Nowadays, it is very common to hear about the hectic reality of hospitals. In fact, many hospitals in the United States are snowed under work caring for their communities that have medicinal, surgical, and caregiving needs. In addition to this fact, one must take into account the coronavirus (COVID-19) and how it has changed the landscape of hospitalizations.
The Associated Press suggests that due to the dire cases brought on by the COVID-19 pandemic, hospitals across the U.S. experience many inconveniences as a result of paying a lot more attention to COVID patients. So, what does this mean for non-COVID patients? Such inconveniences concerning non-COVID patients include:
- A backlog of cancer screenings;
- Canceled or postponed surgical procedures, AND;
- Shortage of hospital staff.
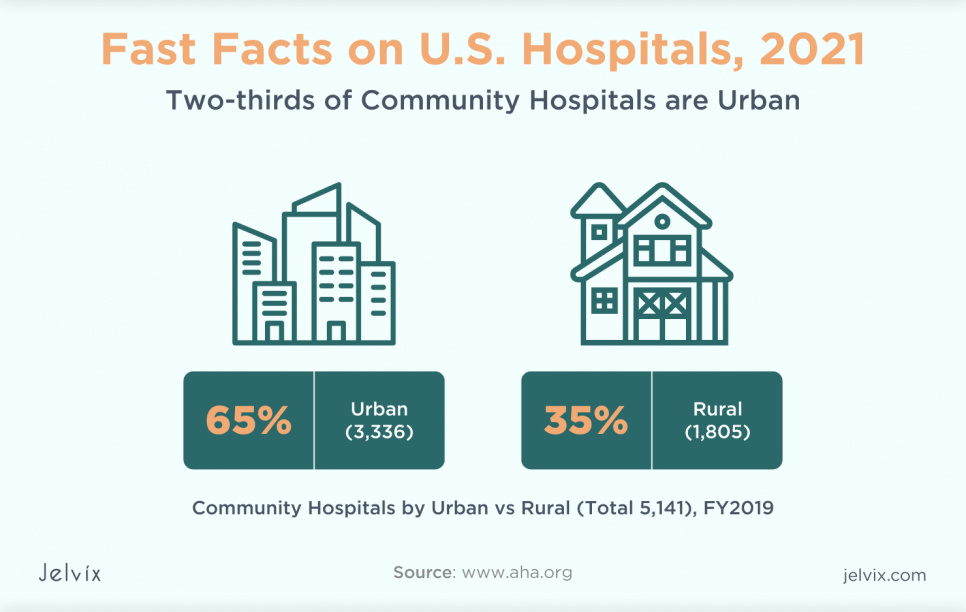
Even as non-COVID patients have already received the brunt of these inconveniences, COVID patients are now experiencing their inconveniences as they suffer from the virus. This leads to the dire reality that hospitals aren’t as abundant as one might assume. In fact, this shocking statistic from the American Hospital Association (AHA) shows that there are more hospitals in urban places in the U.S. than in rural areas:
This shows that while urban hospitals are hectic with tending to COVID patients, rural hospitals are spreading thin with rising cases. To make matters worse, even with the dreaded Delta variant originating from India, and spreading into countries like Great Britain, according to the American Medical Association (AMA), hospitals have already gotten their fair share of overcrowded facilities.
With limited resources, and high demand for more hospital staff, hospitals are already seeing the downward spiral of unpreparedness as a result of COVID-19. Though, the more dire situation is that as more COVID cases enter the hospitals, non-COVID cases are either sent elsewhere, postponed, or worse – turned away.
This can be physically, emotionally, and mentally draining for patients and hospital staff.
A Silver Lining?
The good news is, the health of a hospital doesn’t have to be in a state of crisis, not when there are lives to save. Believe it or not, hope for the healthcare industry may come from an unlike source: virtual reality (VR). With technology rising and evolving over the recent years, it’s no surprise to see the idea of taking part in virtual worlds become a reality.
Now, this may come as a shock to some spectators since normally, things like virtual reality have been reserved for recreational uses, such as video games and simulation. However, in the most recent years, VR has seeped into other industries, including:
- Architecture
- Education
- Engineering, AND
- Healthcare
Yes, even healthcare is starting to dabble with VR to treat patients, further their research on medicines and diagnosis, and even train for surgical procedures. Essentially, VR is no longer a novelty but rather something that can prove useful in even the most hectic and serious industry.
