Mental healthcare has never been more vital or more digital. When COVID-19 came, the world woke up to a deafening crisis: soaring mental health problems, struggling healthcare providers, and a desperate need for improved systems. As a result, there has been a growing demand for mental health practice management software, with one solution taking the lead: Electronic Health Records (EHR) software for behavioral health.
Mental health EHR software is designed to meet the complexities of behavioral care, from private therapy notes to multidisciplinary treatment plans. These solutions represent more than a trend. They are now becoming the standard for mental health providers, allowing them to deliver faster, more personalized, and more streamlined care than ever before.
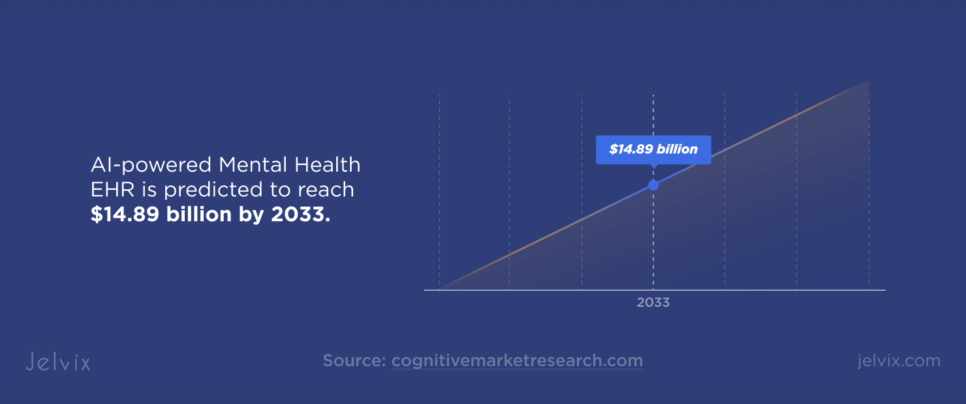
The move to digital is not slowing down. The worldwide EHR market is expected to reach $52 billion by 2033. This growth is driven by the mental health industry, with AI-powered solutions predicted to reach $14.89 billion by 2033, with an impressive 32.1% CAGR.
What’s driving this surge?
- More Mental Illness Cases Than Ever: Rates of depression and anxiety have never been higher.
- Provider Burnout: Mental health software is needed to reduce the burden on therapists and clinicians by streamlining workflows and eliminating unnecessary admin overload.
- Higher Patient Expectations: Remote care, digital prescriptions, and AI-driven diagnostics have gone from being viewed as distant and futuristic to being seen as the bare minimum.
Mental health EHR systems are rapidly being adopted, raising the following questions: What is an EHR, and how does it fit into modern healthcare? In this guide, we’ll examine the essential features of mental health EHR systems, how they improve the quality of care for patients and providers, and some of the major obstacles organizations encounter when implementing them.
A Brief Overview of EHR Software for Mental Health Organizations
EHR systems are essential to the future of healthcare—but not all solutions are the same. Mental health EHR providers build tools tailored to behavioral healthcare that are not embedded within traditional medical records. General software focuses on lab results, prescriptions, and routine checkups, while mental health EHRs prioritize therapy notes, treatment plans, crisis management, and long-term behavioral tracking.
Another key difference is how EHR mental health solutions address documentation and privacy. Therapists and psychiatrists depend on long, deeply personal notes about patients with varying degrees of confidentiality. While general healthcare environments share a single patient record across multiple specialists, mental health EHR systems often have a granular access system, allowing only certain providers to view certain documents.
In addition to confidentiality, mental health EHR platforms for mental health providers streamline workflows by automating administrative tasks, integrating teletherapy options, and providing built-in billing and compliance tools for managing insurance claims and regulatory requirements. They also improve patient progress by measuring it over time, informing data-driven healthcare decisions, and facilitating coordination between psychiatrists, therapists, and case managers.
