The healthcare IT software market is growing quickly. As stated in The Healthcare Technology Report, by 2028, healthcare SaaS alone is anticipated to be worth more than $50 billion. The growth is due to a change in how care organizations function.
Digital tools now affect both how patients are treated and how decisions are made internally. Healthcare software is becoming a key part of both strategic planning and clinical execution, from remote consultations to AI-driven diagnostics.
Organizations are turning to specialized tools that match the increasing complexity of modern healthcare environments. These include making it easier for people in underserved areas to get care, speeding up administrative processes, and supporting compliance with complex regulations.
The growth of different types of medical software is part of a larger trend toward personalized treatment and measurable outcomes. According to Verified Market Reports, by 2033, analytics software alone is expected to hit $22.5 billion, underscoring demand for data-centered tools.
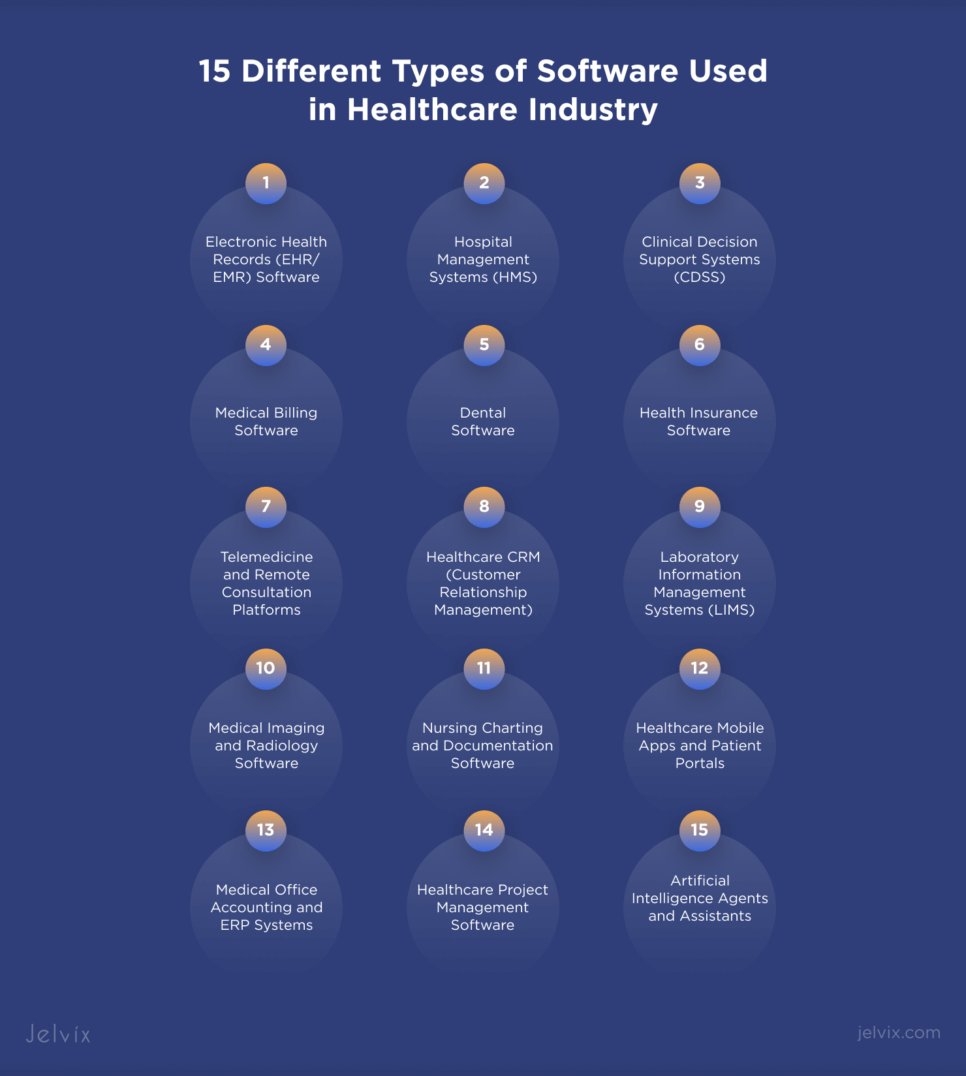
This article outlines 15 different types of software used in the healthcare industry. Every entry includes what the software does, how it fits into a real-world environment, and why it’s becoming popular in today’s market. We’ll talk about the tools that are changing the future of care, from apps for patients to platforms for the back office.
