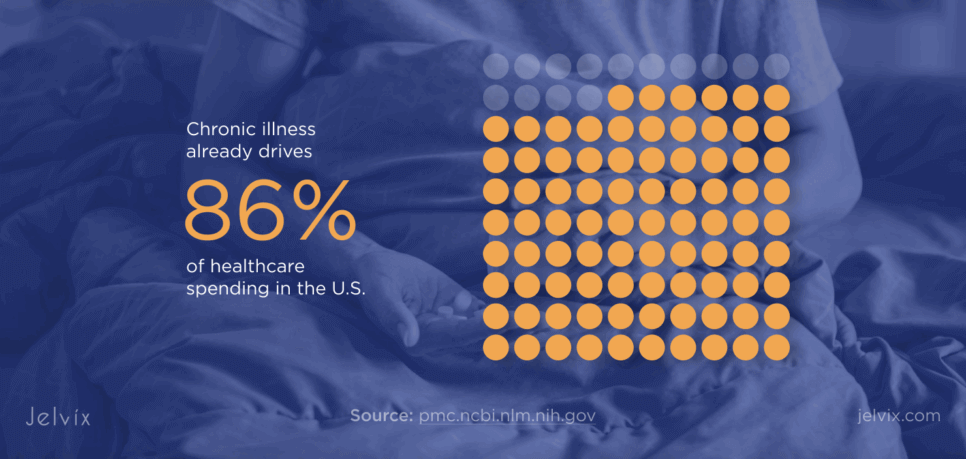
As chronic illnesses drive most U.S. healthcare spending, CCM medical billing is fast becoming the linchpin of scalable care coordination. As stated in the research Chronic Disease Prevalence in the US, with 42% of adults managing two or more chronic conditions and over 12% dealing with five or more, the pressure on care teams continues to grow. According to Halsted R Holman, chronic illness already drives 86% of healthcare spending in the U.S., and with the over-50 population with chronic conditions expected to double by 2050, demand for long-term, coordinated care will only increase.
To respond, CMS introduced the CCM program to reimburse primary care providers for delivering consistent, proactive, and personalized care to Medicare beneficiaries, improving outcomes while reducing unnecessary ER visits and hospitalizations.
But there’s a gap between what the program promises and what most platforms deliver. Despite clear billing codes and generous reimbursements, chronic care management billing often fails.
Medical software development plays a crucial role here—without robust integration frameworks, RPM and IoT devices generate data that never reaches care teams. Task documentation gets lost across siloed EHRs. Shared accountability breaks down without real-time updates. And when billing depends on tracking CPT time precisely and producing airtight audit trails? Manual workarounds are a recipe for denials. This article breaks down where these bottlenecks start, how integration can eliminate them, and what CPOs can do to build scalable billing systems from the ground up.
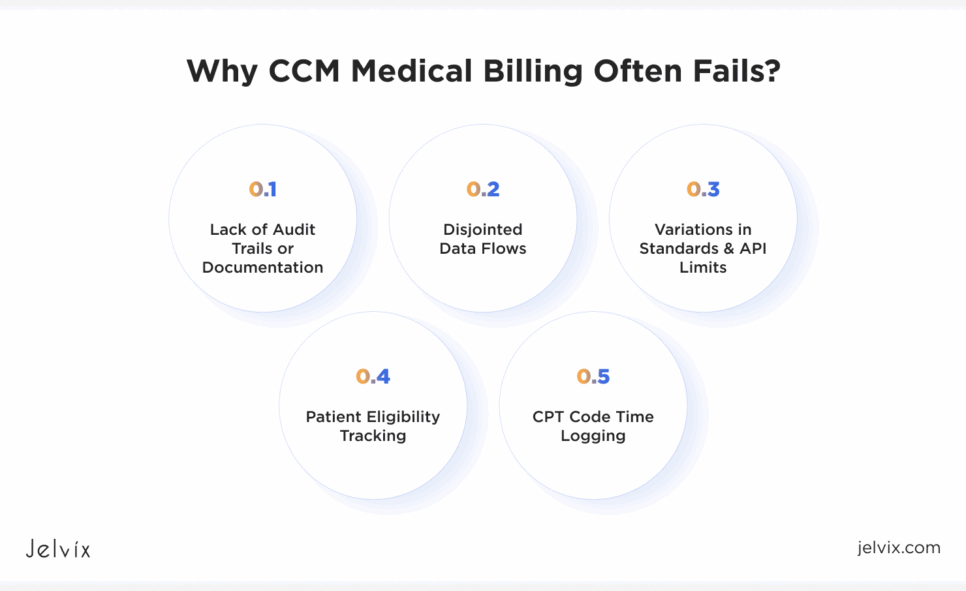
Why CCM Medical Billing Often Fails
The CCM medical billing doesn’t fail due to complexity; it fails due to the fact that the systems behind it cannot communicate. When patient-generated RPM or IoT data doesn’t flow into the EHR (Electronic Health Record) and data from labs, specialists, and care plans exist in silos, billing teams encounter a disjointed landscape of information that must be pieced together.
