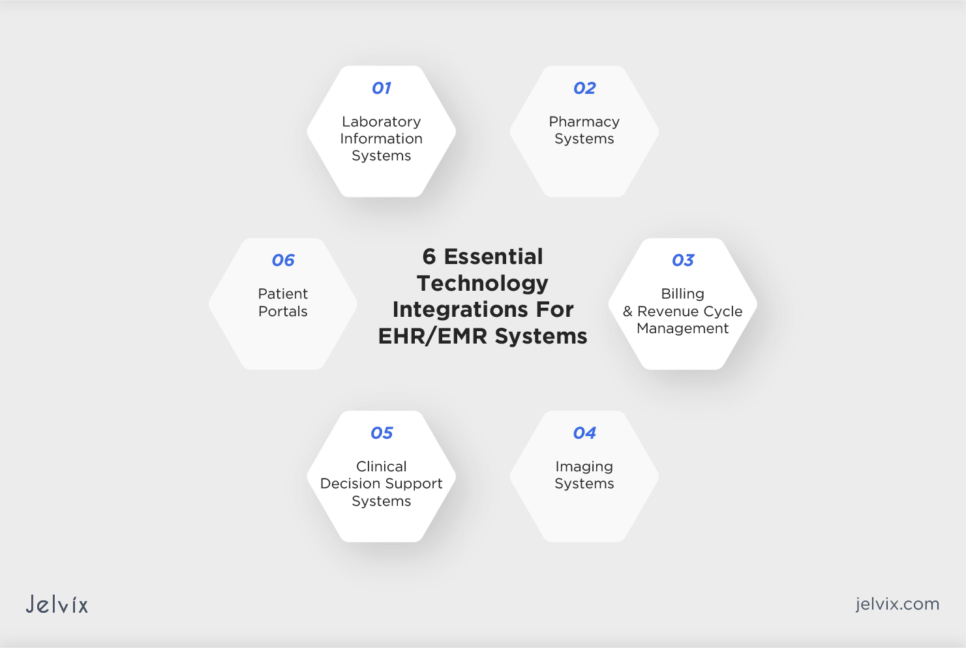
Essential EHR/EMR Integrations To Consider
About 96% of U.S. hospitals use EHR systems in their settings. Integrating these EHRs and Electronic Medical Record (EMR) systems with other healthcare applications and services through APIs can significantly enhance clinical workflows, patient care, and operational efficiency.
Laboratory Information Systems
Integrating EHR/EMR systems with LIS allows for automatically transferring laboratory test orders and results between clinicians and the lab. This can enhance the ordering process, reduce manual data entry errors, and ensure that providers have timely access to lab results for quicker diagnosis and treatment planning.
Pharmacy Systems
EHR/EMR integration with pharmacy systems facilitates e-prescribing, where doctors can send prescriptions directly to pharmacies. This improves prescription accuracy, enhances medication management, and increases patient convenience.
Imaging Systems
Integrating Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS) with EHRs enables the seamless access and sharing of imaging studies and reports. Physicians can view images alongside other patient data within the EHR, supporting informed clinical decisions.
Billing and Revenue Cycle Management
Integration of EHR/EMR systems with billing and revenue cycle management software automates the capture of billable services directly from the patient record. This ensures accurate billing, reduces claim denials, and optimizes revenue cycle processes.
Patient Portals
Linking EHR/EMR systems with patient portals equips patients with online access to their health information, supporting patient engagement, encouraging proactive health management, and improving health outcomes.
Clinical Decision Support Systems
EHR/EMR integration with CDSS enables patient data to provide evidence-based recommendations and alerts to healthcare professionals. This aids in diagnosis, medication dosing, and identifying potential adverse events.
Note, however, that implementing these integrations requires careful planning, technical expertise, robust data security measures, and compliance with healthcare regulations.
9 Steps To Choose the Right Healthcare API for Your Company
Choosing the right API for your clinic involves a systematic approach to ensure the solution can enhance your operational efficiency and improve patient care. By following a step-by-step approach you can select a healthcare API that not only meets your current needs but also supports future growth.