Key Environments Where Healthcare Software Is Used
Healthcare software changes to fit not only the needs of clients but also the pace and infrastructure of the place it works in. In emergency situations, digital systems need to be able to keep up with quick actions and complicated care coordination. They should work as real-time partners instead of just instruments. In outpatient settings, efficiency is the most important measure.
This means that interfaces need to cut down on administrative work and help people make decisions quickly and often. Dental providers typically need workflows that are very visual, with imaging systems and treatment plans that are tightly connected. The program changes in each setting based on the pace of practice, the staff’s bandwidth, and the needs of both the patient and the practitioner.
Long-term and rehabilitative care have different requirements. For example, progress is tracked in little steps, and data continuity takes the place of haste. Software needs to work even when staff members change, make it easier for different types of care to work together, and stay usable for long periods of time.
Insurers put verification, compliance, and structured reporting first, placing financial logic into clinical timetables. When using remote services, you can’t assume that there will always be a connection, and the interface has to be simple enough to be reliable in a clinical setting.
Whether it’s built into the architecture of a big facility or sent to help with care at home, each context changes how healthcare software works.
15 Most Popular Types of Healthcare Software in 2025
Electronic Health Records (EHR/EMR) Software
Doctors can keep track of patient information without using paper thanks to EHR and EMR software. These tools keep all of the medical information, test results, drugs, and notes in one digital spot. What makes them different? EHRs can be shared between multiple doctors and hospitals; however, EMRs can only be utilized at one clinic.
EMR software comes in different formats depending on how and where it’s used:
- Tablet EMR lets doctors use touchscreens or digital pens during checkups.
- Cloud-Based EMR stores data online so you can log in from anywhere.
- On-Premise EMR saves everything on computers inside the clinic.
- Mobile EMR works on smartphones and tablets for on-the-go access.
- Voice Recognition EMR lets doctors speak instead of typing, using speech-to-text.
- Hybrid EMR combines cloud and in-house storage for more flexibility.
EHR systems are built for sharing patient data between hospitals, labs, and specialists. The list of well-known types includes:
- On-Premise EHR installed on the clinic’s own servers.
- SaaS (Cloud) EHR running through a web browser with monthly payments.
- Custom EHR built from scratch for clinics with special needs.
- Integrated EHR + EPM combining patient records and billing in one system.
- Certified EHR officially approved for meeting national healthcare standards.
- Stand-Alone EHR that works on its own without other software systems.
Hospital Management Systems (HMS)
Hospital Management Systems (HMS) are digital control centers. These solutions can handle admissions, discharge planning, scheduling, billing, inventory, and regulatory reporting, all in one safe place. A strong HMS unites departments through a single database, which makes it easier for clinical decision-making and logistical execution to work together.
The best software for managing hospitals might change based on how big and complicated the facility is. Epic and Cerner are two systems that are widely used for large-scale implementations. They offer modular expansions for matters like inpatient care, laboratory information systems, and medication management.
Cloud-native technologies like eHospital and Mediware make it easier for smaller institutions to get things done by requiring less infrastructure. Most of these solutions include HL7 or FHIR protocols, which let structured data be shared with other systems like national health registries or insurance databases.
The HMS architecture has built-in features for managing patients. It keeps track of beds in real time, sets up admissions, handles case histories, and makes follow-up appointments. You can set up integrated notifications for lab result flags, drug interactions, or vital sign thresholds. With role-based access, just the data that is relevant to each user’s job is available to them. This includes everyone from triage nurses to department leaders.
Medical Billing Software
Medical billing software is the financial engine behind modern clinical operations. It handles claims, checks insurance coverage, keeps track of payments, and makes sure that each step follows the regulations set by the payer.
The software cuts down on mistakes made when entering information by automatically filling up claim fields with clinical data from EHRs or hospital systems. Automating code mapping, denial management, and follow-up scheduling is a key part of speeding up revenue cycles.
There are many types of medical billing software. Some platforms are meant to be used as stand-alone billing solutions, while others are included within larger EHR or hospital administration suites. Small practices that need flexibility and low infrastructure costs, such as cloud-based systems like DrChrono or Kareo.
Waystar and NextGen are examples of enterprise-level technologies that offer comprehensive analytics, customisable reporting modules, and support for operations in several locations. These platforms also have capabilities to help with adhering to regulations like HIPAA, ICD-11 updates, and payment models based on value-based care.
