The diabetes app market looks crowded, but in reality, most platforms face the same hidden constraint. They were built fast, as MVPs, with monolithic designs optimized for one condition, one workflow, and one integration.
When the time comes to expand into adjacent conditions like hypertension, obesity, or COPD, many diabetes solutions stall. Adding just one new device, payer API, or EHR connection often means months of refactoring. For product leaders, that translates into slower velocity, higher burn, and missed opportunities. For investors and payers, it raises red flags about scalability and ROI.
The underlying reason is architecture debt. It is a form of technical debt rooted in early design shortcuts. In chronic care SaaS, this debt shows up as tightly coupled device and EHR pipelines, brittle data flows that break under small changes, and compliance features bolted on after launch.
While these decisions speed up the initial release, they trap platforms in narrow use cases and make true scaling far more difficult. Overcoming these limitations is part of a broader journey of digital transformation solutions, where platforms evolve from MVP tools into scalable ecosystems.
If you want to build a diabetes management app that can scale freely, read this report. It explains why diabetes apps carry architectural debt, how it hinders growth, and what leaders can do to address it.
All findings in this report are based on open-source research and Jelvix analysis of popular diabetes management and logging apps, RPM platforms, virtual diabetes clinics, and multi-condition chronic care platforms. Sources include developer documentation, HL7/FHIR guides, app store reviews, and industry reports. No sensitive or client data was used. Insights reflect patterns visible in the market and Jelvix’s experience helping digital health companies modernize their platforms.
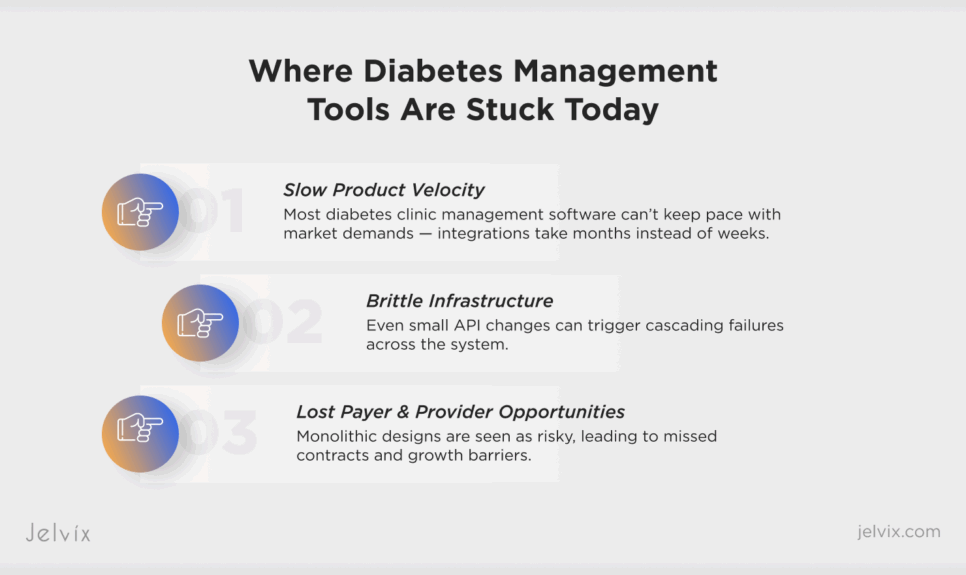
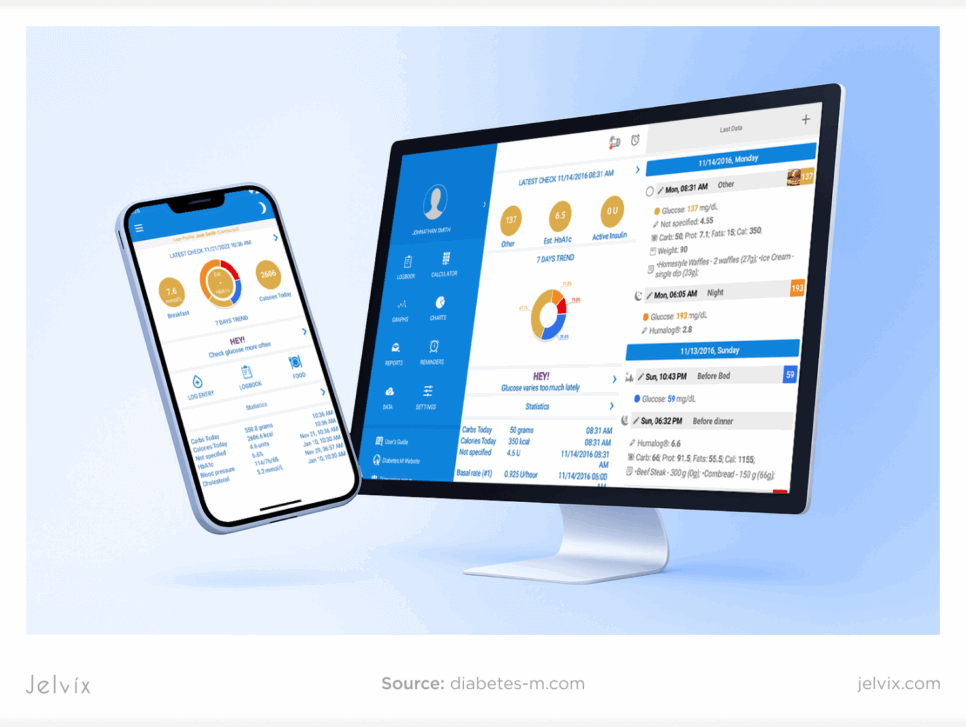
Where Diabetes Management Tools Are Stuck Today
A public analysis of leading diabetes solutions, including logging apps, CGM dashboards, RPM solutions, and virtual clinics, reveals a consistent pattern. Most platforms are still operating on monolithic MVP architectures.
A review of developer documentation, API references, and app store feedback suggests that the majority of digital health tools for diabetes still rely on early-stage “prototype-style” designs. These architectures were built for speed and market entry — often monolithic, hard-coded, and focused on a single condition — but now limit scalability and maintainability.