Key Features of Mental Health EHR Software
When implemented well, EHR systems for mental health providers are not just a repository for patient data but also a system that changes the experience of delivering behavioral healthcare. Whether enhancing clinical efficiency or facilitating data-driven decision-making, these platforms come with features that cater to the distinct demands of mental health professionals and their patients. Let’s examine how they function in practice.
Specialized Templates for Behavioral Health
Mental health documentation is far more complex than the 10-minute checkup summary you might get at a general practitioner’s office. This is why mental health EHRs already come with built-in, specialized templates tailored for behavioral health specialists.
- Cognitive Behavioral Therapy (CBT) Frameworks: Providers can define thought patterns, behavioral triggers, and coping strategies with structured templates;
- Psychiatric Evaluation Tools: Combined symptom scales and screening questionnaires (such as PHQ-9 to evaluate depression or GAD-7 to identify anxiety) monitor patient outcomes over time;
- Trauma-Informed Care Documentation: Providers document sensitive patient histories while enforcing strong access controls.
These structured yet flexible templates make clinical documentation more efficient while preserving the personalized nature of mental health care.
Telehealth Integration
The days of accessing mental health services through in-person visits are over. Telehealth integration has become a necessary feature of mental health EHR software, enabling video consultations, remote patient monitoring, and appointment scheduling for virtual sessions in one application.
For many patients with anxiety, those with mobility problems, and people who live far away, telehealth is an essential bridge to therapy and medication without having to travel. For providers, telehealth baked into their EHR means easier record-keeping, more effortless follow-ups, and better patient engagement.
Secure Patient Communication Tools
As it’s known, therapeutic work does not only happen in the therapy session. Mental health care is highly personal, and patients deserve a safe, private way to communicate with their providers between sessions. That’s where encrypted messaging and patient portals can help.
However, emails or text messages are not secure or compliant with sensitive patient conversations. Modern EHR systems for mental health providers include HIPAA-compliant communication tools that can do more than just message back and forth.
- Secure patient portals, where patients can privately message their therapists, request prescription refills, and review treatment notes;
- Self-evaluations are guided by a therapist who lets patients enter weekly reports of their symptoms, sleep cycles, and medication reactions;
- Digital journaling tools, integrated with the EHR, allow patients to log thoughts and emotions. These become valuable resources for therapists to analyze the progress.
These features promote ongoing engagement, which can lead to increased treatment adherence, early detection of symptoms, and improved patient well-being.
Compliance with Industry Standards
Mental health records contain some of the most sensitive data in healthcare. This means compliance isn’t optional—it’s mandatory. A robust mental health EHR must adhere to:
- HIPAA (Health Insurance Portability and Accountability Act): Protects patient privacy and prevents unauthorized data access;
- ONC Certification (Office of the National Coordinator for Health IT): Ensures EHRs meet federal functionality, security, and interoperability guidelines;
- HITECH Act (Health Information Technology for Economic and Clinical Health): Strengthens data security and promotes the use of electronic health records;
- 42 CFR Part 2: Adds extra protection for substance use disorder treatment records, ensuring only authorized providers can access these files.
A mental health EHR system that meets these standards gives providers and patients peace of mind, knowing their data is secure, legally compliant, and protected from breaches.
Advanced Reporting and Analytics
Data transforms mental health care, but raw information is useless without the right analysis tools. This is precisely why modern EHR platforms should be equipped with:
- Predictive analytics, which can note potential patient crises based on historical trends and the worsening of symptoms;
- Behavioral health outcome tracking, using AI to assess long-term treatment effectiveness across different demographics;
- Operational efficiency dashboards allow clinic administrators to pinpoint workflow bottlenecks and learn how to deliver better service.
For mental health providers, a modern EHR system is not simply software. It is a clinical partner working to streamline workflows, improve patient engagement, and enhance security. These platforms redefine how behavioral health professionals provide care by incorporating specialized documentation tools, real-time analytics, and robust communication channels.
Use Cases of Mental Health EHR Software
With the features we just covered and the definitions learned, it’s time to uncover how this technology translates into tangible improvements in patient outcomes and clinical efficiency. Let’s explore real-world scenarios where EHR for therapists and behavioral health organizations does wonders.