In fact, various companies and developers are testing and bringing forth new apps and VR products that can ease the burdens faced in the hospital world. According to a 2021 study done by Fortune Business Insights, the hospital industry invested approximately $1.56 billion in VR technology in 2018.
Furthermore, that number is expected to grow to $30.40 billion by 2026. So, how valuable is VR in the healthcare industry, and how are hospitals going about it? And, can VR be the ultimate saving grace for hospitals that are always slewed with too many patients, including many from the ongoing COVID-19 crisis?
This article will discuss the benefits and uses of VR through various case studies in hospital settings. Read on, and see how VR is working its technological magic in healthcare!
Define Virtual Reality In Healthcare
Virtual reality offers simulated scenarios that users can work in. In the healthcare industry, this can be beneficial, since more and more doctors and nurses are coming into the field, especially in these trying times.
But with that said, there are thorough investigations before VR can be implemented 100%. In fact, the healthcare industry has strict guidelines on how to operate and what products are viable to use when taking into account the safety and wellbeing of patients. According to the Centers for Disease Control and Prevention (CDC), the use of virtual reality in healthcare can benefit training in the following ways:
- Applying new skills in given scenarios;
- Assessing current skills to see if they’re still viable for use in real-world scenarios, AND;
- Improving said skills in a safe and controlled learning environment.
What can be learned and modified in VR simulations and training can be implemented in real-world scenarios, just as long as they’re safe and viable for patient care. Instead of leaving anything to chance when, say, operating on a patient, VR can help guide researchers, doctors, and nurses on what methods to take, how to do it, and when.
In this way, costly mistakes (i.e. accidental injuries during surgery, overdosage of hospital medications, etc.) can be avoided. In essence, VR simulations can help do the following:
- Limit traumas from various procedures like surgery
- Improve outcomes of said procedures
- Improve communications between patients and doctors
- Lower medical costs
Some of the most effective VR devices to date in the healthcare industry are head-mounted displays (much like popular VR sets such as the Oculus Rift, HTC Vive, etc.), haptic gloves (which are now used for surgery simulations), and smart glasses (like Google Glass).
The Benefits
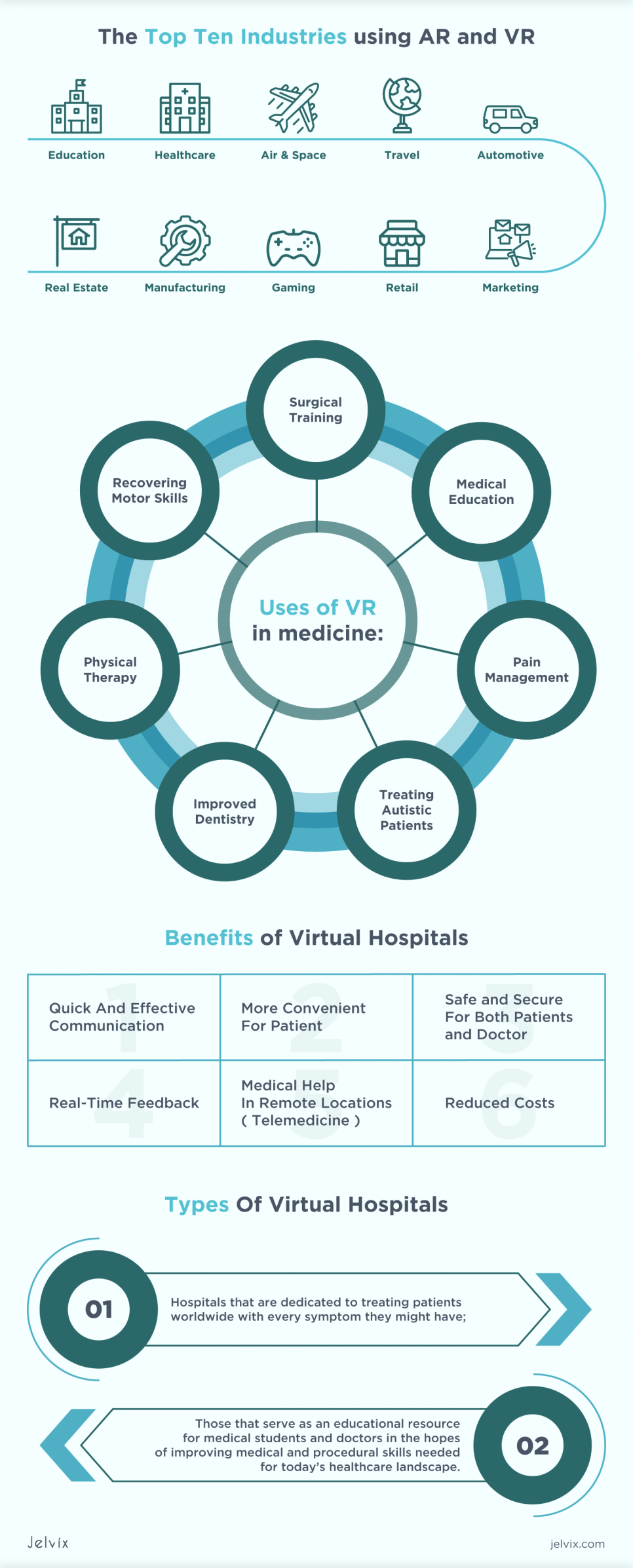
As we delve deeper into virtual reality in healthcare, we’ll now introduce you to the benefits of these proposed “virtual hospitals.” The benefits of using VR in hospitals go as follows:
Quick And Effective Communication
- Provider-to-patient collaboration is possible when doctors and or nurses can contact patients no matter where they are, and even offer consultations on the fly. Plus, patients can show doctors or nurses photos or videos of their symptoms from where they are, without having to rush to a hospital.