When choosing medical billing software, decision-makers generally look at how well it works with other systems and how accurate its claim scrubber is before looking at how many features it has. Systems need to work well with hospital software such as EMRs, patient registration modules, and portals for checking insurance eligibility.
If you don’t have that alignment, you could get your claims denied, your reimbursements delayed, or be at risk of not following the rules.
Health Insurance Software
Health insurance software operates as a critical infrastructure layer between payers, providers, and patients. Unlike technologies that can be used for various purposes, customized health insurance systems demonstrate how the insurer operates, the rules it must follow, and its long-term objectives.
Off-the-shelf choices are easy to set up quickly, but custom platforms let you align your internal procedures over the long run and have more control over how your data is structured.
Most payer-side ecosystems are built on claim-centric systems. These solutions make it easier to submit, check, and decide on claims. Fraud detection algorithms and compliance checks operate simultaneously, reducing the need for manual intervention and minimizing the risk of errors when reimbursing.
When used in conjunction with machine learning, claims platforms can identify issues early and expedite processing in areas with a high volume of claims.
Agent-facing software helps with sales funnels, commissions, and the policy life cycle. With integrated CRM features, you can adjust policies in real time, automate onboarding, and group clients. This technique makes the sales funnel clearer for insurers with big sales teams and cuts down on overhead.
Patient-centered systems put the most important elements first, such as user access, remote communication, and health coordination. These generally come with smartphone apps, chat portals, and self-service dashboards that let you choose a plan and keep track of your benefits.
When these interfaces are integrated into larger health insurance software stacks, they make members happier and reduce the amount of support work that needs to be done.
Policy management solutions make things easier for administrators by eliminating the need to manually track information. Digital records that can be searched replace static documents. This makes it easy to keep track of renewals, make quick adjustments, and keep track of compliance.
These systems are a crucial element of the computer software used in hospitals when verifying third-party insurance claims as part of the billing process.
Other adjacent options are data analysis engines for predicting, modeling performance, and dividing customers into groups, which are all important for risk scoring and premium strategy. Risk analysis tools use medical histories and past claims to figure up coverage terms and pricing tiers with perfect accuracy.
Lead management tools and scheduling systems help sales enablement even more by keeping track of conversion metrics and operational throughput without having to do things by hand.
It is important to be able to work with claims management systems. Fragmented systems produce delays, rework, and audit failures. Unified platforms, whether custom-built or heavily customized, enable fluid data exchange between hospitals, insurers, and regulatory bodies, building a connected ecosystem that delivers both accuracy and speed.
Clinical Decision Support Systems (CDSS)
Clinical Decision Support Systems serve as intelligent layers within clinical software, guiding medical teams toward accurate decisions based on data, algorithms, and established protocols. Modern CDSS typically combine two core functions: identifying a patient’s condition and recommending what actions to take next.
For example, a system may detect a renal impairment and adjust dosage recommendations automatically based on lab data. These tools pull data from electronic health records and apply encoded clinical logic, supporting both diagnostics and treatment planning.
System classification depends on several variables, including user interaction design, communication model, and computational logic. In terms of interaction, CDSS tools today range from EHR overlays to voice-activated modules or visual prompts. Communication can occur via alerts, pop-ups, or inline suggestions during order entry. The underlying decision models also differ.
Many rely on structured logic—such as decision trees, clinical rules, or flowcharts—that align with guideline-based care. These are human-readable and align closely with conventional practice. Others incorporate probabilistic frameworks or machine learning models like neural networks and support vector machines, which can uncover patterns beyond human cognition but often lack transparency.
Although black-box systems offer high predictive performance, adoption lags due to trust concerns. When outputs diverge from established guidelines without a clear rationale, clinicians hesitate. Interpretability and guideline alignment remain key to clinical adoption, especially in high-stakes decision environments.
Telemedicine and Remote Consultation Platforms
Telemedicine systems are becoming necessary for providing care outside of hospitals. Most solutions let you access patient records, e-prescriptions, and encounter documentation directly from the virtual consultation environment.
With synchronous telemedicine software, patients and clinicians can talk to one another in real time. People commonly use these systems when they need to make quick clinical decisions. The interface usually lets more than one person join a conference, share a screen, and connect medical devices in real time for live readings.
Patients can provide data, pictures, or queries to asynchronous solutions, also known as store-and-forward platforms, without starting a live session. Providers can look over submissions at set times, which makes the system flexible and helps both clinical accuracy and provider productivity.