Streamlining Therapy Practices
For doctors in private practice, managing multiple patients, tracking progress, and handling administrative tasks can be overwhelming. EHR for therapists simplifies the process by:
- Automating appointment scheduling and sending reminders to reduce no-shows;
- Providing structured therapy notes that allow practitioners to track patient progress over time;
- Facilitating teletherapy sessions with built-in video conferencing and secure messaging.
For instance, a licensed therapist who specializes in anxiety disorders said that an EHR for therapists reduced her paperwork, allowing her to see more patients without burning out. Secure patient messaging also enabled her to provide additional support between visits, increasing engagement and treatment adherence.
Enhancing Behavioral Health Clinics
At the clinic level, mental health professionals need an EHR accommodating team-based care. An integrated and connected behavioral health EHR software guarantees:
- Smooth collaboration of therapists, psychiatrists, and case managers;
- Tools that help manage medication and avoid errors in prescribing;
- Patient risk assessment features that aid providers in flagging early warning signs of crises.
Consider, for example, a mental health clinic that treats patients with PTSD. Shared in real-time, an EHR for mental health makes it easy for the clinic’s team to see a patient’s records and create holistic treatment options. Optimizing their approach to therapy, AI-powered analytics help them discover which methods have the highest success rates.
Crisis Intervention & Suicide Prevention Centers
Mental health emergencies require fast, coordinated responses. EHR systems help crisis intervention teams by:
- Providing instant access to patient history, allowing responders to make informed decisions;
- Automating referrals to inpatient facilities, ensuring patients receive the proper care quickly;
- Tracking follow-ups and ongoing support, reducing the risk of relapse.
Large Hospital Networks
For hospitals and large healthcare systems, integrating EHR for mental health with general medical records is crucial. This allows:
- Primary care doctors and psychiatrists to share information;
- AI-driven analytics to predict mental health deterioration;
- Compliance with strict mental health data privacy laws.
For example, a regional hospital implemented an AI-powered mental health EHR module, which flagged at-risk patients and helped decrease readmissions. This proactive intervention saved costs and improved long-term patient outcomes.
Technology Trends in Mental Health EHR Software
Mental health EHR software is evolving beyond simple data management. Now, it’s a proactive tool that augments care, anticipates crises, and tailors to patients’ needs. Predictive analytics powered by AI are changing the face of mental health care by identifying patterns that may have gone undetected previously. Rather than relying on clinician observations alone, AI-augmented EHR systems mine through therapy notes, medication adherence, sleep patterns, and — owing to their direct access to patient data — even patient-reported mood logs to highlight potential vulnerabilities.
Some systems employ sentiment analysis to detect subtle shifts in the language of someone that might indicate worsening depression or suicidal ideation. Using machine learning, providers can intervene sooner, focusing on those most at risk and preventing emergency admissions to the hospital.
In addition to AI, wearable devices and IoT-based technology are revolutionizing mental health observation. Many mental health conditions manifest as physiological changes, such as irregular sleep, higher heart rate variability, and lags in activity. Smartwatches, EEG headbands, and stress sensors can now be directly integrated into EHR systems, providing real-time insight into a patient’s state of being.
Some clinics have even started using wearable data to predict PTSD episodes in veterans, allowing for preemptive interventions before symptoms escalate. These integrations bolster provider decision-making and grant patients tangible feedback as they track their mental health progress.
As more mental health services are conducted online, the on-demand, scalable nature of cloud-based EHR solutions has become a necessity. On-premise systems can be costly to maintain, slow to expand, and difficult to work remotely with. In these instances, cloud-based platforms mitigate these challenges by allowing providers to securely access patients’ records from any device, whether working on in-person sessions or telehealth appointments. Seamless updates minimize the burden of meeting HIPAA and other evolving data privacy regulations, while a scalable architecture grows with behavioral health networks.