This perspective aligns with academic research on healthcare SaaS. Academic reviews highlight the persistent reliance on monolithic cloud systems in healthcare, and studies of software architecture debt confirm that tightly coupled systems degrade maintainability and scalability over time. For companies working in healthcare software development, this illustrates how architectural decisions directly shape long-term business performance.
Even when vendors attempt modernization, the transition is complex. For example, BD has publicly discussed the challenges of scaling its digital health and AI solutions in healthcare, noting issues such as fragmented systems, inconsistent data, and interoperability hurdles when integrating new digital tools into legacy infrastructures. These industry experiences illustrate why many platforms remain stuck between the MVP stage and full scalability — a gap that demands careful planning around system integration and architectural transformation.
Struggling with disconnected systems? Discover how system integration can unify your workflows and boost efficiency.
Slow Product Velocity
Most diabetes clinic management software struggles to move at the pace the market demands. Integrating a new CGM or RPM device, for example, often takes 12–16 weeks on monolithic systems. At the same time, competitors with modular architectures can roll out two or three new integrations. This lag reduces a platform’s ability to compete for payer contracts, where rapid expansion into covered devices and conditions is a differentiator.
Brittle Infrastructure
In tightly coupled architectures, even a small change can have outsized consequences. A CGM vendor updating its API version, or an EHR switching authentication methods, can ripple across the entire system. Instead of a smooth patch, teams end up with cascading failures in data ingestion, visualization, or reporting modules. These breakages translate into emergency sprints, downtime, and higher engineering costs, which undermine trust with providers and patients.
Lost Payer and Provider Opportunities
Health systems and insurers increasingly demand multi-condition readiness and robust interoperability in their RFPs. A diabetes app that cannot easily integrate hypertension data or fails to produce standardized outcome reports (e.g., diabetes technology leveraging the FHIR standard) risks being excluded from long-term contracts. NHS pilots and U.S. payers are especially clear about scalability and ROI being prerequisites. Platforms stuck in monolithic designs often lose out, not because of clinical shortcomings, but because their technical debt signals risk to buyers.
