Patient safety has always been a whopping issue in U.S. healthcare. In 1999, the IOM published a report that focused on patient safety problems, indicating the increasing number of deaths. As of 2023, about 795,000 Americans died or faced permanent disability due to misdiagnosed medical conditions yearly.
High-profile medical errors and patient safety concerns made healthcare organizations seek solutions to prevent these issues. A clinical decision support system, with its ability to flag potential safety issues, gained prominence as a tool to enhance patient safety and improve quality of care.
If you’re struggling to manage vast amounts of patient data and keep up with constantly changing medical guidelines, read this article. You’ll find out how CDSS can help you get timely and relevant insights into patient conditions, reduce errors, and optimize care delivery.
What is a Decision Support System in Healthcare?
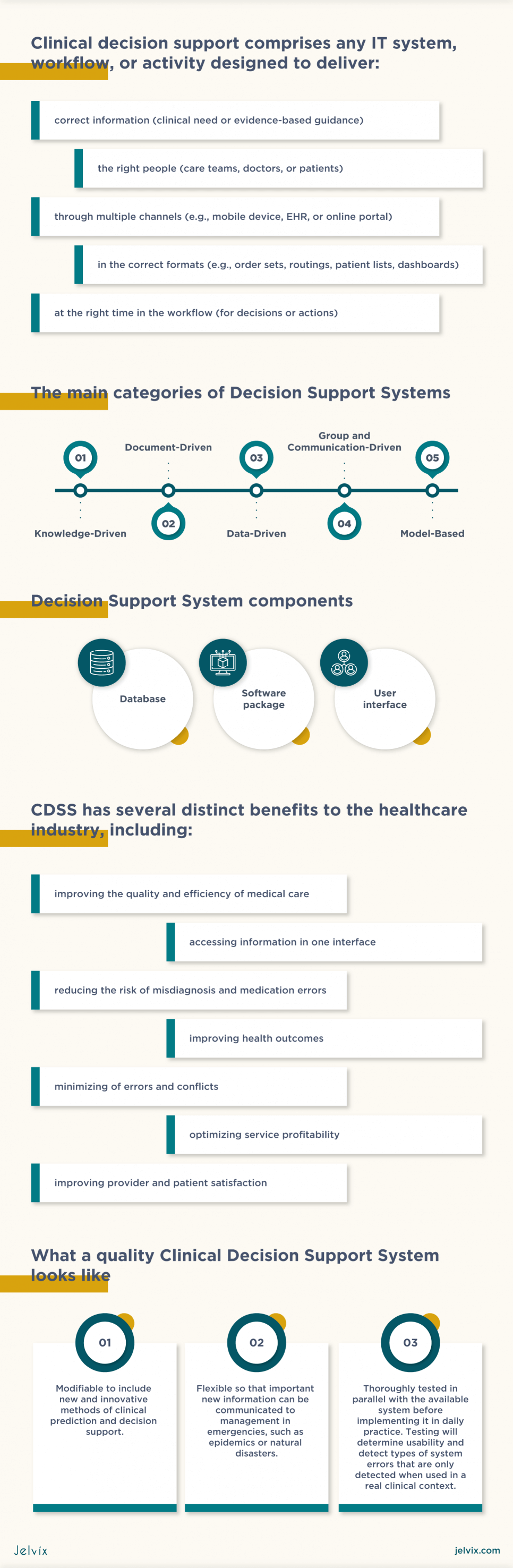
A Decision Support System (DSS) is a computer-based tool that aids individuals or organizations in making informed decisions by processing and analyzing data, providing relevant information, and generating insights or recommendations.
In healthcare, a Clinical Decision Support System (CDSS) helps medical professionals make data-driven decisions about patient care, operations, and management. It combines data analysis, knowledge management, and user-friendly interfaces to provide actionable insights to improve healthcare delivery and outcomes.
In contrast, Decision Support Systems (DSS) are broader in scope and can be applied across various industries and domains beyond healthcare. They can be customized for diverse decision-making needs, using analytical tools and models to address complex problems and optimize business outcomes.
What Is a Clinical Decision Support System?