Factors Defining the Success of EHR Software for Mental Health
The success of EHR for mental health providers hinges on three key factors:
- User-friendly design;
- Seamless integration with existing systems;
- Ongoing support and updates.
A well-designed system will empower providers to document sessions quickly, access the histories of patients smoothly, and use the platform without excess clicks or confusion. An intuitive EHR allows therapists to spend less time in the administrative aspect of therapy and more time in direct patient engagement, improving efficiency and reducing clinician burnout.
It’s not just usability that matters; seamless integration ensures a smooth workflow. Mental healthcare is often a team effort involving professionals ranging from therapists and psychiatrists to case managers and primary care physicians. When an EHR does not sync with telehealth platforms, billing systems, e-prescribing tools, and a wider network of hospitals, it creates inefficiencies that disrupt care coordination. A well-functioning mental health EHR must facilitate real-time data sharing between various platforms so that patient information is consistently current.
Nevertheless, every carefully designed and integrated system requires ongoing support and periodic updates to function correctly. Healthcare regulations change, best practices evolve, and technology improves—an EHR that doesn’t keep up quickly becomes obsolete. Vendors providing frequent security updates, new feature rollouts, and compliance improvements allow mental health providers to continue providing quality care without interruption.
Also, having responsive support is essential. Clinicians require rapid conclusions when problems occur to avoid compromising patient care. Top EHR providers don’t stop at selling you the software: they provide a partnership that encompasses training and services, all of which are aimed at helping you adjust, troubleshoot, and continually improve your system by providing the necessary feedback based on your experience.
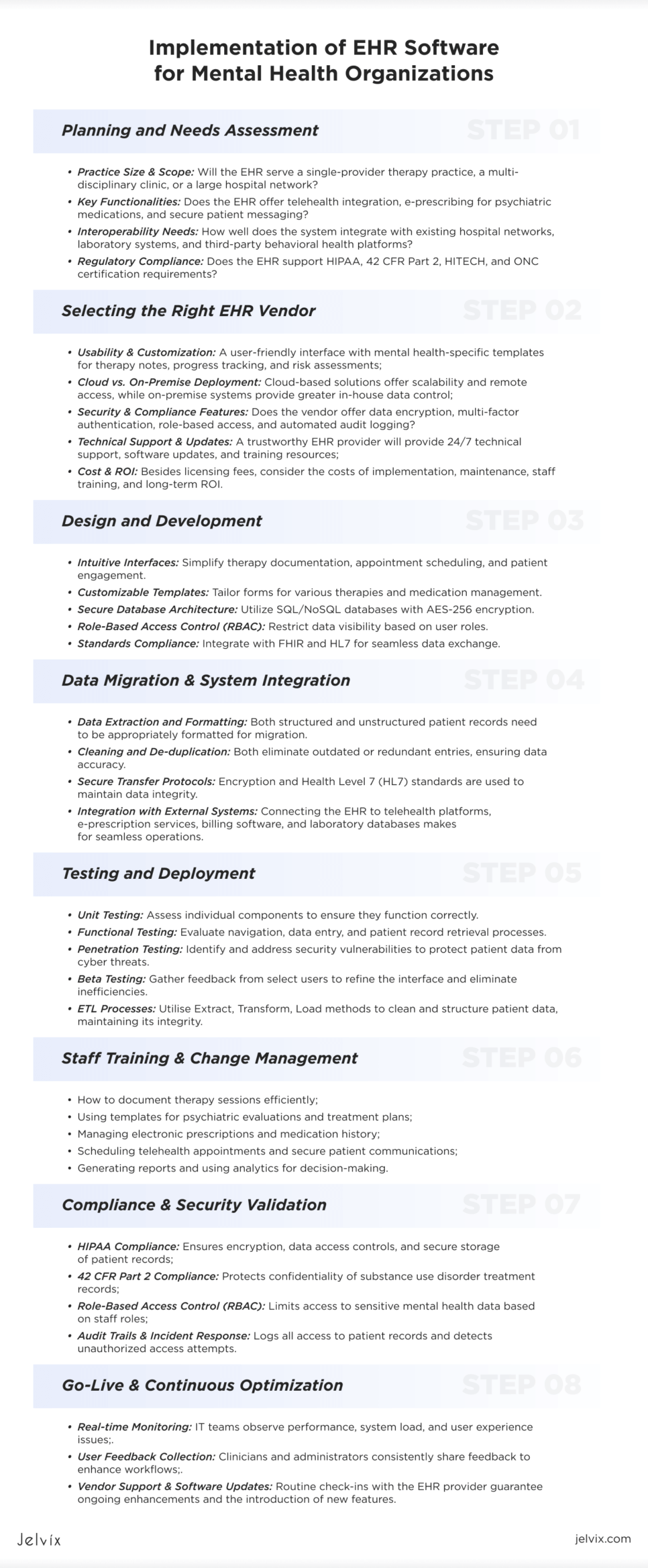
Implementation of EHR Software for Mental Health Organizations
Proper planning and staff training are needed to customize the implementation. Such systems in mental health organizations must follow a detailed framework, which includes planning, data migration, customization, training, compliance validation, and continuous optimization.