This model is often utilized in dermatology, radiography, and ophthalmology, where real-time contact isn’t very important, but the quality of the documentation and the accuracy of the images are.
Remote patient monitoring is a new feature of telemedicine platforms. Software in this group constantly collects biometric data and sends it to healthcare providers for examination.
To build this kind of infrastructure, you frequently have to make sure that it works with current systems, data compliance frameworks, and specific logic for how devices send data. Healthcare software development is a key part of building reliable and flexible telemedicine ecosystems for businesses that need solutions that can grow and meet regulations.
Healthcare CRM (Customer Relationship Management)
Healthcare CRM systems can be divided into three main groups based on how they work: sales automation, marketing automation, and service automation. Sales-focused settings handle B2B pipelines, which include coordinating referrals, medical device vendors, and lab services.
Marketing automation engines help with targeting specific groups of people, launching campaigns, and communicating with customers about your brand. These are often linked to the growth of your service line. Automation takes care of duties like checking provider availability, taking in new patients, and sorting patients by nurse.
This operational layer is very important for digital health platforms, especially when they are connected to telehealth networks.
Healthcare CRMs are built on the same technical basis as other popular systems. Unified communication monitoring, task management, document handling, and engagement across email, online, and phone are some of the most important aspects. Salesforce Health Cloud and Keona Health are examples of cloud-based solutions that use software-as-a-service architectures to make sure that care environments can be flexible and always up-to-date.
Medical Imaging and Radiology Software
Radiologists use software platforms that can manage high-resolution image data, facilitate clinical reporting, and enable collaboration from a distance. These systems are part of hospital networks and diagnostic procedures, and they help with both getting images and understanding them in different places.
Picture Archiving and Communication System (PACS) is a key system in this area. It connects directly to imaging equipment and keeps image data in one place. PACS supports access from several points, which makes it easier for professionals to look at and compare studies without having to wait for physical media.
Radiology Information Systems (RIS) add a layer of workflow to imaging. These systems set up exams, keep track of how well procedures are going, send out reports, and store all of the radiology department’s administrative data in one place.
DICOM viewer software shows diagnostic picture formats in a clinical setting. It reads Digital Imaging and Communications in Medicine (DICOM) files and lets radiologists look at scan data with built-in tools for measuring, adding notes, and changing the contrast. Viewer platforms are typically designed to support multi-modality, allowing for seamless switching between CT, MRI, PET, and ultrasound studies.
Advanced visualization software turns 2D image sequences into 3D models that you may interact with. These systems can run techniques like volume rendering, multiplanar reconstruction, and segmentation procedures.
Teleradiology software sends imaging studies across secure networks so that they can be read and discussed from a distance. Radiology organizations, hospitals, and diagnostic service providers use these platforms to provide coverage after hours or work with subspecialists.
Radiomics software pulls out numerical information from medical images to help with predictive modeling and making more accurate diagnoses. In cancer care and research, these technologies are often used to look at large collections of images to find patterns that are related to certain diseases or how well a therapy works.
Laboratory Information Management Systems (LIMS)
A Laboratory Information Management System (LIMS) is a configurable software platform used to manage laboratory workflows, track data, and facilitate integration between instruments, users, and enterprise systems.
At its core, a LIMS enables laboratories to register, monitor, and report on samples. Every implementation includes a workflow engine and structured data capture. Beyond this baseline, system capabilities vary considerably depending on the domain, from pharmaceutical R&D to clinical diagnostics.
In pharmaceutical applications, LIMS solutions may integrate stability testing modules, electronic lab notebooks, and compound tracking. In clinical laboratories, LIS components often include patient records, diagnostic coding, and case-specific documentation.
Read more about the role of the app development companies in medical diagnostics.
Nursing Charting and Documentation Software
Nursing charting and documentation software is very important for making sure that patient care actions are recorded correctly and in real time. These systems keep track of observations, healthcare delivery, assessments, and care plans, which directly affect how consistent treatment is and how well the law is followed.
They are made for use by front-line clinicians and focus on making it easy to enter data, reducing errors, and getting to the patient history right away.
There are many different types of nursing charting systems. We talk about flow sheet-based documentation, narrative entry, checklist models, and smart forms for organized data input. Because they are easy to read and provide quick access to vital signs, procedures, and intake-output tracking, flow sheets are often utilized in acute settings.
Smart form systems, which are commonly built into enterprise EHRs, let you use conditional logic and adaptable input fields that vary depending on the patient’s state or the care protocols.