Here are the most common failure points, laid out clearly:
- Patient eligibility tracking: Without integrated data, demographics, chronic conditions history, consent, platforms fail to flag eligible patients.
- CPT code time logging: Manual entry or siloed task logs make it hard to accurately track the 20–60 minutes per month required by CMS.
- Disjointed data flows: Fragmented health records across EHRs, labs, RPM devices, and external specialists disrupt billing continuity.
- Lack of audit trails or documentation: Billing claims fail without traceable care logs and accurate documentation of services rendered.
- Variations in standards & API limits: HL7, FHIR, and legacy EHRs rarely align, making data sharing slow, incomplete, and error-prone.
At the heart of these breakdowns is a lack of clinical interoperability: the seamless, secure exchange and usage of electronic health data across systems. There are three levels to this:
- Foundational: One system can send data to another, but that’s it. No guarantee it’ll be useful.
- Structural: The data is formatted consistently (like having all vitals in the right columns), but systems might still not know what it means.
- Semantic: Systems not only receive and read the data, but actually understand it—so they can use it for things like care planning, CPT code tracking, and eligibility checks.
By reframing these challenges through the lens of integration and clinical interoperability, we’ll next uncover how automation and platform architecture can directly solve each bottleneck, restoring revenue flow and scaling care coordination.
How Chronic Care Platforms Can Move from Manual Chaos to Seamless Claims
Manual workflows are the silent killer of billing for chronic care management. Every step is vulnerable to human error and system disconnects. These gaps create billing inconsistencies that delay reimbursement, trigger denials, and eventually eat into the margins that chronic care programs are designed to protect.
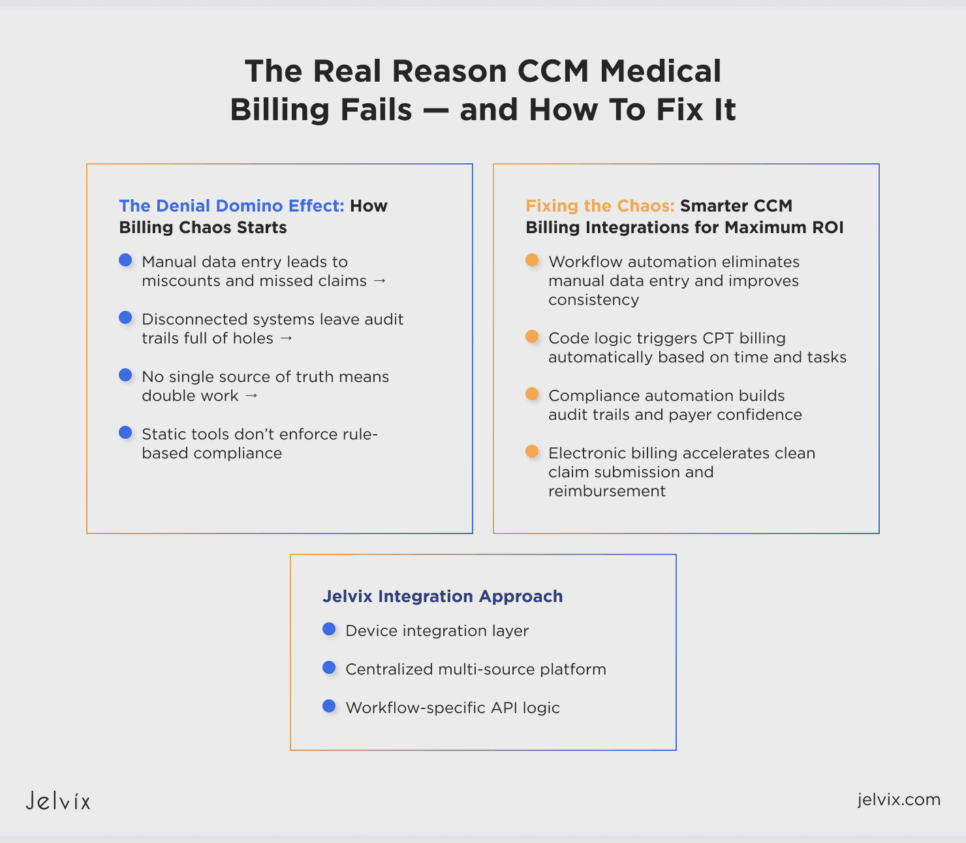
The Denial Domino Effect
Let’s break down how the chaos happens:
- Manual data entry leads to miscounts and missed claims.