1. Understand Your Clinic’s Needs
Start with assessing your clinic’s specific needs. Identify areas where API integration can improve patient care or enhance data management. Clear objectives will help determine the functionalities you need from an API.
2. Look for Real-World Use Cases
Research how other clinics or healthcare providers implemented the API. Real-world examples can provide insights into the API’s practical benefits, challenges encountered during integration, and impact on healthcare delivery.
3. Prioritize Interoperability
Choose APIs that promote interoperability with existing systems like EHRs, practice management software, and patient portals. Look for APIs that adhere to healthcare data exchange standards, such as HL7 and FHIR, to ensure seamless communication between healthcare systems.
4. Evaluate Security and Compliance
Prioritize APIs that offer robust security features and comply with relevant healthcare regulations to safeguard sensitive medical data. Encryption, authentication, and audit trails will help protect patient information and ensure privacy.
5. Assess Scalability and Performance
Ensure the API can handle your clinic’s current and future data volumes. Consider the API’s reliability and response times, as these factors directly affect operational efficiency.
6. Review Documentation and Seek Support
Comprehensive API documentation is critical for smooth integration and troubleshooting. Ensure the API documentation is comprehensive, clear, and accessible. Also, consider the level of provided developer support, including community forums, technical support, and resources for developers.
7. Consider Flexibility and Customization
The API should offer flexibility to customize functionalities according to your clinic’s requirements. Customization capabilities will allow you to tailor the API integration to fit your workflows and enhance overall productivity.
8. Understand Pricing and Licensing
Review the pricing structure for using an API, including subscription fees, usage-based charges, or additional costs for premium features. Make sure you understand the licensing terms, and that they align with your clinic’s operational model and usage expectations.
9. Test Through Demos
Use a trial or demo version of the API to evaluate its functionalities, ease of integration, and compatibility with your systems. Hands-on testing can reveal potential issues and help you make an informed decision.
Discover strategies to increase return on software investment through EHR, empowering your business to achieve heightened financial gains.
How To Integrate a Health App with Epic EHR/EMR