- Provider-to-provider collaboration is also possible when providers can transfer patient data to another provider and exchange clinical opinions with them. This collaboration can also be beneficial for training purposes in healthcare.
More Convenient For Patients
Patients will enjoy the convenience brought forth by VR technology. Instead of waiting to be seen at a physical facility, or turned away (which is treated as a last resort for healthcare facilities), patients will now have the option to be seen virtually by talking to a doctor from their mobile device through a healthcare app.
Plus, when trying to understand a diagnosis, a doctor can visually demonstrate to patients the recommended procedures and possible cures for their, say, cancer or disease.
Reduced Costs
With COVID-19, hospitals have already seen shortages in supplies, including exam gloves, face masks, hospital beds, etc. Since hospital beds and other supplies are needed for COVID patients, with VR, non-COVID patients can now have the option to stay at home and be seen by a licensed physician.
This move can cut hospital costs, and save facilities money and other assets needed for exams and treatment. Plus, it can save patients from having to pay expensive emergency room visits if it turns out that their symptoms weren’t severe to begin with. Either way, hospitals can rest easy with reduced costs, thanks to VR.
Read about the remote patient monitoring and implementation steps.
Case Studies
While virtual reality is about getting involved in simulated scenarios or learning something “up close,” VR in healthcare – or “virtual hospitals,” so to speak – can be different from its video game and recreational equivalents.
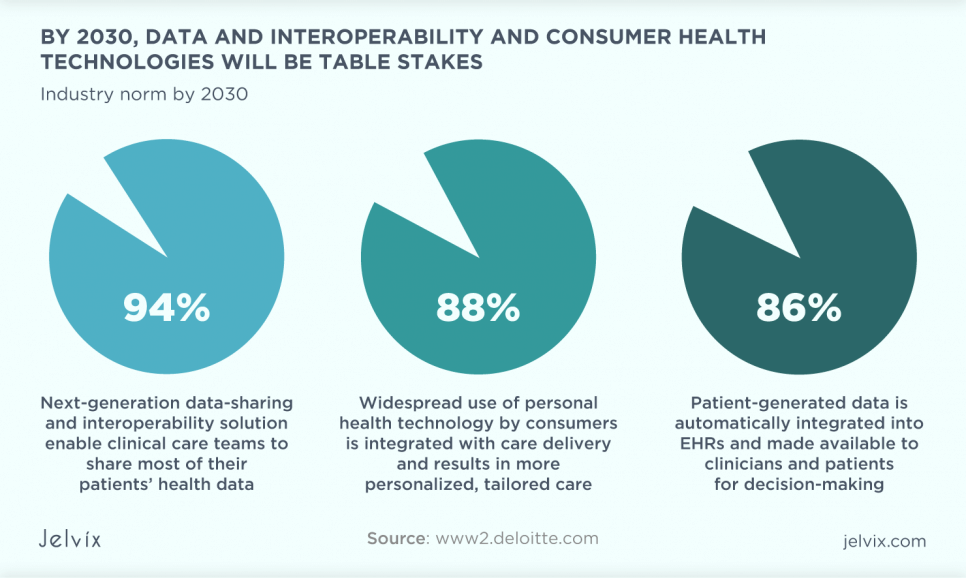
So far, VR can be a potential blessing for the healthcare industry. According to Deloitte Insights, virtual health has helped to improve the consumer experience, expand consumer access to clinicians, and improve clinical outcomes by 74%, among other things. With so many possibilities, it isn’t hard to discover that VR can do wonders for both doctors and patients.