CPT codes 99490, 99439, and 99487 require detailed time tracking (20+ minutes per month of care coordination). When teams use spreadsheets, email threads, or phone logs to capture time, that data is often incomplete or incorrectly rounded. This leads to underbilling or audit flags.
- Disconnected systems leave audit trails full of holes.
If RPM data is in one dashboard, care notes in another, and patient interactions scattered across tools, there’s no centralized audit trail. That’s a compliance red flag. And without timestamped, traceable documentation, payers have grounds to reject claims.
- No single source of truth means double work.
When task data lives in multiple systems (EHR, practice management software, third-party tools), staff must manually consolidate records for billing. This increases labor costs and the likelihood of errors. A single misplaced decimal or CPT code mismatch can cause cascading billing failures.
- Static tools don’t enforce rule-based compliance.
Without logic-based automation that enforces CMS billing criteria (like verifying consent, checking chronic conditions, ensuring minimum time thresholds), medical billing teams rely on memory or worse, guesswork.
Summary: Manual billing failure points:
- Manual Entry: Time tracking errors, CPT mismatches.
- Missing Trails: No centralized documentation = denials.
- Disconnected Tools: Multiply staff workload, reduce accuracy.
- No Compliance Guardrails: No automation = CMS criteria missed.
Solving these medical billing challenges starts with smarter systems. That means replacing manual workarounds with integration that enforces medical software compliance rules, connects every data source, and produces billing-ready records without extra steps. The next part of this guide explores how medical software compliance integration can deliver that level of precision.
Chronic Care Management Without the Bottlenecks
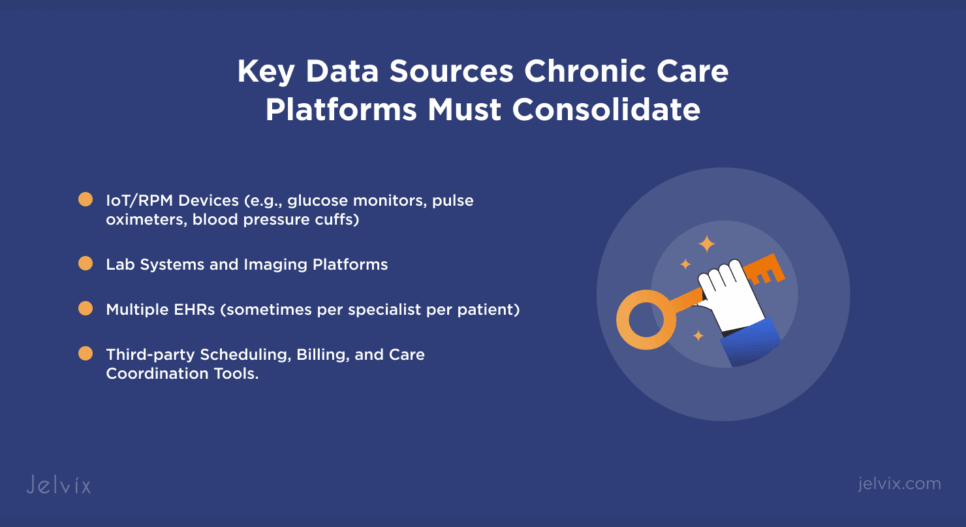
Chronic care platforms supporting diverse specialties must consolidate data from:
- IoT/RPM devices (e.g., glucose monitors, pulse oximeters, blood pressure cuffs);
- Lab systems and imaging platforms;
- Multiple EHRs (sometimes per specialist per patient);
- Third-party scheduling, billing, and care coordination tools.
This is further exaggerated when applied across chronic disease areas, as each condition introduces different care workflows, data sources, and billing sensitivities. The control of heart disease and stroke through RPM depends strongly on the quick delivery of vital information from such devices; however, slow syncing or gaps in data can make platforms miss CPT time thresholds required by CMS. When combined with the lab results, imaging data, and longitudinal treatment plans that are made all the more complex due to siloed systems from a variety of stakeholders, cancer care becomes even more complex.
Discover how seamless EHR, IoMT, and lab integrations transformed chronic care management —cutting integration time in half and freeing up product teams to innovate.