Step 1: Planning and Needs Assessment
Prior to choosing an EHR for mental health, organizations must evaluate their particular needs. There are four main things to consider:
- Practice Size & Scope: Will the EHR serve a single-provider therapy practice, a multi-disciplinary clinic, or a large hospital network?
- Key Functionalities: Does the EHR offer telehealth integration, e-prescribing for psychiatric medications, and secure patient messaging?
- Interoperability Needs: How well does the system integrate with existing hospital networks, laboratory systems, and third-party behavioral health platforms?
- Regulatory Compliance: Does the EHR support HIPAA, 42 CFR Part 2, HITECH, and ONC certification requirements?
At this point, input from stakeholders is essential. Involving clinicians, IT staff, and administrative personnel ensures that the EHR solution meets practical operational needs.
Step 2: Selecting the Right EHR Vendor
Once organizational requirements are defined, selecting the right EHR for therapists and mental health providers becomes the next priority. Key evaluation criteria include:
- Usability & Customization: A user-friendly interface with mental health-specific templates for therapy notes, progress tracking, and risk assessments;
- Cloud vs. On-Premise Deployment: Cloud-based solutions offer scalability and remote access, while on-premise systems provide greater in-house data control;
- Security & Compliance Features: Does the vendor offer data encryption, multi-factor authentication, role-based access, and automated audit logging?
- Technical Support & Updates: A trustworthy EHR provider will provide 24/7 technical support, software updates, and training resources;
- Cost & ROI: Besides licensing fees, consider the costs of implementation, maintenance, staff training, and long-term ROI.
In-depth vendor demos and trial periods allow organizations to test the EHR’s functionality in realistic scenarios before implementing it.
Step 3: Design and Development
In the design phase, attention is paid to intuitive interfaces that simplify therapy documentation, appointment scheduling, and patient engagement. Developers collaborate with UX/UI experts who design a clean and uncluttered dashboard that enables therapists and administrators to access progress notes, risk assessments, and treatment plans with a few clicks. Customizable templates are essential, allowing providers to tailor forms for CBT, DBT, trauma-informed care, or medication management.
On the backend, a secure database architecture is essential. Patient records are stored in SQL or NoSQL databases, and advanced encryption protocols (AES-256) keep data confidential. Role-based access control (RBAC) limits data visibility based on user roles—therapists, for example, only see their assigned patients, and compliance officers handle audit logs. Engineers also work with FHIR (Fast Healthcare Interoperability Resources) and HL7 standards to facilitate the free flow of data with hospital networks, pharmacy systems, and telehealth platforms.
Step 4: Data Migration & System Integration
One of the most pivotal and time-intensive stages of the implementation process is migrating patient data from legacy systems, paper records, or prior EHRs. The process involves:
- Data Extraction and Formatting: Both structured and unstructured patient records need to be appropriately formatted for migration.
- Cleaning and De-duplication: Both eliminate outdated or redundant entries, ensuring data accuracy.