With that said, VR can be seen as two types of virtual hospitals:
- Hospitals that are dedicated to treating patients worldwide with anything and every symptom that they might have, AND
- Those that serve as an educational resource for medical students and doctors in the hopes of improving medical and procedural skills needed to today’s healthcare landscape.
Since patients are a top priority for hospitals, doctors and nurses can use VR to help better treat sick people, while offering professional-looking diagnoses to those who had suffered an injury or might have a type of cancer or disease. As for the patients themselves can use VR to learn more about their own bodies and seek advice from medical staff 24/7.
So, now that you have begun to understand the definition and benefits of virtual hospitals, it’s time to delve deeper into this discussion by learning about some of the most successful case studies from the healthcare industry involving the use of VR.
While many of the case studies that we’ll now look into may seem too good to be true, understand that said cases come from the idea that perhaps VR can be beneficial in learning about something, rather than finding a quick and easy solution to a diagnosis.
And, while there are many other success stories involving virtual hospitals that might not be listed in this article, the following case studies will give you a sense of hope in VR aiding the ever-evolving industry. With that in mind, let us explore these case studies:
Atrium Health
Atrium Health is one significant example of being a virtual hospital. In this virtual hospital, there are two levels, or “floors”:
The first floor serves as an observation unit, where doctors and medical professionals can monitor patients. For example, COVID-19-positive patients are admitted to the first floor of this virtual hospital. They’re given digital tools to monitor their temperature, blood pressure, oxygen levels, and pulse.
Using a Bluetooth-enabled device, data from their monitored points can be transferred to a smartphone app from the health system’s IT department. As a result, the data can be fed into the patient’s EMR (Electronic Health Record), thus fully integrating into the patient’s continued healthcare needs.
The operations done in the “first-floor” are done by a team of clinicians, who monitor the data and check on patients daily back at Atrium Health’s call center.
As the second floor, that part of the virtual hospital is for patients who need more intensive care. While patients here have the same home monitoring tools as first-floor patients, they tend to receive more intensive management, along with frequent check-ins. Intensive management involves community-based paramedics visiting patient homes to administer any or all of the following:
- Breathing treatments
- EKGs
- IV antibiotics
- IV fluids, AND
- Other medical interventions that these patients might need
As a result of this arrangement, Atrium Health was able to control many patients that were in the hospital. Within 10 months of operation, the virtual hospital was able to administer the right treatment for COVID patients, which saved them about 500 hospital days that would have been required for hospitalized patients.
In addition, this arrangement had saved many families from being separated (physically, emotionally, and mentally) from each other during the quarantine phase of one’s COVID-19 diagnosis.
Joint Virtual Care Center
This next case study comes from the University of New England (UNE). As an experiment, the university wondered how resilient communities could be built with virtual care. Eventually, students and researchers came up with the New England Virtual Health Network (NEViHN), which is an innovative education and healthcare network dedicated to bringing virtual health to communities no matter where they are.
Again, the two types of virtual hospitals apply to this case study. NEViHN offers in-place healthcare for patients, along with in-place learning for all future UNE medicine and health students in New England’s North West region (which covers almost 10 million hectares of land, and houses over 18,500,001 people).
While this virtual hospital was proven experimental for the people involved, it proved to be something useful for real-world purposes.
Once the COVID-19 pandemic had hit, NEViHN was called to assist the Armidale Hospital emergency department in Australia in opening a virtual emergency room for the incoming waves of COVID patients and cases.
At the time, the hospital was in need of a way to tend to all of their patients – COVID and non-COVID patients. The last thing the hospital wanted was to turn people away, because there were no hospital beds or resources available.
With NEViHN, patients have the option of receiving a tablet (or installing a mobile app on their smartphones), along with any devices that match their condition. For example, if a patient had something like blood pressure symptoms, they were given a blood pressure monitor, among other things.
In addition, patients are able to use NEViHN’s features to regularly attend scheduled virtual visits. As a result, the burden on the hospital was lessened, thanks to NEViHN’s convenient services and functions for patients, no matter their diagnosis, as the facility braced for waves and waves of COVID patients.
Mercy Virtual
Another case study to consider is the Mercy Virtual Care Center, which started operations in Chesterfield, Missouri in 2015.