Typically, daily glucose readings and monthly consultations for diabetes management are not consolidated in a single record, which hinders precise care logging. Chronic respiratory diseases such as COPD often include data from pulse oximeters or inhaler sensors, devices that are frequently operating outside the core EHR systems. The other example we would give is even arthritis care, which crosses multiple specialties, but still falters when integrated documentation and shared task tracking fail.
The solution to these issues is purpose-built EHR integration layers that standardize input, validate eligibility rules, and automatically update care plans in sync with medical documentation. This approach directly reduces CCM claim denials with EHR integration logic that ensures every claim is defensible.
Take cancer care, for example. A successful FHIR integration solution implemented by Jelvix allowed oncology teams to access structured clinical data (e.g., genomic, imaging, lab results) across vendors. That same model can power chronic disease platforms too, streamlining care planning, compliance, and billing.
Boosting ROI with Smarter CCM Billing Integration
Modern chronic care platforms are now asking: how can I improve healthcare workflow automation in a hospital or clinic without hiring more billing staff or rewriting EHR integrations from scratch?
The answer lies in tightly embedded billing logic within clinical workflows. Systems that automatically detect eligibility, assign CPT codes based on logged activity, and update care plans in real-time remove the manual bottlenecks that typically slow or deny reimbursement.
Here’s how it works:
- Eligibility detection automation: Once a patient’s chronic conditions and CMS consent forms are verified, the platform flags them for monthly CCM billing.
- Auto-code assignment: When task completion logs hit 20, 40, or 60-minute thresholds, the system dynamically maps those to CPT 99490, 99439, or 99487.
- Live care plan sync: Task updates, clinical notes, and device data are all written back to the EHR.
- Electronic billing submission: Completed claims are assembled and submitted via direct payer integration or clearinghouses, improving cash flow and lowering rejection rates.
Beyond speed and accuracy, smarter integration ensures medical billing compliance automation. Audit logs are updated not in retroactive batches but continuously. Task ownership is tracked per user. And billing eligibility is tied directly to CMS rules.
Summary: Smarter CCM billing integration ROI
- Workflow automation eliminates manual data entry and improves consistency.
- Code logic triggers CPT billing automatically based on time and tasks.
- Compliance automation builds audit trails and payer confidence.
- Electronic billing accelerates clean claim submission and reimbursement.
Next, we’ll break down the exact metrics product leaders can track to benchmark these gains, from claim accuracy to staff hours saved.
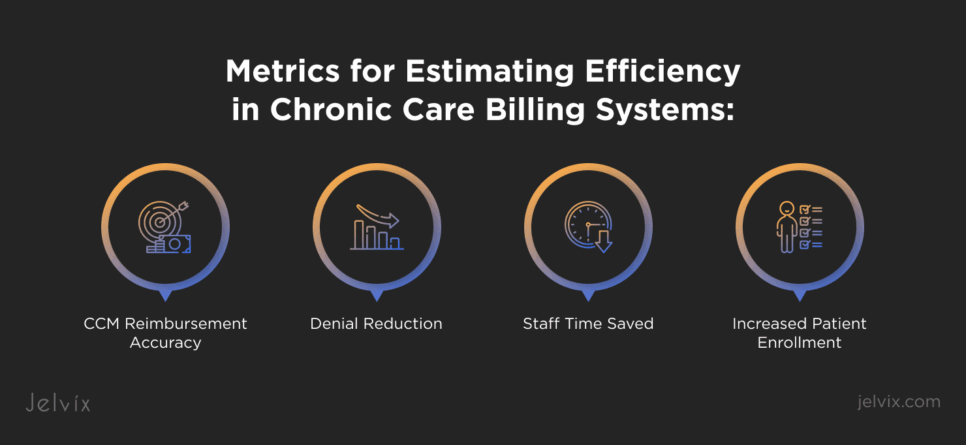
Metrics That Matter for CPOs: Estimating Efficiency in Chronic Care Billing Systems
CCM Reimbursement Accuracy
Measure the ratio of approved to submitted claims, weighted against total claim volume. For systems that have EHR integrations built in and automated CPT mapping, you can expect reimbursement accuracy to top 98% every time. The only variations stem from inaccurate data mapping, incompatible forms of FHIR resources, or delays in updating APIs to new specs—all issues that can be addressed through a focused FHIR integration strategy.
Denial Reduction
Track both the absolute denial rate and the root-cause distribution. Platforms are seeing denial reductions in the first year of utilizing real-time eligibility checks, standards-compliant data models, and bi-directional EHR writeback. It is not merely a billing metric; more realistically, this number reflects how well your system enforces business rules at the workflow level.