- Secure Transfer Protocols: Encryption and Health Level 7 (HL7) standards are used to maintain data integrity.
- Integration with External Systems: Connecting the EHR to telehealth platforms, e-prescription services, billing software, and laboratory databases makes for seamless operations.
Given this, many organizations will run parallel systems during the transition period to validate data accuracy before full deployment and avoid disruption.
Step 5: Testing and Deployment
Once development is complete, extensive testing is required to guarantee stability, compliance, and integration with existing healthcare systems.
It starts with unit testing to check single components and continues with system-wide functional testing of navigation, data entry, and patient record retrievals. Penetration testing is conducted to find security weaknesses and ensure that patient data is not exposed to cyber-attacks.
Organizations do beta testing with select providers before deployment, allowing real-world feedback to hone the interface and remove inefficiencies. ETL (Extract, Transform, Load) processes are best for cleaning and structuring patient data while preserving integrity.
Step 6: Staff Training & Change Management
A successful EHR implementation is also about people using it effectively. Comprehensive training ensures that clinicians, therapists, and administrators understand:
- How to document therapy sessions efficiently;
- Using templates for psychiatric evaluations and treatment plans;
- Managing electronic prescriptions and medication history;
- Scheduling telehealth appointments and secure patient communications;
- Generating reports and using analytics for decision-making.
Change management strategies, such as super-user training and phased rollouts, can reduce resistance and improve adoption rates. Hands-on workshops and EHR simulation environments help staff gain confidence before using the system with actual patients.
Step 7: Compliance & Security Validation
Before full deployment, an EHR system must be validated for:
- HIPAA Compliance: Ensures encryption, data access controls, and secure storage of patient records;
- 42 CFR Part 2 Compliance: Protects confidentiality of substance use disorder treatment records;
- Role-Based Access Control (RBAC): Limits access to sensitive mental health data based on staff roles;
- Audit Trails & Incident Response: Logs all access to patient records and detects unauthorized access attempts.
Security testing, including penetration testing and vulnerability assessments, ensures the system resists breaches and cyber threats.
Step 8: Go-Live & Continuous Optimization
It’s time to go live once the system is fully integrated and tested. Many organizations start with a soft launch, during which only a portion of the staff uses the EHR before full deployment.
- Real-time Monitoring: IT teams observe performance, system load, and user experience issues;
- User Feedback Collection: Clinicians and administrators consistently share feedback to enhance workflows;
- Vendor Support & Software Updates: Routine check-ins with the EHR provider guarantee ongoing enhancements and the introduction of new features.
Post-implementation, organizations should continuously optimize EHR workflows based on performance data and evolving clinical needs.
When To Choose Custom Mental Health EHR
A custom mental health EHR is built around an organization’s needs and doesn’t have the limitations associated with generic solutions. Unlike off-the-shelf software, it is designed to integrate seamlessly with telehealth, hospital networks, pharmacies, and credentials databases—without the risk of incompatibility.
Another benefit is security. Developers ensure that the custom EHR meets stringent compliance requirements by providing fine-grained access controls to sensitive data, patient consent management, and advanced encryption, keeping sensitive data safe. They also simplify navigation by removing bloated features, allowing therapists, psychiatrists, and case managers to do their work faster.
Finally, a custom EHR grows with the organization, evolving as more services, users, or compliance requirements are added. Unlike vendor-restricted solutions, it does not require expensive upgrades or built-in licensing constraints.
With all the advantages considered, a custom EHR for mental health is ideal when:
- Your organization requires highly specialized documentation, workflows, or compliance measures.
- You need seamless interoperability with existing systems.
- You’re growing rapidly and need a scalable solution.
- Your practice has experienced workflow inefficiencies due to limitations in commercial EHR software.
- You want complete control over security, compliance, and data privacy without relying on third-party vendors.
While off-the-shelf solutions work for many smaller practices, mental health organizations with unique needs or long-term growth plans will benefit significantly from a custom-built EHR.