Considered the world’s first facility dedicated to virtual hospital – or telehealth, so to speak – Mercy Virtual the Virtual Care Center is devoted to offering virtual care services to patients across participating states in the U.S.
Having originated in a four-story, 125,000-square-foot building in Chesterfield, the virtual care program was hailed as a telehealth godsend that provided various healthcare services for patients. With that said, the virtual hospital provides 4 core telehealth programs to date:
vEngagement is a core telehealth program provided by Mercy Virtual, which uses biometric monitoring and interactive technologies to help various patients with varying diagnoses.
In this program, the center’s team monitors and helps patients with even chronic symptoms. All patients need is a tablet, so that they can see their monitored blood pressure, their weight, and their pulse.
vHospitalist supports real-time assessment for patients. The program can also order specific tests and therapies, while handling patient admissions and transfers.
vICU understands that Intensive Care Units are hectic, when it comes to patient emergencies and COVID cases. With that said, this program in Mercy Virtual allows doctors and nurses to remotely monitor patients’ vital signs through advanced camera technology.
With highly sensitive two-way cameras, the Internet of Things (IoTs), and care navigation technologies, the program is able to monitor patients in many ways.
vStroke understands how serious strokes can be. Stroke can be life-threatening to many patients. That’s why Mercy Virtual came up with vStroke, which allows stroke patients to receive an immediate virtual assessment from a certified neurologist. Then, using a two-way camera, the neurologist can examine a patient, and then record it in the patient’s electronic health record.
Thus, Mercy Virtual serves well as a central freestanding facility staffed with healthcare professionals on the ready.
Conclusion
Ultimately, virtual hospitals are a godsend for hospitals and related facilities. What was once reserved for leisurely activities like video games, VR is now being used in medicine and healthcare.
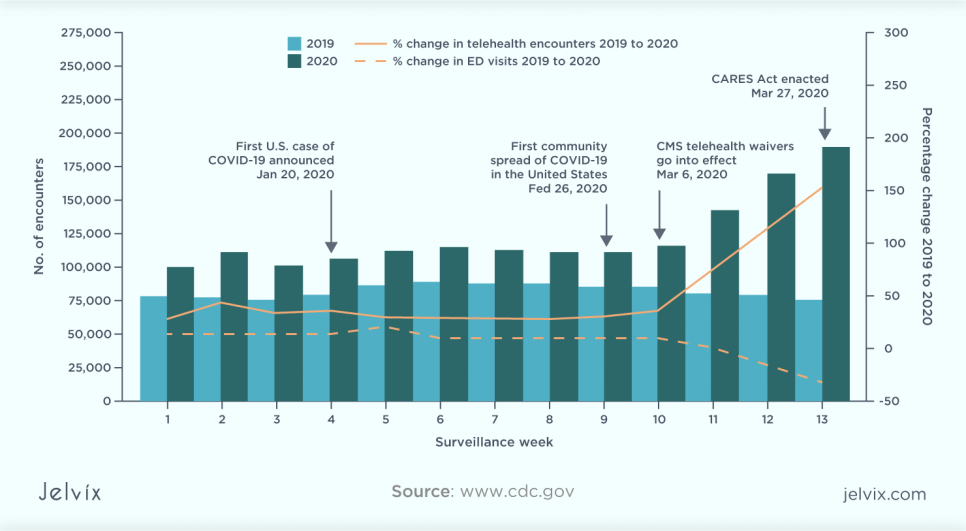
According to AHA, with rises in COVID cases and a 14.5% increase in total hospital expenses, virtual reality is now moving into patient care and training. As you saw by the cases discussed, VR has already made strides in the healthcare industry. As the case studies show, the VR healthcare market is here to stay.
Virtual hospitals are revolutionizing the healthcare landscape by providing remote, efficient, and comprehensive care, leveraging the latest in virtual reality technology. To understand how these innovative solutions are designed and the impact they have on patient care, Jelvix’s Healthcare software development services offer a deep dive into the creation and implementation of virtual healthcare systems.
Do you have a promising idea on how to use VR in your business? Share your vision with our team, and we will build innovative software that will bring profit now.
Jenny Divine is a blog writer at LastMinuteWriting.com and Coursework writing services UK. She is also an editor at Gumessays. As a marketing specialist, she helps companies improve their marketing strategies and concepts. As a content writer, she writes articles about different aspects of marketing, along with trendy tech products and coding. In her spare time, she likes to read about business practices and economics.
Need a qualified team?
Access the talent pool, start digital transformation now.