About 285 million patients worldwide have medical data stored within Epic’s cloud-based EHR system. Successfully integrating your systems with Epic offers access to a vast pool of patient data and aligns health apps with the workflows of major healthcare providers.
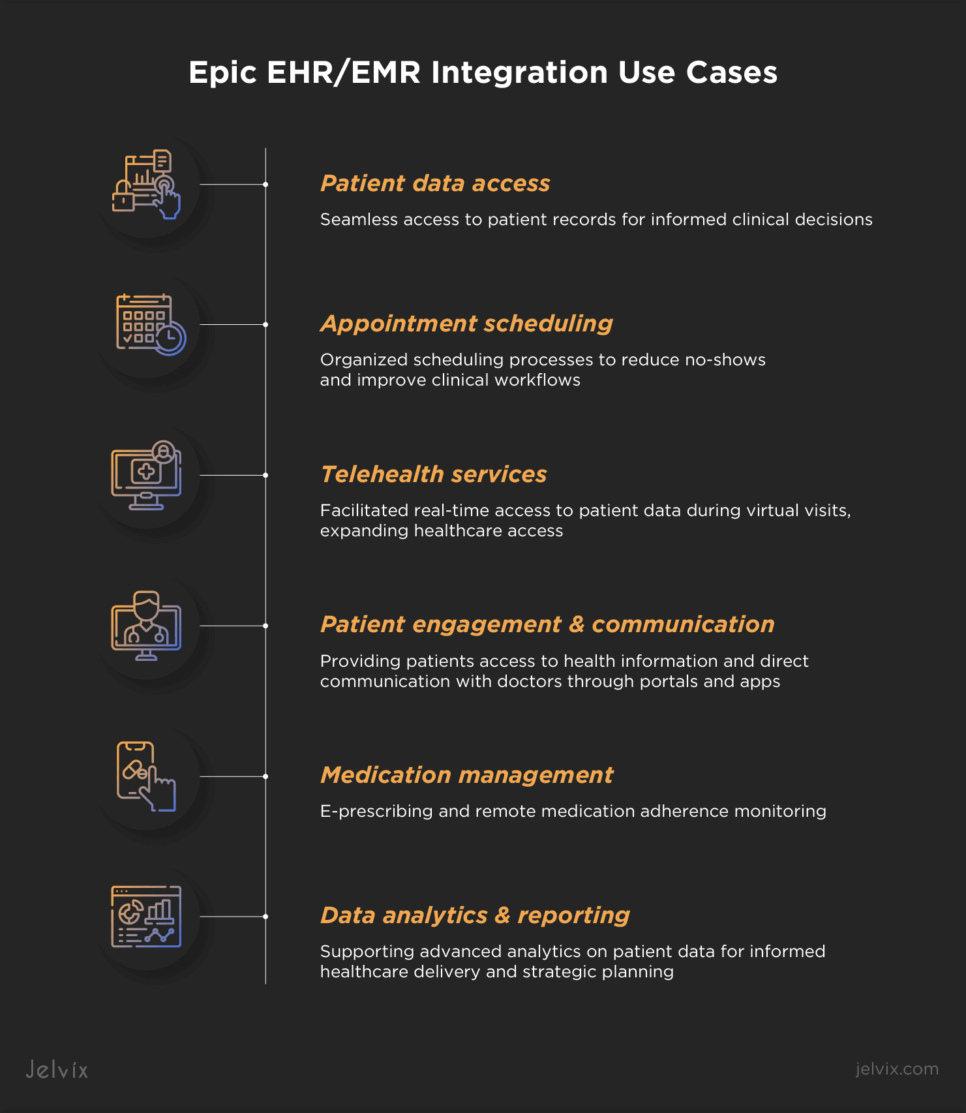
Integrating Epic’s API into healthcare applications can transform patient care and operational efficiency. The specific use cases can highlight the potential of such integrations:
- Patient data access: EPIC API enables seamless access to patient records for informed clinical decisions;
- Appointment scheduling: it organizes scheduling processes, reducing no-shows and improving clinical workflows;
- Telehealth services: it facilitates real-time access to patient data during virtual visits, expanding healthcare access;
- Patient engagement and communication: it offers patients access to their health information and provides direct communication with doctors through patient portals and apps;
- Medication management: Epic API allows for e-prescribing and medication adherence monitoring remotely;
- Data analytics and reporting: it supports advanced analytics on collected patient data to inform healthcare delivery and strategic planning.
Integrating Epic Healthcare API with an App: Key Considerations
Integrating a health app with Epic’s USCDI API is a strategic move that allows for enhancing healthcare delivery by ensuring seamless data exchange between your app and Epic’s EHR/EMR system. If you decide to integrate your mHealth app with Epic’s USCDI API, consider following the process described below.
Check Epic’s Support
Verify if Epic supports the sites from which you plan to extract data. Reach out to your account or integration manager at Epic to ensure the healthcare sites you’re targeting are supported by Epic’s system.
Create an Account with Epic
To access the API key necessary for integration, you’ll need to register at epic website. This step is essential for data protection as it verifies your identity, granting you the credentials needed to proceed with the integration.
Review the Available Data
Determine whether the API provides access to all the data your healthcare software needs, such as care plans, diagnosis reports, documentation, and patient history. Ensuring the API has the required endpoints is vital for the correct operation of your health app.
Get the Key
After registration, you’ll receive an API key. It’s important to test this key with the endpoints using REST clients to ensure they are functioning correctly and that your app can access the necessary data.