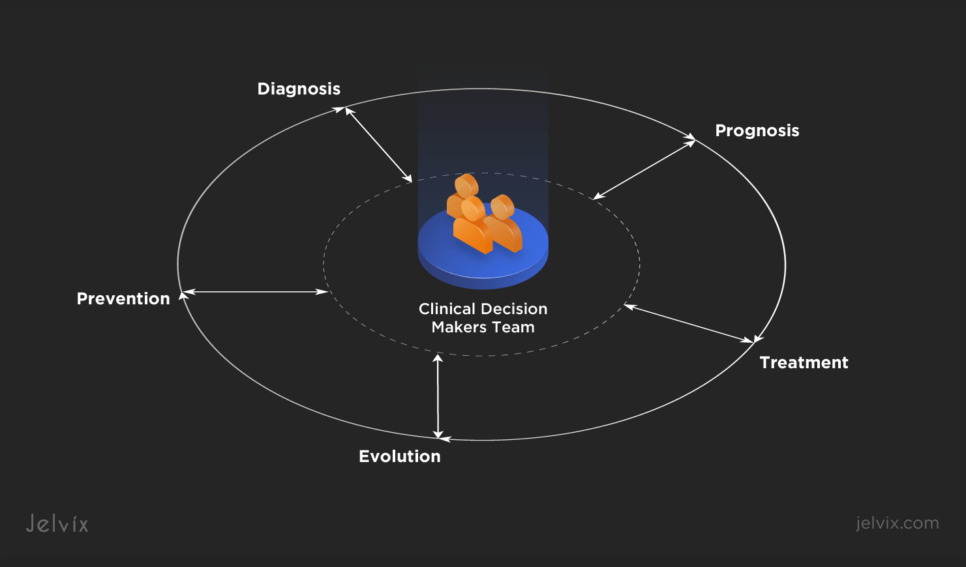
A Clinical Decision Support System (CDSS) is a tool designed to assist healthcare professionals, including physicians, nurses, and other clinicians, in making informed decisions about patient care. The CDSS integrates medical knowledge with patient data to provide evidence-based recommendations or warnings. It can help in diagnosing, treatment planning, and managing patient care more effectively.
The CDSS integrates patient-specific data from electronic health records (EHRs) with a comprehensive medical knowledge base, algorithms, and decision-making tools. By analyzing vast amounts of data and using algorithms and medical guidelines, the CDSS enhances the accuracy and efficiency of care.
Explore CRM-EHR Integration for enhanced patient care and operational efficiency in your healthcare institution.
Types of Clinical Decision Support Systems
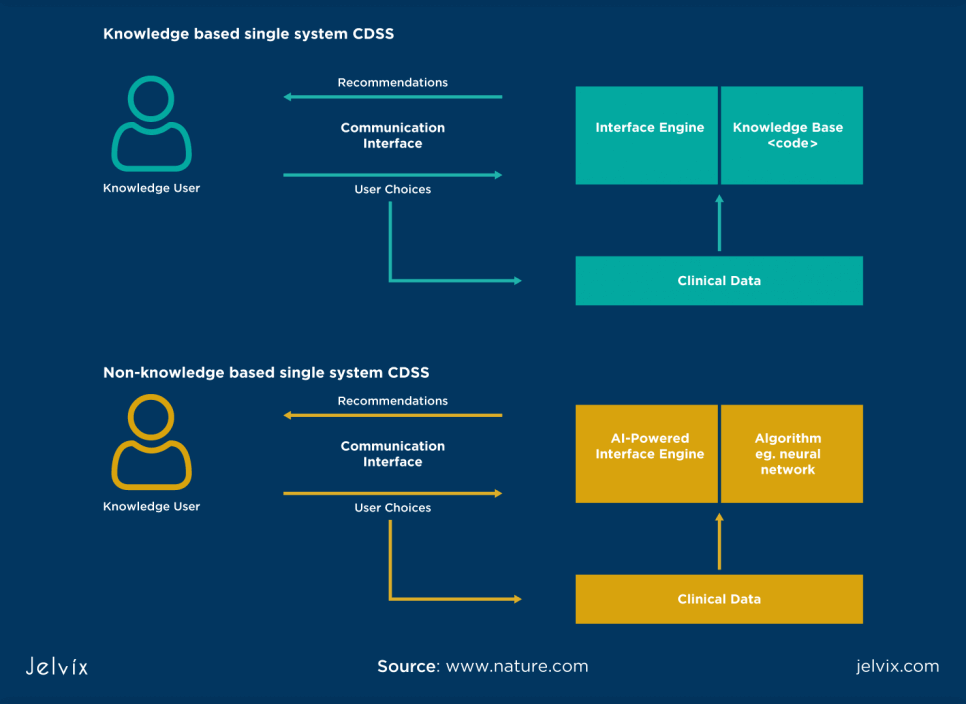
There are two main types of clinical decision support systems: knowledge-based and non-knowledge-based. Both types play important roles in supporting healthcare staff in improving patient care.