The Smart Way to Choose – Download Your Guide to Selecting the Right Healthcare Tech Partner!

Challenges and Solutions in Mental Health EHR Software
Data Security & Privacy Concerns
Mental health records are highly sensitive and require stronger privacy protections than standard medical data. Regulations require tight controls on who can view patient information and how it can be disseminated. A single security lapse can result in data breach incidents, legal sanctions, and loss of patient trust.
Possible solutions include implementing the following:
- End-to-End Encryption;
- Role-Based Access Control (RBAC);
- Audit Logs & Real-Time Monitoring;
- Secure Patient Communication Channels.
Discover how we developed a personalized EHR system that optimized the clinic’s workflow while ensuring maximum privacy and security.
Interoperability Issues with Other Healthcare Systems
Many off-the-shelf EHRs don’t communicate well with hospital networks, pharmacy databases, or billing systems outside their operations. This data fragmentation creates inefficiencies, resulting in duplicate records, manual data entry mistakes, and delays in treatment coordination.
Solution:
- HL7 & FHIR Standards Compliance: Ensures mental health EHRs can exchange data seamlessly with hospital networks and government health registries;
- Custom API Integrations: Allows mental health EHRs to communicate with third-party applications such as lab, telehealth, and e-prescribing tools;
- Cloud-based systems allow real-time data synchronization across various sites, making patient records highly available across different providers without lags.
Resistance to Adoption Among Staff
Unfortunately, EHRs often face widespread adoption issues within the mental health space. These issues stem from difficult-to-navigate interfaces, disrupted workflows, and a steep learning curve. Some staff members prefer paper records or fear technology will interfere with patient interactions.
Solution:
- User-Friendly Design: A thoughtfully developed EHR will reflect existing workflows rather than require clinicians to modify their practice;
- Phased Rollout Strategy: Introduces the system gradually, allowing staff to adapt in stages rather than all at once;
- Super-User Training Model: Identifies tech-savvy team members to lead training sessions and provide peer support;
- Automated Documentation Tools: Automation features such as voice-to-text note-taking and AI-assisted templates help ease the documentation burden, making the EHR more of a time-saver than a time-waster.
Mental health EHR software must balance security, interoperability, and ease of use to be truly effective. Strong data protections, smooth system integrations, and careful training can alleviate adoption challenges and help providers realize the full potential of digital tools in establishing better pathways to improved patient care.
Best Practices for Mental Health EHR Software
As we discussed, regular updates ensure security, compliance, and interoperability. Keeping up with HIPAA, 42 CFR Part 2, and AI-driven tools helps mental health EHRs stay efficient, scalable, and patient-friendly.
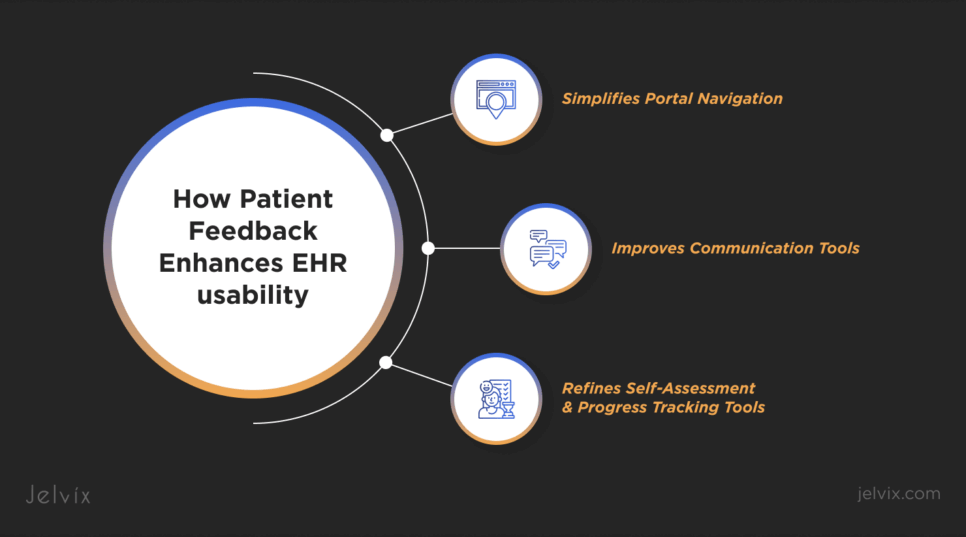
When talking about “patient-friendly,” though, their feedback usually goes unnoticed. While EHR software is designed for providers, patients interact with it through portals, telehealth services, appointment scheduling, and secure messaging. If these tools are confusing or difficult to use, patient engagement drops, affecting treatment adherence.