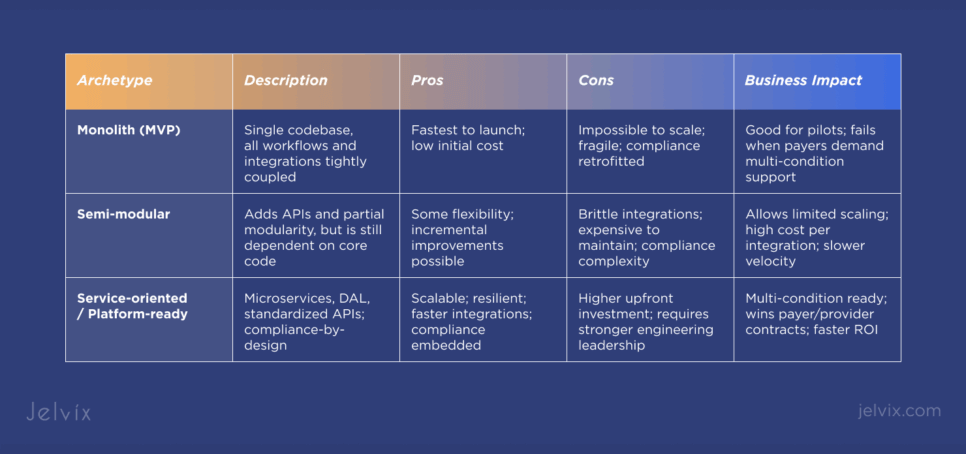
Common Architecture Archetypes in Diabetes SaaS
Not all digital diabetes platforms are stuck at the same stage. From our analysis of public developer docs, APIs, and industry case studies, three main archetypes emerge. Each represents a different level of architectural maturity, and it directly impacts scalability, compliance, and business performance. Understanding these patterns is essential for anyone planning EHR implementation or broader system upgrades in chronic care platforms.
Want to improve chronic disease management? Here’s how Jelvix built a digital solution that unifies care, boosts engagement, and scales across conditions.
Monolith (MVP Stage)
The majority of diabetes management tools start here. A single codebase handles everything: device connections, patient workflows, reporting, and compliance features. This design is fast to launch, but quickly becomes a bottleneck. Adding a new CGM or supporting a second condition often means rebuilding core components from scratch.
Semi-Modular (Partial APIs, Still Brittle)
Some platforms evolve toward modularity, introducing APIs for devices or EHRs. However, integrations remain tightly coupled, and workflows often break when one module changes. This stage reduces short-term pain but leads to high maintenance costs as the platform grows. Many teams at this stage begin exploring a FHIR interoperability standard or healthcare API integration to stabilize data exchange. However, without an architectural redesign, even standards-based integrations can remain brittle.
Service-Oriented / Platform-Ready (Scalable, Compliance-Ready)
The most advanced diabetes SaaS platforms adopt modular, service-oriented architectures. They use microservices, Data Aggregation Layers (DALs), and standardized APIs to decouple device ingestion, clinical workflows, and reporting. Compliance is built in, not bolted on. This approach supports multi-condition expansion, rapid integration, and payer-grade reliability.
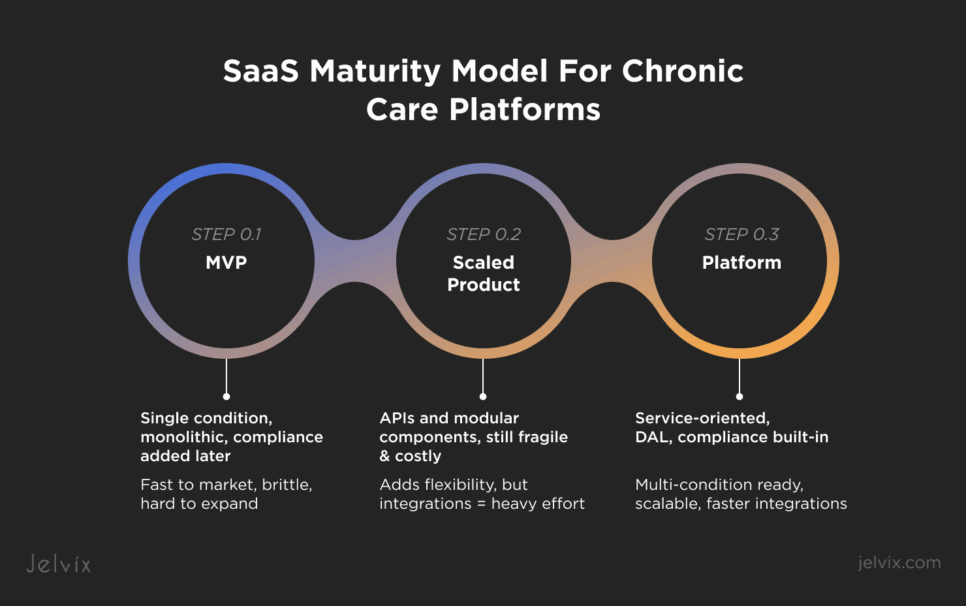
The SaaS Maturity Model for Chronic Care Platforms
Architecture debt is not random. Most diabetes platforms follow a predictable evolution. Based on our analysis, the journey from MVP to a scalable platform can be described in three stages.