A Knowledge-Based CDSS
A knowledge-based CDSS relies on an extensive knowledge base of clinical guidelines, medical literature, expert opinions, and rules. This system uses rule-based engines to provide recommendations and alerts to physicians based on patient-specific data:
- Knowledge base: this system has a comprehensive database of medical knowledge, including information on diseases, treatments, drug interactions, and best practices;
- Patient data analysis: it analyzes patient-specific data, such as medical history, symptoms, test results, and demographic information;
- Rule-based reasoning: using rule-based reasoning, the CDSS matches the patient’s data against predefined rules and guidelines in its knowledge base;
- Recommendations: based on the analysis and rule matching, the CDSS generates recommendations and alerts for physicians. These recommendations include suggested diagnoses, treatment options, medication choices, and warnings about potential issues or contraindications;
- Clinical guidelines: the CDSS adheres to established clinical guidelines and protocols. It ensures that healthcare pros follow evidence-based practices and can provide explanations for its recommendations based on the rules and guidelines it uses.
A Non-Knowledge-Based CDSS
The non-knowledge-based CDSS, in contrast, relies on statistical and machine learning techniques to analyze large datasets and extract insights. This system can identify patterns, correlations, and trends in patient data without relying on predefined rules:
- Data analysis: this system processes vast amounts of patient data, including EHRs, laboratory results, and medical images;
- Machine learning algorithms: it uses ML algorithms to identify patterns that may not be evident to human observers. This can involve techniques like clustering, classification, regression, and natural language processing;
- Data-driven insights: a non-knowledge-based CDSS generates insights based on data-driven patterns and correlations that can include predictions, risk assessments, and recommendations for treatment or further diagnostic tests;
- Adaptability: a non-knowledge-based CDSS can adapt and learn from new data. It continuously refines its models and recommendations as it examines more patient cases.
The Main Categories of a CDSS
A CDSS can be divided into multiple categories each serving specific purposes and addressing various aspects of clinical decision support. The choice should depend on the specific needs, goals, and challenges of a healthcare organization.
A knowledge-Driven CDSS
A knowledge-driven CDSS relies on an established knowledge base of clinical guidelines, medical literature, expert opinions, and predefined rules. It uses this knowledge to provide recommendations and alerts to physicians based on patient-specific data. This type of CDSS is often rule-based, providing guidance aligned with clinical best practices and established guidelines. It emphasizes adherence to evidence-based medicine and aims to reduce variability in care decisions.
A Data-Driven CDSS
A data-driven CDSS utilizes statistical and machine-learning techniques to analyze large datasets containing patient information. It identifies patterns, correlations, and trends in the data to support clinical decision-making. The data-driven CDSS uses the power of big data and advanced analytics to reveal insights that may not be available through traditional rule-based systems. It adapts and learns from new data, making it suitable for complex healthcare scenarios.
A document-Driven CDSS
A document-driven CDSS focuses on the analysis of clinical documentation, including EHRs, medical reports, and patient histories. It employs natural language processing and text analysis to extract relevant information. The document-driven CDSS enhances the accessibility of unstructured clinical notes by converting them into structured data.
A communication-Driven CDSS
A communication-driven CDSS facilitates collaboration and communication among healthcare teams. It provides tools for group decision-making, information sharing, and consensus building. This category of CDSS fosters teamwork, enabling multiple healthcare professionals to collectively assess patient cases, discuss treatment options, and reach agreement on care strategies.
A model-Based CDSS
A model-based CDSS employs mathematical and computational models to simulate various clinical scenarios. It helps healthcare providers assess the potential outcomes of different treatment options. The model-based CDSS allows healthcare professionals to experiment with different scenarios, predict patient outcomes, and evaluate the impact of interventions.