Healthcare Mobile Apps and Patient Portals
Healthcare apps are made to meet specific needs within this larger ecosystem. These needs might be anything from following up after a hospital stay to keeping track of a chronic ailment.
Condition-specific apps support targeted interventions. For example, a diabetes management app may include carb-counting tools, while a cardiac rehab app may offer progress dashboards for exercise tolerance and vitals.
Fitness and wellness applications are in a similar group, but they don’t often connect to treatment routes directly. These platforms keep track of things like your sleep quality, physical activity, or nutrition. The information they collect can be used during consultations or discussions regarding preventive care. Certain businesses and insurance companies promote these apps to help with public health efforts.
Healthcare apps help patients become more informed, increase treatment continuity, and show quantifiable improvements in engagement metrics across all categories. Their connection to formal health systems is getting stronger all the time, especially as remote monitoring and value-based care models become more common.
Dental Software
The most common systems among dental software for managing patient records store medical history, treatment notes, diagnostic data, and billing information in structured formats. Cloud-based technologies now allow for collecting data from afar, easily connecting with practice management software, and automating appointment tracking and billing, all while complying with regulatory standards.
Other types of dental software help with matters like planning treatments, taking diagnostic images, and inter-practitioner communication. Clinical decision support systems give evidence-based suggestions for procedures, while teledentistry platforms make it easier to have consultations, share images, and work on cases with people in different places.
Educational software for fields including periodontology, endodontics, and dental pathology helps with simulation-based learning and ongoing education.
Intraoral cameras, digital X-ray devices, and CAD/CAM systems are examples of diagnostic tools that use specialized software to collect, process, and display clinical data. All types of dental software are made to work with electronic patient records.
Medical Office Accounting and ERP Systems
Medical office accounting software is made to manage the financial needs of healthcare settings. It does this by integrating general ledger functions with modules for claims reconciliation, insurance modifications, patient billing, and tracking co-pays. These systems work directly with EHR platforms and practice management software to keep billing events and clinical activities in sync.
Some of the most important features are automated charge recording, real-time claim status tracking, and access to financial information depending on roles. Advanced implementations support ANSI X12 electronic data interchange formats, which makes it easy to communicate with clearinghouses and payer systems.
Enterprise resource planning (ERP) systems go beyond billing in more complicated settings. They often incorporate inventory management, payroll, compliance tracking, and financial forecasting. ERP systems give hospital groups and multisite networks a centralized view of all departments, which improves strategic planning and operational control.
Healthcare Project Management Software
Healthcare project management software is designed to help healthcare companies plan and carry out clinical, operational, and administrative projects. These tools let you see Gantt charts, allocate resources, map dependencies, and manage milestones in real time. This makes it possible to keep a close eye on complicated projects like EHR rollouts, facility expansions, or compliance audits.
Healthcare-specific platforms frequently come with templates that are unique to rules like HIPAA or HITECH. They also have audit logging, version control, and access controls that are in line with healthcare data governance requirements.
Artificial Intelligence Agents and Assistants
AI agents in healthcare have changed into systems that are task-specific and data-driven. They can automate medical decisions, sort patients, and tailor care routes to each of them. Some of the most important uses for AI in 2025 are helping with clinical documentation, reconciling medications, and adding AI-powered virtual assistants to patient portals.
Real-world examples include Nuance DAX for ambient clinical documentation and IBM Watson Assistant for care coordination. Hospitals also use AI to make discharge planning easier, automate follow-ups, and use real-time EHR data to figure out how likely it is that a patient will have to go back to the hospital.
Healthcare chatbots and virtual rehabilitation assistants are now more aware of their surroundings and act in an ethical way. The Jelvix chatbot case is a great illustration of this since it shows how ethical AI concepts were used to make a virtual healthcare assistant.
The assistant used rule-based workflows and adaptive machine learning to sort through symptoms, give health advice based on evidence, and forward cases to human physicians as necessary. Some of the most important aspects were architecture that followed GDPR and HIPAA rules, answer modules that were aware of emotions, and the capacity to tell the difference between low-risk questions and situations that needed clinical help.
These agents not only lighten the load on call centers, but they also make it easier for people who don’t have enough access to care to get it.
When Do You Need Custom Healthcare Software?
Custom healthcare software becomes necessary when predefined platforms cannot support the unique demands of your operations. Tailored solutions offer better control, adaptability, and long-term scalability.