Stage 1: MVP
This is the launch stage, where speed to market outweighs scalability.
- Characteristics: Single condition only, hard-coded device flows, compliance added after launch.
- Strengths: Fast time-to-market, suitable for pilots or proof-of-concepts.
- Weaknesses: Every new integration requires deep refactoring. It is impossible to expand beyond diabetes without breaking workflows.
- Business Impact: Suitable for early adoption, but stalls when payers or NHS contracts require multi-condition support.
Stage 2: Scaled Product
This is the transitional stage, where teams start adding APIs but struggle with fragility and cost.
- Characteristics: APIs and modular components begin to appear, but remain fragile and expensive to maintain. Integrations are project-based rather than standardized.
- Strengths: Adds some flexibility and reduces bottlenecks compared to monoliths.
- Weaknesses: Each new device or EHR still demands heavy engineering effort; compliance updates slow down the roadmap.
- Business Impact: Platforms at this stage can expand cautiously, albeit at a high cost and with limited speed, creating vulnerability to faster competitors.
Stage 3: Platform
This is the maturity stage, where platforms evolve into scalable ecosystems with compliance built in.
- Characteristics: Service-oriented architecture with modular integration frameworks, Data Aggregation Layer (DAL), and compliance built into workflows. Standardized APIs enable smooth device and EHR connections.
- Strengths: Scalable, resilient, multi-condition ready. Integrations are measured in weeks rather than months. Compliance shifts from drag to enabler.
- Business Impact: Positioned to win payer and provider contracts, expand into multi-condition ecosystems, and deliver stronger ROI to investors.
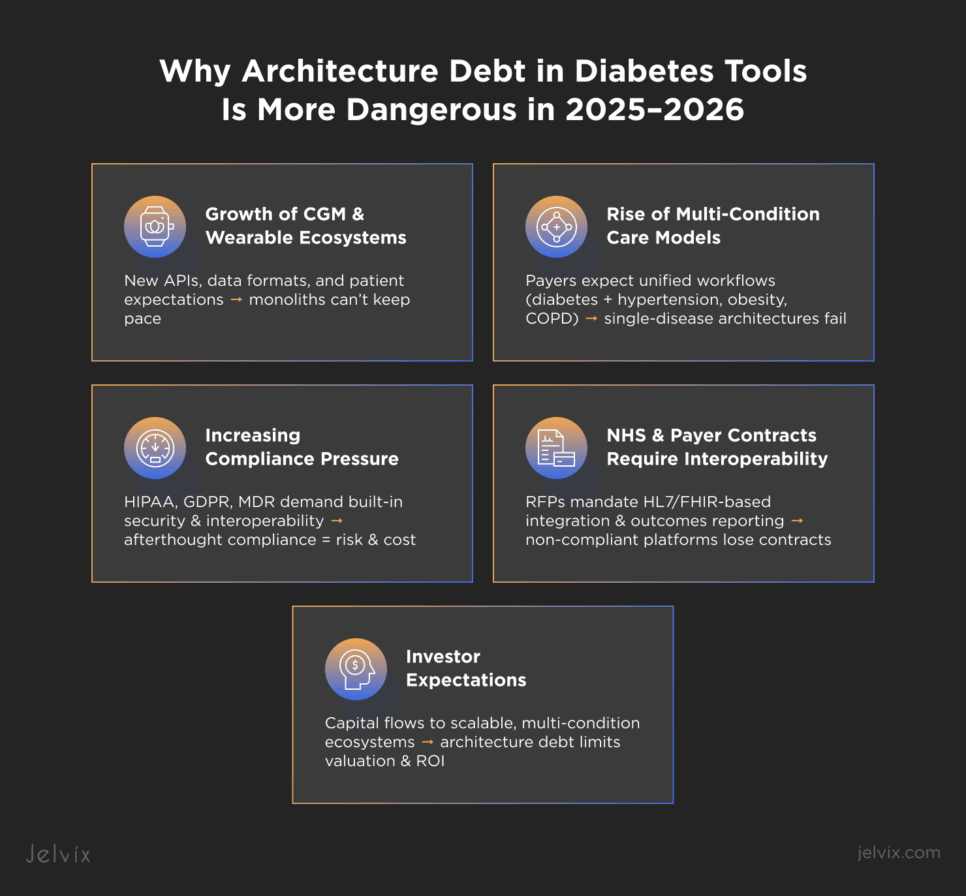
Why Architecture Debt in Diabetes Tools Is More Dangerous in 2025 – 2026
The risks of architecture debt intensify as the digital health transformation accelerates. Several shifts make monolithic diabetes solutions especially vulnerable over the next two years.