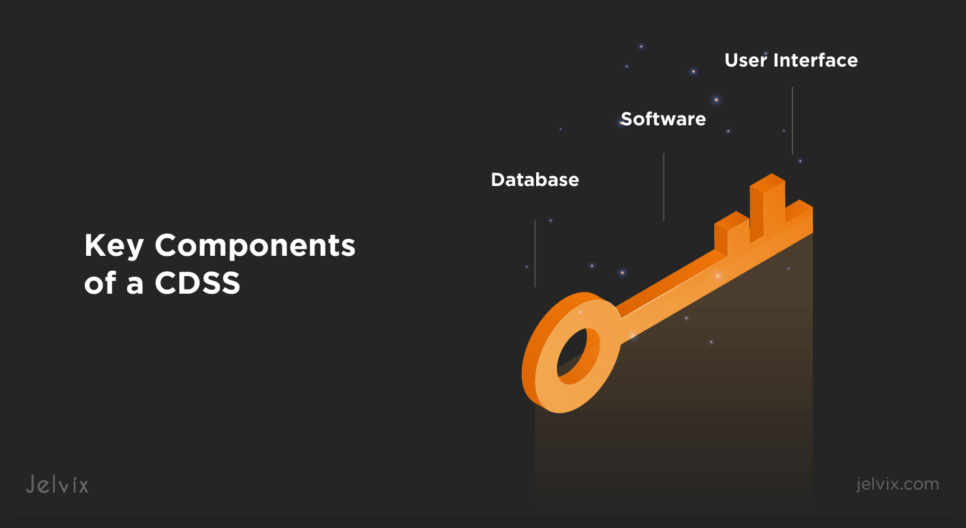
Key Components of a CDSS
A CDSS includes key components that work together to enable it to provide clinical decision support to healthcare staff. The database stores and manages patient data and knowledge, the software processes and analyzes this data, and the user interface presents the results in a way that is accessible to healthcare professionals.
Database
The database is a fundamental component of any CDSS. It serves as the storage system for all structured and unstructured healthcare data, including patient records, medical histories, laboratory results, and clinical guidelines. Database forms the foundation for data retrieval, allowing the system to generate accurate recommendations and alerts based on patient-specific data.
Software
Software is the brain of any CDSS, responsible for analyzing patient data, applying clinical knowledge, and providing decision support. It includes the computational and analytical capabilities needed to process patient data, interpret clinical guidelines, and generate recommendations and alerts. Software may also incorporate machine learning algorithms in a data-driven CDSS to identify patterns and insights.
User Interface
The user interface is the part of the CDSS that allows physicians to interact with the system. It includes the design, layout, and functionality of the interface, which can be web-based, mobile, or integrated with EHRs. The user interface presents recommendations, alerts, and relevant patient data to clinicians in a user-friendly and comprehensible manner. A well-designed UI enhances the CDSS’s usability, ensuring that healthcare professionals can use its capabilities efficiently in their clinical workflows.
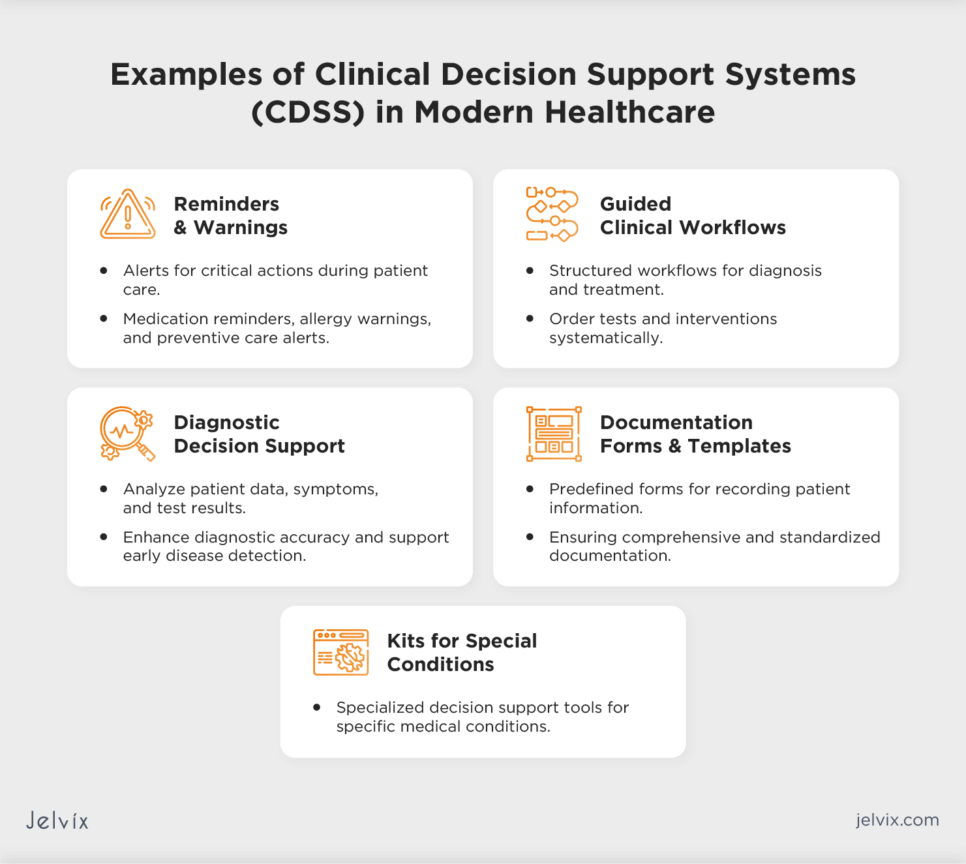
Examples of Clinical Decision Support Systems in Modern Healthcare
CDSS can help diagnose medical conditions, recommend treatments, and prevent medical errors. Real-world CDSS applications demonstrate how these systems streamline clinical workflows and lead to shorter hospital stays, reduced wait times, and effective use of healthcare resources.