Integrate Epic API with Your App
Incorporate calls to the API within your app’s code, using the tested endpoints. Once everything is implemented and checked, your app will be fully integrated with Epic’s EHR/EMR, with access to the functionalities it offers.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

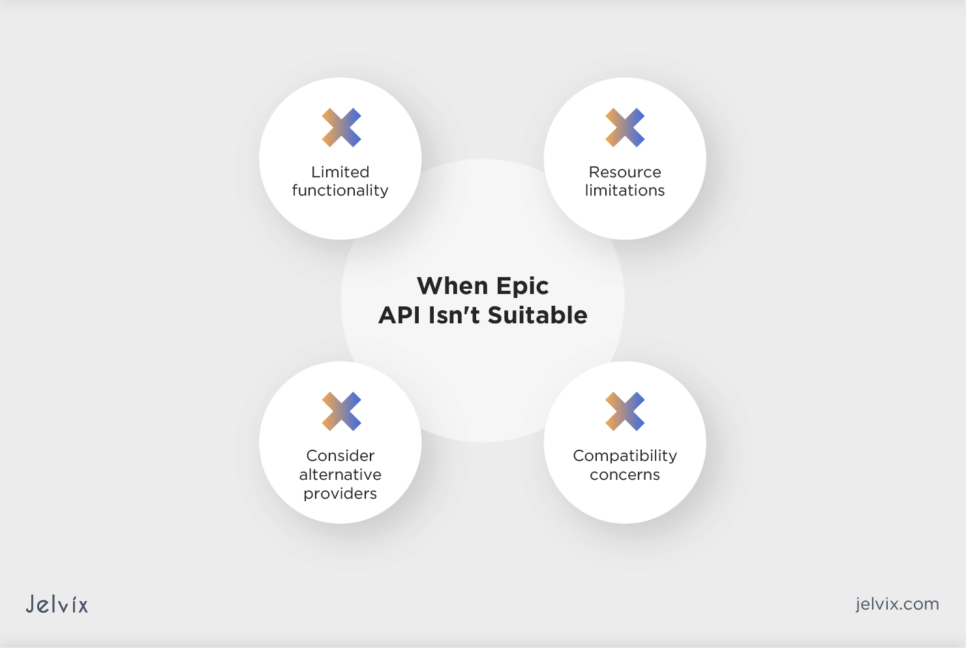
When Epic API Is Not a Good Fit
While Epic’s API facilitates access to a wealth of patient data and system functionalities, there are cases where it might not be the best fit:
- Limited scope of use: if your app needs are outside Epic’s API functionalities, it might not deliver the expected value;
- Resource constraints: the time, cost, and technical expertise required for Epic API integration may be challenging for smaller organizations or startups with tight budgets;
- Alternative systems: in areas where Epic’s EHR isn’t widely used, integrating with APIs from more prevalent EHR providers could be more useful;
- Compatibility and flexibility issues: apps requiring broad system compatibility or wider customization than Epic’s API allows may face limitations.
The Cost of Integrating EMR/EHR Healthcare API
The cost to integrate an EHR/EMR API can vary widely depending on the integration complexity, the type of accessed data, the level of customization, compliance requirements, and the API’s pricing model.
Integration costs can range from a few thousand dollars for basic access to patient data within smaller systems, to tens or even hundreds of thousands of dollars for comprehensive integration across multiple systems with customization and data analytics capabilities.
Pricing models for API integration influence its cost, too. For instance, subscription-based models require a fixed monthly or annual fee, offering predictability in budgeting. On the other hand, pay-per-use models charge based on the actual usage of the API, such as the number of requests made.
How Custom Healthcare Solutions Support API Integration
At Jelvix, we understand that every healthcare organization has unique needs. Our seasoned development team creates FHIR-supported custom solutions with flexible API integration capabilities, ensuring that whether you’re looking to integrate with EHRs, wearable devices, or telehealth platforms, the solution can fit your specific requirements.
If you struggle to choose an API solution to facilitate seamless data exchange across your healthcare settings, reach out to our experts for a consultation. They will help you select a solution that will suit your company best, guide you on integrating the ready-made product into your clinical settings, or assist you in developing a new API solution from scratch.
Need a qualified team of developers?
Reach new business objectives with the dedicated team of professionals.