Growth of CGM and Wearable Ecosystems
New generations of continuous glucose monitors (Dexcom G7, Abbott Libre 3) and consumer wearables (Fitbit, Apple Watch) are being rapidly adopted worldwide. Each device brings new APIs, new data formats, and higher patient expectations for seamless integration. Platforms without modular frameworks will struggle to keep up with the pace of diabetes technology innovation.
Rise of Multi-Condition Care Models
Diabetes rarely exists in isolation. Payers and providers increasingly expect platforms to address comorbidities like hypertension, obesity, and COPD in unified workflows. Monolithic architectures built around a single disease state cannot support the complexity of multi-condition care without major rework.
Increasing Compliance and Regulatory Pressure
Global regulations are tightening. HIPAA in the U.S., GDPR in Europe, and MDR across the EU all demand higher levels of security, interoperability, and auditability. Platforms that treat compliance as an afterthought face slower releases, higher legal risk, and escalating costs as rules evolve.
NHS and Payer Contracts Demand Interoperability
Procurement requirements have shifted. Both NHS pilots in Europe and payer contracts in the U.S. now mandate proof of interoperability and outcomes reporting, often using HL7/FHIR standards. That’s why building toward clinical interoperability has become a prerequisite for reimbursement readiness and long-term contracts.
Investor Expectations for Fast, Scalable Growth
Venture and strategic investors no longer reward single-condition plays. They want platforms that can scale across multiple chronic conditions, adapt quickly through SaaS integration, and demonstrate a clear ROI. Architecture debt signals fragility and limits valuation, which is a growing concern in an investment climate where capital is flowing toward scalable digital diabetes management ecosystems.