Reminders and Warnings
CDSS can issue reminders and warnings about critical actions that need to be taken during patient care. This includes medication reminders, allergy warnings, and preventive care alerts. These systems help reduce medication errors, improve adherence to clinical guidelines, and enhance patient safety by preventing adverse events.
Guided Clinical Workflows
CDSS can guide clinicians through structured clinical workflows, ensuring that each step of a diagnostic or treatment process is followed systematically. It may include ordering tests, assessments, and interventions in the correct sequence. As a result, CDS systems streamline care processes, reduce variability in practice, and ensure standardized and evidence-based care delivery.
Diagnostic Decision Support
A CDSS assists healthcare providers in diagnosing medical conditions by analyzing patient data, symptoms, and test results. It provides differential diagnoses, suggests further tests, and offers diagnostic probabilities that are sent to human physicians for analysis. This enhances diagnostic accuracy, supports early disease detection, and aids in complex diagnostic scenarios.
Documentation Forms and Templates
A CDSS offers predefined documentation forms and templates for recording patient information, assessments, and treatment plans. These templates ensure comprehensive and standardized documentation, improving the accuracy and completeness of medical records, reducing documentation errors, and supporting compliance with regulatory requirements.
Kits for Special Conditions
A CDSS provides specialized kits or decision support tools for managing specific medical conditions. Examples include diabetes management, antenatal care, and chronic disease management. These kits tailor care plans to the unique needs of patients with specific conditions, promote proactive disease management, and improve patient outcomes.
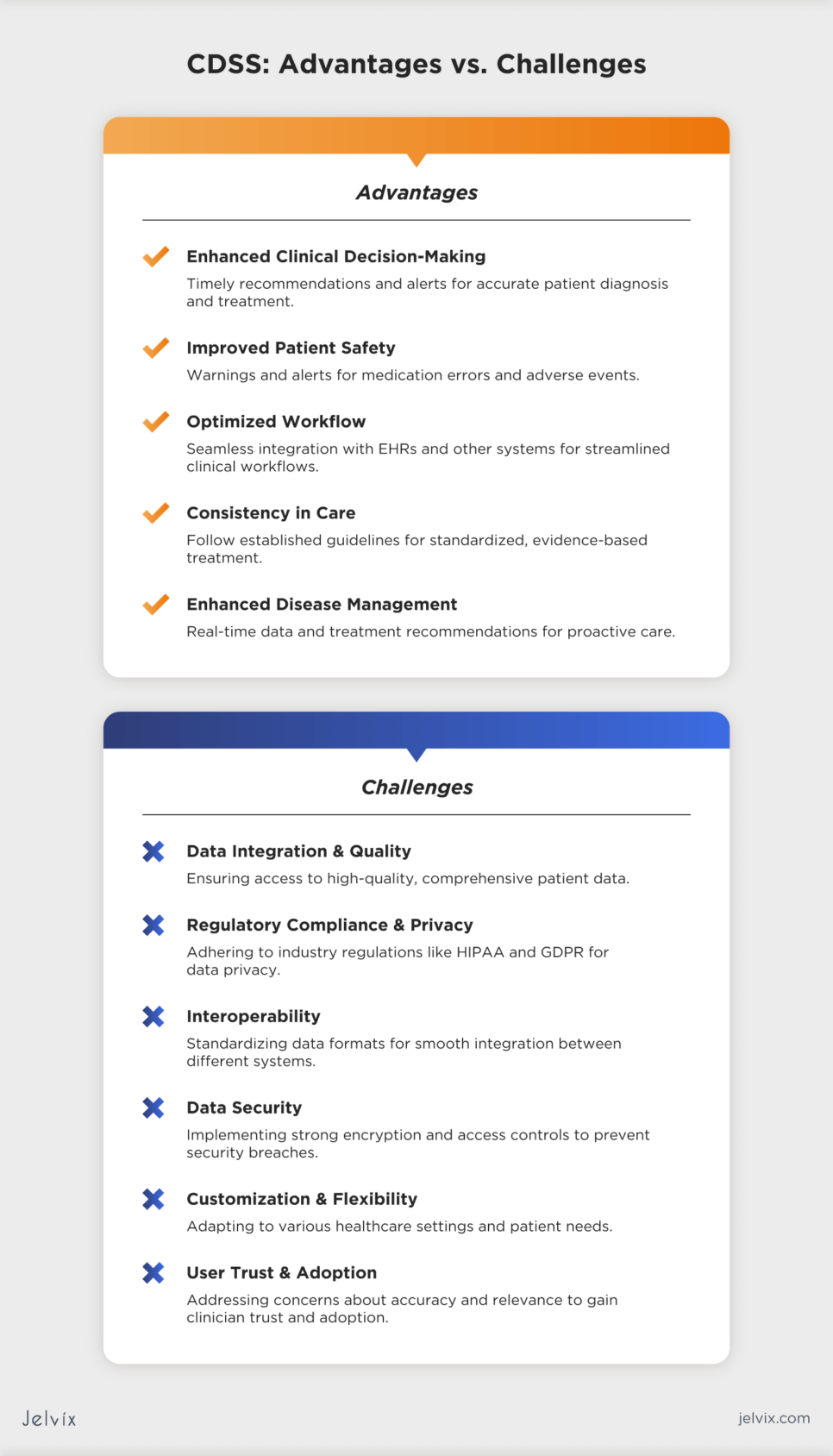
Advantages of a Clinical Decision Support System
As noted earlier in this article, a CDSS can be truly beneficial in assisting medical staff in making care-related decisions. This system helps improve patient outcomes, reduce medical errors, and improve clinical efficiency.
Enhanced Clinical Decision-Making