How patient feedback enhances EHR usability:
- Simplifies Portal Navigation: Patients may struggle to find past therapy notes, request medication refills, or book follow-up sessions. Regular feedback helps refine UI/UX design for a more intuitive experience.
- Improves Communication Tools: Gathering feedback ensures that messaging features remain seamless and convenient.
- Refines Self-Assessment & Progress Tracking Tools: Patients engaging with mood logs, therapy homework, or AI-driven self-help tools should find them practical and relevant. Feedback helps improve content and engagement strategies.
Organizations prioritizing these best practices will be certain that their EHR remains a valuable tool for providers and patients, supporting high-quality mental health care for years to come.
Signs Your Behavioral Health EHR Solution Needs an Upgrade
An outdated EHR for mental health can slow down workflows, create compliance risks, and frustrate staff and patients. If your system lacks integration, usability, or security, an upgrade could be your next step forward.
One red flag is if features are outdated or if the EHR is not interoperable with newer technologies like telehealth platforms, AI-driven analytics, and wearable device integrations. When the EHR doesn’t sync with external systems, providers spend unnecessary time on manual data entry, increasing the risk of errors and inefficiencies.
Another significant issue is growing complaints from staff and patients about slow load times, complex navigation, or poor patient portal functionality. A good EHR for therapists should streamline workflows, not complicate them.
Lastly, organizations that fail to comply with updated regulations such as HIPAA, 42 CFR Part 2, or ONC standards become more vulnerable to legal penalties, data breaches, and ransomware. Missing security updates or failing audits is an obvious sign that your system isn’t keeping pace.
If your current EHR slows you down, frustrates your staff, or puts compliance at risk, it’s time to change. Whether you require a solution built around your practice’s unique needs or a smarter way to harness new technologies, Jelvix can help. Our experts work with mental health professionals and organizations to find or develop the right EHR that fits your workflow, scales with your growth, and enhances care quality. Contact Jelvix for a consultation today and make your next step to a better mental health EHR!
FAQ
What is mental health EHR software?
Mental health EHR software is an electronic system that helps mental health professionals manage their documentation and treatment plans. It supports tasks like patient intake, notes on therapy sessions, medication tracking, and reporting, all designed for the specific needs of mental health practices.
What is the difference between EHR and EMR for mental health providers?
EHRs and EMRs help manage patient information. However, EHRs offer more complete details about a patient’s medical history from various providers. This makes EHRs better for mental health professionals who need to work with other healthcare providers.
How does an EHR improve patient engagement in mental health care?
Mental health electronic health records frequently feature patient portals for individuals to schedule appointments, view treatment plans, and communicate securely with their providers. This encourages greater transparency and engagement, which enhances treatment adherence and outcomes.
How does mental health EHR software ensure patient confidentiality?
These systems safeguard sensitive patient information through advanced security techniques, including data encryption, role-based access controls, and adherence to standards like HIPAA and GDPR. Tailored solutions can offer even more precise controls to address unique confidentiality requirements.
Are custom EHR solutions more secure than ready-made options?
Custom EHRs frequently offer advanced security options customized to meet your organization’s specific compliance requirements, such as HIPAA or GDPR. With control over the system architecture, you can implement high-level encryption, access controls, and other security measures that generic platforms may not provide.
Need a qualified team of developers?
Reach top talent pool to handle end-to-end delivery of your project.