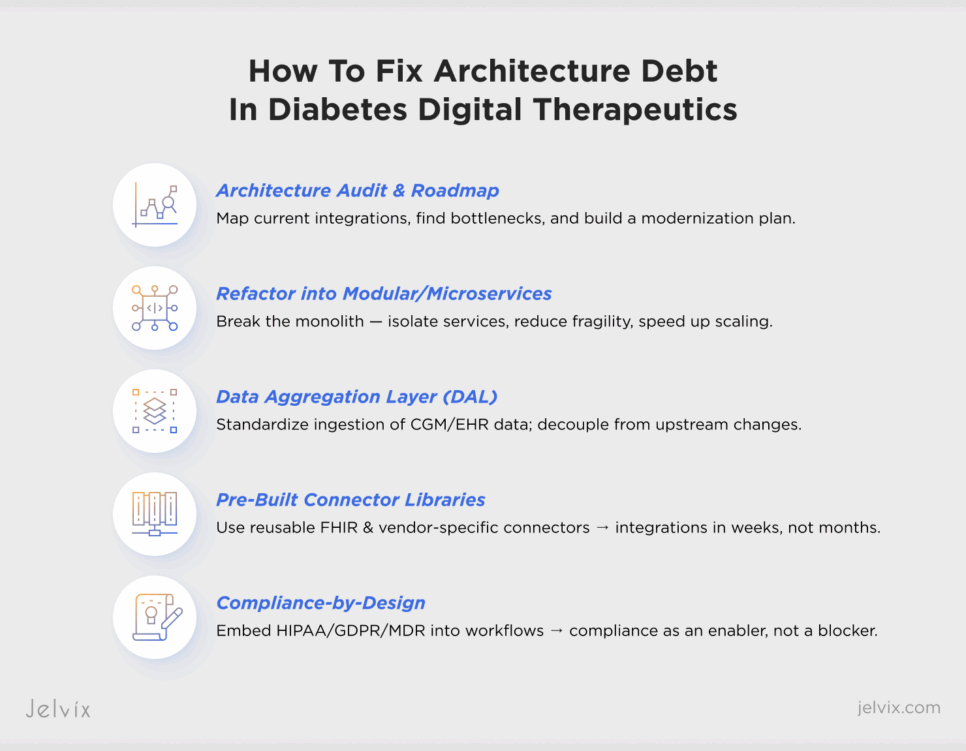
How to Fix Architecture Debt in Diabetes Digital Therapeutics: 5 Practical Approaches
Overcoming architecture debt means taking deliberate steps to decouple, modularize, and future-proof the platform. Product leaders can prioritize the five practical moves we described below.
1. Architecture Audit and Roadmap
Start by mapping the current state. An audit identifies where integrations are tightly coupled, where compliance is retrofitted, and where technical bottlenecks slow down delivery. The output is a roadmap that balances quick wins (e.g., stabilizing brittle APIs) with long-term modernization. For teams building diabetes management software or broader digital health transformation solutions, this step provides clarity on how to move from MVP fragility to scalable ecosystems.
2. Refactoring into Modular or Microservice Designs
Breaking the monolith into services reduces fragility. Even partial refactoring, such as isolating data ingestion, analytics, or patient engagement modules, can dramatically cut integration timelines. Full microservice migration, while costlier upfront, provides the resilience and scalability needed for multi-condition care.
3. Implementing a Data Aggregation Layer (DAL)
A DAL acts as a buffer between external devices/EHRs and the core platform. Instead of hard-coding each CGM or payer API, the DAL standardizes data ingestion, making the system more resilient to upstream changes. This also accelerates the onboarding of new devices and partners through healthcare API integration, which is critical for providers, payers, and patients relying on digital therapeutics diabetes tools in real-time.
4. Pre-Built Connector Libraries for EHRs and CGMs
Reusable connectors (FHIR-based for EHRs and vendor-specific for CGMs) facilitate integration by shifting it from bespoke projects to plug-and-play. With connector libraries, a new device integration can take weeks instead of months, which is a crucial advantage when payers or providers demand rapid expansion. Using standards like Cerner FHIR and Epic integration can help ensure long-term interoperability and reduce the risk of compliance delays.
5. Compliance-by-Design Frameworks
Instead of bolting on HIPAA, GDPR, or MDR requirements after the fact, embed them into workflows and data flows from the start. Automated audit logs, standardized consent management, and encryption defaults turn compliance from a release blocker into an enabler of trust.
Case-Inspired Insights for Improving Diabetes Management Software
Real-world experience shows how architectural maturity directly impacts scalability and cost. The following anonymized patterns illustrate common outcomes across diabetes SaaS platforms.
Example 1: MVP-Stage Platform Failed to Add Hypertension
A diabetes app launched quickly on a monolithic codebase and won early traction with patients and providers. When the team attempted to add hypertension management as a second module, they discovered that device data pipelines, workflows, and reporting were all hard-coded around diabetes. The cost and timeline of refactoring were so high that the expansion project was abandoned, leaving the platform stuck as a single-condition tool while competitors moved ahead.