A CDSS provides physicians with timely and evidence-based recommendations, alerts, and reminders. This helps to make accurate decisions regarding patient diagnosis, treatment, and management. It can also improve remote patient monitoring by integrating and analyzing data from RPM devices, allowing physicians to make timely and accurate assessments.
Improved Patient Safety
A CDSS can issue warnings and alerts for medication errors, drug interactions, allergies, and potential adverse events. These safety checks reduce the risk of medication-related harm, enhancing patient safety.
Optimized Workflow
A CDSS can integrate seamlessly with EHRs, chatbots for healthcare, and other systems, streamlining clinical workflows. This integration reduces administrative burden on staff, minimizes manual data entry and errors, and improves overall workflow efficiency.
Consistency in Care
A CDSS follows established clinical guidelines and best practices consistently. This helps standardize care across healthcare settings and ensures that patients receive high-quality, evidence-based treatment regardless of the healthcare provider.
Enhanced Disease Management
A CDSS supports chronic disease management by providing clinicians with real-time patient data and treatment recommendations. This enables proactive care and early intervention for patients with chronic conditions.
Decision Support Systems and Analytics
Analytics in a CDSS plays its role in transforming raw healthcare data into actionable insights. This info is used to inform decision-making, optimize operations, and enhance patient care. A CDSS can use various types of analytics to aid healthcare pros in making informed decisions:
- Descriptive analytics: analyzes historical data to understand the changes over time and identify patterns and trends;
- Predictive analytics: uses data, statistical algorithms, and machine learning techniques to predict patient risks or the probable progression of diseases;
- Prescriptive analytics: provides recommendations on actions to achieve desired outcomes. This could include treatment options based on patient history and current health data;
- Diagnostic analytics: assists in the examination of data to understand the cause of events and behaviors. This involves analyzing clinical data to understand the cause of a patient’s condition.