You need custom healthcare software when:
- Your workflows require functionality not available in commercial solutions.
- Integration with legacy systems or specialized medical devices is critical.
- You operate under complex regulatory or security constraints.
- Multi-location data synchronization or custom reporting is a core requirement.
- You need to scale or adapt features as services evolve over time.
- Patient or provider-facing interfaces demand a unique experience.
- Real-time analytics or decision support tools must align with specific use cases.
Custom development ensures software is built around your objectives, not the other way around.
Factors to Consider Before Building Healthcare Software
Before launching any healthcare software project, it’s important to look at the technical, regulatory, and operational environment that the solution will have to work in. A focused pre-development evaluation helps lower risk, makes the system easier to use, and ensures it will remain functional for a long time.
Compliance requirements need to be dealt with right away. Solutions should be in line with HIPAA, GDPR, HL7, and FHIR to ensure that data is handled legally and can work with other systems. When working with sensitive patient data across many teams, data security architecture should provide end-to-end encryption, access control, and audit trails.
Interoperability with older systems is generally not up for discussion; integration plans must allow for specific APIs, structured data mapping, and synchronization in real time.
Long-term performance is affected by scalability and cloud readiness. Infrastructure needs to be able to handle user growth, changes in regulations, and modular expansion without any downtime.
The design of clinical UX/UI affects how well workflows work. Interfaces should make clicking less deep, provide context-aware inputs, and work well on both mobile and desktop.
Choosing the right vendor is important. Working with a team that has experience in regulated environments ensures that both domain knowledge and technical rigor are present.
Taking these things into account from the start helps you build healthcare software that works well, stays compliant, and adds measurable clinical and operational value.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

Conclusion — Innovate with Confidence
The future of healthcare IT software is in smart integration, automation based on data, and interoperability throughout the whole system. New platforms are going beyond separate functions to create cohesive environments. Cloud-native architectures, AI-powered analytics, and modular EHR components are becoming standard.
This lets enterprises add or remove features as needed to keep up with changes in regulations and care models. Digital twins, ambient voice interfaces, and predictive diagnoses are moving from research labs to commercial use. This raises both the expectations and the complexity of modern healthcare systems.
To go through this landscape, you need more than just technical skills. When you work with teams that specialize in healthcare product development, you can be sure that infrastructure, UX, and compliance are all seen as parts of a solid software ecosystem that depend on each other.
Companies like Jelvix use their experience in specialized industries to speed up deadlines, cut down on rework, and make sure that products meet the needs of providers, payers, and patients. When creating systems that affect sensitive areas like behavioral health or specialist care, it’s extremely important to have this level of awareness.
Getting a product team involved early in the planning process helps make sure that commercial goals, clinical goals, and technological choices are all in line. Jelvix makes unique healthcare software that meets the demands of your company, whether you need a comprehensive digital platform or just a specific part, such as Mental Health EHR integration, patient interaction modules, or analytics engines.
It’s not an expense to work with experienced engineers and domain experts to make software that is compliant, scalable, and really works in healthcare. It’s an investment in the product’s viability. Let’s connect!
FAQ
What are the benefits of using software in healthcare settings?
Healthcare software boosts clinical efficiency, improves patient care, minimizes manual mistakes, guarantees compliance with regulations, and facilitates better decision-making through data analytics and seamless department interoperability.
How is healthcare software regulated for safety and compliance?
In the U.S., healthcare software must follow rules like HIPAA, in Europe, it must follow GDPR, and for data transmission, it must follow standards like HL7 and FHIR. Software manufacturers also have to follow rules for getting their medical device software (SaMD) certified and are checked on a regular basis.
Can small clinics and private practices afford healthcare software?
Yes. A lot of companies sell cloud-based healthcare IT solutions that are affordable and well-suited for small clinics and solo practitioners. These frequently have modular pricing, which makes it easy to scale while the practice grows.
What are examples of healthcare IT service providers?
Leading healthcare IT service providers include Cerner, Epic Systems, Allscripts, McKesson, GE Healthcare, and Jelvix. They offer services like custom software development, system integration, data migration, and digital transformation.
How do I choose the right type of medical software for my facility?
Consider your facility’s size, specialty, patient volume, and regulatory needs. Look at solutions based on how easy they are to use, how well they work with other software, how good their support is, and how well-known the company is. Getting help from a healthcare IT partner like Jelvix might make this process go more smoothly.
Need a qualified team of developers?
Unlock new business opportunities with the first-rate dedicated development team.