Example 2: Semi-Modular App Doubled Costs Per Integration
Another vendor had evolved past a pure monolith and offered APIs for select device integrations. However, because the APIs were brittle and inconsistently documented, every new integration required significant custom engineering. Instead of getting faster with scale, the average cost per integration nearly doubled. The result was slower product velocity for its diabetes management app, rising operational expenses, and mounting frustration from provider partners.
Example 3: Platform-Ready Design Cut Integration Time from 16 to 6 Weeks
In contrast, a diabetes SaaS platform that invested early in service-oriented design achieved rapid scalability. By deploying a Data Aggregation Layer (DAL) and pre-built connector libraries, the team reduced average device integration timelines from 16 weeks to just 6.
Compliance frameworks were embedded from the start, allowing the platform to meet payer and NHS requirements without re-engineering. This readiness positioned the company to win multi-condition contracts and demonstrate faster ROI to investors.
Jelvix Expert Guidance To Help Businesses Avoid Technical Debt
At Jelvix, we’ve seen the full spectrum of diabetes and chronic care platforms, ranging from monolithic MVPs stuck in single-condition loops to service-oriented ecosystems that win payer contracts. The difference comes down to how teams manage or even escape their architecture debt.
Lessons from SaaS Integration Projects
Our work with digital health platforms shows a consistent pattern. The sooner a company invests in modular architecture, the faster it unlocks multi-condition growth. Teams that delay often face spiraling costs, emergency refactors, and lost contracts when expansion becomes urgent.
Our Services
We help chronic care platforms move from fragile MVPs to scalable ecosystems by addressing both the technical and regulatory layers that determine growth.
Architecture Audits and Roadmaps
Our audits go beyond code review. We map how your current data pipelines, workflows, and compliance layers interact, identifying brittle integrations and performance bottlenecks. The roadmap we deliver shows not only where to refactor but also how to prioritize changes for quick wins versus long-term modernization.
Data Aggregation Layers (DALs)
Instead of coding a device and SaaS integration directly into the core platform, we build a DAL that standardizes ingestion. This makes your system resilient to upstream changes, for example, when a CGM vendor updates its API, the DAL absorbs the change without breaking downstream workflows. As a result, you get integrations that are faster to add and cheaper to maintain.
Pre-Built Connector Libraries
Jelvix maintains libraries of reusable connectors for major CGMs (Dexcom, Abbott, Medtronic), EHRs (FHIR, HL7), and RPM platforms. By deploying these, our clients cut integration time from months to weeks. This is especially valuable for payer or NHS contracts where multi-device coverage is a requirement.
Compliance-by-Design Frameworks
We design workflows with HIPAA, GDPR, and MDR compliance built in, from encryption and consent management to automated audit logs. This reduces regulatory risk and accelerates product releases, since compliance is no longer a blocker retrofitted at the last stage.
Accelerating Scaling and Winning Contracts
By reducing integration timelines, stabilizing data flows, and embedding compliance, we help digital health companies scale faster and prove ROI to investors and payers. For diabetes platforms preparing for NHS pilots or payer negotiations, this architectural readiness is a decisive competitive advantage.
Summing Up
Diabetes SaaS platforms have proven their clinical value, but most remain trapped by architectural debt. Monolithic MVPs, brittle integrations, and compliance drag prevent them from evolving into the multi-condition ecosystems that payers, providers, and investors now expect.
The lesson is clear: architecture debt is a growth barrier, while modular frameworks are growth enablers. Platforms that invest in decoupling data flows, standardizing integrations, and embedding compliance position themselves not just to survive, but to lead in the chronic care market.
Think of the journey as a four-step process that starts with auditing your current architecture, continues with refactoring brittle components, moves into integrating standardized frameworks and connectors, and ultimately positions the platform to scale confidently into multi-condition care supported by diabetes management tools.
At Jelvix, we help digital health companies follow this path by guiding platforms from fragile platforms to multi-condition ecosystems ready for NHS and payer demands. If you’re preparing for expansion or investor due diligence, now is the right time to act.
Book an architecture readiness assessment with Jelvix experts today and turn your architecture into a competitive advantage tomorrow.
Want to deliver a better patient experience?
Partner with Jelvix to unify data flows and future-proof your diabetes platform.