Challenges of Healthcare Decision Support Systems
Although a CDSS brings numerous benefits that leverage healthcare practice, it also possesses challenges that range from establishing interoperability between various systems to helping patients and doctors adapt to new technologies. The Jelvix team recommends addressing these challenges to make your CDSS effective and user-friendly.
Data Integration and Quality
Ensuring the CDSS has access to high-quality, comprehensive patient data from various sources is a major challenge. Poor data quality can lead to inaccurate recommendations and compromising care outcomes. Consider developing algorithms and frameworks for integrating and cleansing data from diverse sources to improve data quality and relevance.
Regulatory Compliance and Privacy
Ensuring privacy and compliance requires a solid understanding of industry regulations, continuous updates to the systems as laws change, and implementation of strong data protection measures. Make sure your system adheres to HIPAA in the U.S. and GDPR in the EU to ensure data privacy.
Interoperability
Interoperability means making different health systems work together smoothly. The key challenge here is to standardize how data is formatted and exchanged. Use common data formats like HL7 and FHIR to help different systems understand each other’s data, ensuring doctors have all the patient information they need for accurate decisions.
Explore how implementing FHIR can revolutionize data sharing in the healthcare industry.
Data Security
A CDSS should offer safe access to data to prevent security breaches and data leaks. Implement strong data encryption algorithms, such as AES and RSA, establish access controls based on two-factor authentication, and conduct regular security audits to enhance the safety of your system.
Customization and Flexibility
A CDSS needs to be adaptable to different healthcare settings and customizable to individual patient needs. Develop a system that is adaptable to various healthcare settings and customizable to individual healthcare workflows and patient needs.
User Trust and Adoption
Clinicians may be hesitant to rely on a CDSS due to concerns about accuracy or relevance. Demonstration of the system’s effectiveness can help establish trusting relations with clinicians. Educate physicians on the benefits and limitations of a CDSS and conduct training sessions to facilitate the use of the system.
CDSS’ Prospects for The Future
The future of clinical decision support systems looks promising, with advancements focusing on enhancing precision medicine and personalized care.
CDS systems are expected to integrate machine learning and artificial intelligence, allowing for more accurate and individualized patient treatment plans. Research in a Norwegian Hospital confirmed that an NLP-driven CDSS demonstrated increased detection of patient allergies. What’s more, the system showed a high acceptance rate by physicians.
CDS systems are likely to be integrated into telehealth solutions. This approach is expected to result in better support for patients with two or more long-term health conditions and improve the accessibility to care.
Overall, the CDSS will experience wider adoption, with its market expected to reach $3.74 billion by 2030. The system itself will become more sophisticated and intuitive to transform both the patient experience and clinical outcomes.
What a Quality Clinical Decision Support Software Should Look Like
A quality CDSS should be designed to offer accurate, evidence-based recommendations in a user-friendly interface. It should be customizable and flexible, able to integrate seamlessly with existing healthcare systems, such as EHRs.
Real-time data processing and comprehensive data analysis are essential for timely and effective decision-making. The system should focus on patient-centric care, adhering to privacy and security regulations like HIPAA and GDPR. What’s more, ongoing support, maintenance, and a feedback mechanism can contribute to continuous improvement and reliability of the system.
How To Choose a CDSS for Your Needs
When choosing a CDSS, make sure to align your decision with the specific needs of your healthcare organization. Consider factors like the system’s ability to seamlessly integrate with healthcare management systems. Prioritize a CDSS that offers customizable features to adapt to your unique clinical workflows and protocols.
Look for a user-friendly interface that ensures easy adoption among healthcare professionals. Scalability, vendor support, compliance with regulatory standards, and a comprehensive evaluation of cost-effectiveness should all play a role in your decision-making process.
Building a Custom CDSS with Jelvix
The development and integration of clinical decision support systems into healthcare infrastructure is a complex but essential task aimed at enhancing patient outcomes.
The Jelvix team offers expertise in developing tailored clinical solutions to meet the specific needs of healthcare organizations. Our process involves a deep understanding of client requirements, designing user-friendly interfaces, implementing advanced safety algorithms, and ensuring compliance with healthcare regulations.
In case you need a consultation on developing a custom CDSS, contact our team. They will provide you with advice taking into account your specific needs and business goals.
Need a qualified team of developers?
Access the talent pool to scale your team capacity.