Staff Time Saved
Calculate time saved on manual data entry, care plan reconciliation, and post-denial resubmissions. For example, in a well-instrumented chronic care management stack, automation of eligibility detection and electronic billing submission can reduce the administrative load. Healthcare automation workflow telemetry is the key, knowing exactly which elements of the process can be abstracted into API logic without compromising governance.
Increased Patient Enrollment
Monitor enrollment lift as a downstream benefit of operational efficiency. Faster onboarding flows and predictable reimbursement timelines free capacity for providers to enroll more eligible patients.
Why These Metrics Matter for Product Leadership
The KPIs are either read as architectural validation points to CPO, or, to put it simply, these are the operational health indicators. They verify that your integration framework, compliance logic, and workflow automation modules are resulting in clinical value as well as revenue scaling. In other words, they connect the dots between engineering investment and market growth.
Check how a custom app transformed Chronic Disease Management with real-time tracking, telehealth, and streamlined medication workflows.
Jelvix Integration Approach
Connecting endpoints is not enough to scale chronic care management billing. With GDPR and other standards, it needs a robust integration architecture that can handle changing standards, high-volume events, and compliance without slowing things down. The way Jelvix fights this challenge is through structuring an API-first environment where all data flows from device readings to multi-EHR records through a single standards-driven pipeline oriented towards both clinical decision-making and precise medical claims processing.
Device integration layer
Instead of relying on one-off connections for each device, Jelvix builds a dedicated ingestion framework capable of handling diverse IoT and RPM sources. It authenticates securely, reshapes incoming payloads into a normalized format, and streams updates into patient records as events occur.
Centralized multi-source platform
The system consolidates EHR output, lab results, imaging data, and coordination notes in one integration hub. By implementing the FHIR interoperability standard, it aligns data semantics across systems, ensuring that patient records, care plans, and observations are consistently structured.
Workflow-specific API logic
With clean, normalized data in place, the platform applies logic designed for CCM billing workflows. It runs automated eligibility checks against CMS criteria, matches activity logs to the correct CPT codes, and writes updates back into connected EHRs for continuous audit readiness. Claims are generated directly from this verified dataset, passed through clearinghouses with integrated transaction monitoring, and resolved automatically if payers flag issues. The result is a closed feedback loop between clinical activity and medical claims submission, without introducing manual reconciliation steps.
By building in device integration, central interoperability, and workflow logic, Jelvix prevented the lag and data siloing that tends to make scaling chronic care billing prohibitively expensive. The core architecture is still as flexible as new providers, devices, and EHRs can be onboarded without needing to rewrite the foundation.
Integration Audit Checklist
Using best practices from how to improve interoperability in healthcare, this quick diagnostic will help you map your current position:
- Are all EHR, RPM, and lab data streams integrated into a single workflow without manual reconciliation?
- Are FHIR or HL7 standards applied consistently across all endpoints to maintain semantic and structural integrity?
- Does your system automatically detect eligibility, map CPT codes, and update care plans as activities are logged?
- Is your audit documentation updated in real time and fully traceable to clinical actions?
- Can you add a new partner, device type, or EHR connection in weeks rather than months, without disrupting medical claims processing?
If you answered “yes” to all five, you’re operating at a scale-ready stage. Three or four “yes” answers indicate partial readiness, but integration gaps could block revenue growth. Fewer than three means your current architecture isn’t ready to handle scaling, and new features will only add operational strain.
Knowing your stage is the first step toward building the interoperability backbone your platform needs to scale without breaking.
Summary
CCM medical billing fails less from code complexity and more from fragmented data, inconsistent standards, and the inability to coordinate across multiple chronic care programs.
The solution lies in an integration strategy that merges device data, EHR outputs, and lab results into a unified platform. These features include real-time eligibility checks, automated CPT mapping, and continuous audit logging—all aimed at making billing a proactive revenue stream instead of a lag. With FHIR and HL7 standards, workflow-specific API logic, and end-to-end interoperability, billing becomes a predictable revenue stream instead of an operational drain.
Before scaling, evaluate your readiness. Identify where integration bottlenecks clog your reimbursement cycle. Recognize which workflows still depend on manual reconciliation. And then assess how fast you can bring new providers or technologies in without jeopardizing your medical claims flow.
Jelvix specializes in building scalable, standards-compliant interoperability frameworks for healthcare organizations. Our medical software development team experts work with chronic care platforms to develop integration layers for collecting and aggregating all data, billing process optimization, and audit preparedness. At scale!
Ready to scale without breaking your billing? Fill out the form below, and let’s design your integration architecture for long-term success.
Looking for expert developers?
Get a dedicated team focused solely on your project — from kickoff to delivery.